Abstract
Pre-clinical research and development relies heavily upon translationally valid models of disease. A major difficulty in understanding the biology of, and developing treatments for, rare disease is the lack of animal models. It is important that these models not only recapitulate the presentation of the disease in humans, but also that they share functionally equivalent underlying genetic causes. Nonhuman primates share physiological, anatomical, and behavioral similarities with humans resulting from close evolutionary relationships and high genetic homology. As the post-genomic era develops and next generation sequencing allows for the resequencing and screening of large populations of research animals, naturally occurring genetic variation in nonhuman primates with clinically relevant phenotypes is regularly emerging. Here we review nonhuman primate models of multiple rare genetic diseases with a focus on the similarities and differences in manifestation and etiologies across species. We discuss how these models are being developed and how they can offer new tools and opportunities for researchers interested in exploring novel therapeutics for these and other genetic diseases. Modeling human genetic diseases in translationally relevant nonhuman primates presents new prospects for development of therapeutics and a better understanding of rare diseases. The post-genomic era offers the opportunity for the discovery and further development of more models like those discussed here.
Similar content being viewed by others
Introduction
Understanding the causes of rare genetic disease and developing appropriate evidenced-based treatment strategies are ongoing challenges for scientists and clinicians. Rare diseases occur, by definition, infrequently, but with an estimated 10,000 unique rare diseases their overall impact is substantial [1]. The challenges and long-lasting impacts that they present for the patients, family members, and communities can be overwhelming. Uncovering the genetic basis and molecular mechanisms of these diseases are not only important for developing effective disease treatments, but also provide opportunities to better understand human biology and fundamental processes underlying human health and development.
Animal models are important tools for the study of human genetic disease for many reasons, not the least of which is the ability to study disease progression with great control in the laboratory. This is a necessary and important precondition for understanding analogous aspects of human biology and the prevention, etiologic description, or treatment of disease. The first recognition of the processes of inheritance and developmental pattern formation occurred from research with laboratory animals [2, 3]. The models are only useful and valid, however, with a comparative (across species) understanding of genotypes, phenotypes, and crucially, the relation between them. Translational studies require nonhuman models for a variety of reasons: for elucidating genetic causation or contribution to disease or normative phenotype, for understanding interactions between genetic or epigenetic factors and disease progression, for describing genotypic contributors to pharmaceutical effectiveness or the efficacy of other treatments, and for gene editing and therapy.
Among the most important considerations is the model species chosen for study. As our closest living relatives, nonhuman primates (NHPs) are especially critical research surrogates, and this review highlights new findings and directions in NHP modeling, specifically in the genetics of disease. Phylogenetic affinities, however, are only rarely the final arbiter regarding species chosen for research. Although humans are primates, there are other important, and far more widely-used, nonhuman animal models outside this order. Indeed, it has been estimated that only 0.28% of animals used in research are nonhuman primates [4]. Primates are much more expensive animal models to develop and maintain compared to other laboratory species due to their unique husbandry requirements, limited numbers, long generation time, and ethical concerns.
Non-Primate models of disease
Although examples of animal models of disease have historically included numerous and diverse mammalian and non-mammalian taxa, the use of rodents has increased for many decades and for obvious reasons. Common laboratory rodents (mice, rats, etc.) are small, with short generation times, and are easily maintained and bred in the laboratory. Certain manipulations, including the production, maintenance, and use of specific genetic strains and the productions of particular variations, are often straightforward, allowing exquisite control of variables. This includes the development of “humanized” rodents with genes, cells, or tissue grafted from its namesake [5]. Also, their phylogenetic relationship to primates is not especially distant relative to other well-studied laboratory organisms such as zebrafish and Drosophila [6].
A detailed look at rodent genetic models is beyond the scope of this review. In short, much is known about rodents, and their contribution to genetically-focused biomedical advances are considerable [reviewed in 7, 8], particularly in their utility for genetic manipulation and rapid breeding. In some cases, however, the very characteristics that help make common laboratory rodents ubiquitous in experimental settings are the ones that most clearly delineate limitations as models for human beings. Their small size can present difficulties regarding the procedures that can be performed and/or translational interpretation; for example, low blood volumes and diminutive organs in rodents limit gene therapeutic and surgical approaches to pathologies such as hemophilia and retinal degeneration [9]. Small size is also coupled with a litany of differences in physiology and metabolism [10, 11]. Excepting outbred and wild strains, genetic disease investigations often require a priori hypotheses and manufactured variation, and are highly targeted, not encompassing the normal, associated variation that characterizes human population [12]. This tight control over variation offers power in experimental design, but lacks the context of inter-individual variation seen in human clinical cases.
A number of larger, non-primate mammalian models have been developed including sheep, pig, cat, and dog, often during the process of line breeding and other selective husbandry practices. While more difficult and costly to house and breed when compared to rodents, their advantages include larger organ sizes, tissues that are more easily accessible, larger blood volumes, and in some cases otherwise more humanlike anatomy or physiology. In addition, they can easily be examined as individuals with varied genotypes, phenotypes, clinical histories, prognoses, and treatment options, and examined over long durations, as are human patients [9]. In the case of domestic animals, a large number are potentially available for screening of genetic variations associated with human pathology. For example, sheep models exist for a wide range of inherited medical conditions, including visual disorders such as heritable cataracts and achromatopsia, blood and connective tissue disorders, nervous system disorders such as Batten disease, and many others [13]. The discovery and investigation of various clinical conditions in dogs is facilitated by the fact that millions of companion animals are closely monitored by their owners and regularly seen by veterinarians, providing opportunity to identify various disorders [14].
Nonhuman primate models of disease
Non-primates are, at the end of the day, non-primates. Members of the Order Primates share a last common ancestor varyingly estimated to have lived between approximately 65 and 80 million years ago [15,16,17,18,19,20] with New World monkeys diverging 40–50 million years ago, Old World monkeys 30–35 million years ago, the ape radiation 20–25 million years ago, and the separation of the African ape/human lineage from Asian apes, 15–20 million years ago. While work has been conducted with species throughout the order, the most common NHP translational genetic model is presently the rhesus macaque (Macaca mulatta), a medium-sized (adults ~ 6–12 kg) Old World monkey whose genome was first reported in 2007 [21] and updated most recently in 2020 [22]. Well characterized breeding colonies of specific pathogen free rhesus macaques are maintained in the US. Work with this species is supported by a publically-available, searchable, annotated database (The Macaque Genotype and Phenotype Resource, or mGAP) on genetic variants and known disease association [23]. Additional Old World monkeys important in translational genomics research include, but are not limited to, other species of macaques, e.g. cynomolgus macaques (M. fascicularis) and Japanese macaques (M. fuscata) [24], baboons (Papio sp.) [25], and vervet (African green) monkeys (Chlorocebus aethiops sabaeus) [26]. Among New World monkeys there is growing interest in common marmosets (Callithrix jacchus), small simians (adults ~ 300 g) which have a published whole draft genome [27] and newer annotated reference assemblies. Marmosets are notable for litters of 2–4 offspring that are hematopoietic chimeras, as outgroups for catarrhine evolutionary studies, and for their potential in genetic engineering studies [28, 29]. Regarding prosimians an ongoing initiative is investigating the translational potential of mouse lemurs (Microcebus spp.), which—with their small size (30–60 g) and rapid maturation (sexually mature at 6–8 months)—present some logistical advantages similar to rodents, but with some added advantages of primate physiology [30]. Each model has its strengths and limitations, and the further development of new or underutilized model species will undoubtedly prove valuable.
While all of the primate genetic models subsequently discussed in this review occur in macaques, it is important to recognize that large-scale sequencing of vervet monkeys, baboons, and marmosets would also be expected to identify functionally significant mutations and lead to new genetic models in those species. Each primate species carries its own unique array of functionally significant mutations. The current emphasis on macaques, and in particular rhesus macaques, results largely from the significant support by the NIH for expansion of breeding programs over the past several decades, especially in response to the need for macaques for HIV/AIDS studies.
NHPs, collectively, share more genotypic and phenotypic identity with humans than any other model organisms, as primates have a number of derived features, relevant to disease modeling, that differ either qualitatively or quantitatively from other mammals. Quite striking are synapomorphies related to vision and the tactile sense [31]. Eyes are large and located anteriorly, on the front of the face, providing extensive overlap of visual fields. A bony strut (postorbital bar, rare in other mammals) lateral to the eye and, in haplorrhines, an additional bony cup behind it (postorbital plate, unique to these primates) protect these vital organs. Primate optic nerve fibers cross from one eye almost equally to both the left and right brain hemispheres for processing, in contrast to other mammals, where inputs are almost wholly to the opposing side. Collectively, these features contribute to excellent depth perception, or stereoscopic vision. Trichromatic color vision, among mammals, is likewise limited to Old World monkeys, apes, and humans with phenotypic convergence in some New World monkeys as well [32]. Platyrrhine and catarrhine primates share a primate specific retinal feature called the macula [33]. This is a region of the central retina that is especially rich in cone photoreceptors, making these species valuable as models of many human visual system disorders [34, 35]. Anthropoids are particularly important for studies of macular disorders that primarily affect cone photoreceptors, or age-related macular degeneration, where rodents, dogs and other mammals cannot provide models that mimic human macular function and dysfunction as effectively as macaques or other nonhuman primates.
Primates have excellent pedal and/or manual grasping abilities; this is exemplified by an opposable thumb in most catarrhines, flat nails rather than claws on at least some digits, and ridged tactile pads and Meissner’s corpuscles on toes and fingers, which combine for an exquisite sense of touch [31]. These adaptations speak to the importance of NHPs for investigating genetic disorders that influence vision or sensorimotor function; in an evolutionary sense, they may reflect, at least in small part, the largely arboreal, branch-grasping history of members of this order [36,37,38].
Primate brains, when controlled for body size, are comparatively large and differ from other mammals in some key areas of neuroanatomy. These include differences in the organization of phylogenetically ancient brain structures, unique alterations in neural connections, and novel structural units [39]. The granular prefrontal (PF) cortex, other PF areas, and certain parietal and temporal areas appear to be uniquely primate, and have been suggested to facilitate rapid goal formation, remarkable utilization of relational metrics—including quantity, duration, and distance—and flexible, sometimes immediate, solving of unique and complex problems [40,41,42,43]. Compared to other mammals, primates are strongly attuned to novelty [e.g., 44, 45] and show marked within-species, inter-individual differences in both novelty response and temperament [e.g., these exhibit heritable variation in baboons, 46] as well as between-species differences. In addition, NHPs, of all nonhuman animals, show the most extensive abilities in executive function tasks such as prospective memory, self-control, metacognition, and episodic memory [47], functions mediated by prefrontal cortical networks that are greatly expanded and differentiated in primates and have unique molecular regulation compared to rodents [48,49,50,51]. This is especially relevant in that executive function deficits are oftentimes the first to be detectable in genetic disorders involving the central nervous system, or that may presage other pathologies [52,53,54]. NHPs are modally very social, exhibit protracted life histories including a prolonged juvenile period, and have great ecological and behavioral plasticity [55,56,57]. In short, NHPs are the nonhuman animals that most closely experience the world in the manner that humans do, with myriad repercussions on the detection, description, and treatment of diseases influencing sensation, perception, behavior, and cognition.
Many other features of morphology likewise render NHPs a uniquely valuable resource for genetic modeling [58, 59]. These include numerous physiological similarities to humans that are rare or absent in other mammals. Regarding reproduction, for example, this includes humanlike estradiol-luteinizing hormone feedback loops in both males and females, similar anatomical origins for sex steroids, menstruation, and a similar pattern of reproductive senescence, in at least some species [4]. NHPs such as baboons and macaques are thus preferred models for reproductive disorders [60].
Leveraging contemporary nonhuman primate genetics for disease model development
The similarities seen between human and NHPs reflect their close genetic affinity. Recent technical advances such as next-generation sequencing have, as noted, made feasible the construction of largely complete and well-annotated primate reference genomes, and more specifically have aided the identification of species-specific genetic variation that is directly relevant to disease risk, causation, or prognosis [61]. What follows will, we hope, give strong indication of the translational advances that have stemmed, and will stem, from further detailed primate genomics research.
Recently, the reduced cost of whole genome sequencing for research colonies of rhesus macaques has facilitated an important change in the approach to and discovery of macaque models of human inherited diseases. It is now possible to perform whole genome or whole exome sequencing on nonhuman primates from research colonies that are identified with spontaneous pathologies that may be relevant to human diseases of various kinds [12, 62]. In addition, the amount of genetic variation present in rhesus macaques and other laboratory primates creates significant opportunities for novel analyses of naturally occurring genetic variation [22, 63]. As a result, we now can more readily identify new nonhuman primate models of human genetic diseases through careful monitoring for relevant pathologies combined with genomic analysis. Two complementary approaches have proven successful: a) sequencing large numbers of research primates in order to identify potentially damaging mutations in genes known or suspected to be involved in human diseases, or b) sequencing particular animals that are identified as having pathology indicative of disease, in order to identify the causative mutation(s).
A primate model of a human genetic disease need not specifically recapitulate the mutations found in human patients. A human genetic disease caused by damaging mutations in a specific gene can often be modeled by other mutations in the same gene that disrupt protein function to an equivalent degree. The disease is the result of disrupting a genetic pathway that consists of many genes working in concert, so that a human disease can be mimicked by any mutations that produce similar disruption to that pathway. Identifying dysregulation in these gene networks beyond specific pathogenic mutations can further elucidate the larger biology of the disease and provide alternative methods to approach treatment.
In addition, it is now possible to generate novel genetic models of disease in nonhuman primates using CRISPR/Cas9 methods to make specific changes in genomic DNA sequences [64]. This approach has been used to produce macaque models related to autism [65] and Parkinsonian neurodegeneration [66]. This approach opens new opportunities to generate particular mutations in specific nonhuman primate genes, and thus can quite remarkably model human genetic disorders. However, this approach entails significant cost, requires large numbers of animals to be performed successfully and can generate off-target mutations that may in some cases compromise the translational value of the model. Moreover, it requires knowledge of the disease-causing mutation in humans a priori, precluding identification of novel disease-causing factors. Thus, while genetic manipulations of primates using CRISPR-Cas9 or analogous methods will likely play a role in the future of biomedical research, the opportunity to exploit naturally occurring variation should not be neglected.
Specific nonhuman primate genetic models of disease
In addition to experimentally induced models of disease, nonhuman primates have long been used as genetic models of diseases having significant heritable components, including when specific genetic origins are unclear in either humans or animals. This includes complex behavioral phenotypes such as anxiety [67,68,69,70], heart disease and other cardiovascular phenotypes [71,72,73,74,75], obesity and type 2 diabetes [25, 76], and heritable cancers [77, 78]. For some of these diseases, nonhuman primate models have led to further elucidation of specific contributing genetic factors or targets for treatments. There is a significant historical body of literature on the genetics of alcohol use disorder, particularly the OPRM1 gene [79,80,81,82], and a more recent breakthrough in understanding the role of NPSR1 in endometriosis [83].
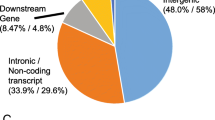
Increasingly, naturally occurring nonhuman primate models of rare human disease are being discovered and developed (Table 1). Animals born with phenotypes similar to those seen in human disease are characterized genetically and are often found to carry mutations in genes that are homologous to putative pathogenic variation in humans. The identification of disease-causing mutations present in the population can then be exploited to develop genetically-defined animal models of disease for use in preclinical studies or, alternatively, to inform breeding decisions to avoid unintentionally producing affected individuals. In the past several years, the number of NHP rare disease studies has grown significantly. The examples below illustrate the breadth and depth of models that have emerged, the pathways that have led to their development, and opportunities for future research directions. For each of these, animals or close relatives confirmed to harbor or potentially harboring disease-causing mutations are present in extant colonies. This list is not exhaustive and the details presented about disease pathologies in both humans and their NHP counterparts are brief, but it does represent a small window into the range of NHP genetic models that have been described and a guidepost for the future (Fig. 1).
Neuronal ceroid lipofuscinosis (CLN7)
Neuronal ceroid lipofuscinoses (NCLs) are a collection of rare, recessive neurodegenerative diseases that typically emerge in early to middle childhood. Commonly referred to as Batten Disease, symptoms include the progressive loss of vision, speech, motor control, and cognitive skills, ultimately leading to premature death. The neuropathology of affected individuals revealed the hallmarks of lysosomal dysfunction, including the abundant accumulation of intracytoplasmic, autofluorescent lipopigment throughout the central nervous system (CNS), with associated neural inflammation and degeneration [84,85,86,87]. NCLs are autosomal recessive disorders linked to fourteen different genes (CLN1-14), each encoding a lysosomal protein, endoplasmic reticulum membrane protein or a protein associated with vesicular membranes [88]. CLN7 disease specifically is associated with nonsense, missense and splice-junction mutations in the CLN7/MFSD8 gene, which encodes a transmembrane transport protein located in the lysosomal membrane [89].
A spontaneous model of CLN7 disease was identified in a Japanese macaque (M. fuscata) breeding colony at the Oregon National Primate Research Center (ONPRC). Affected animals displayed progressive neurological deficits, including visual impairment, tremor, ataxia and imbalance. Imaging and functional studies revealed that CLN7 macaques have measurably reduced retinal thickness and retinal function within the first year, with profound cerebral and cerebellar atrophy progressing over five to six-years. Histological analyses detected an accumulation of highly autofluorescent storage material in cerebral, cerebellar and cardiac tissue, as well as significant degeneration of neurons. Post-mortem brain weights were 28% below average of age-matched, healthy individuals. A homozygous, single base pair deletion within CLN7 exon 8 (c.769delA; p.Ile257LeufsTer36), was identified in five affected individuals, confirming the diagnosis [24]. To date, nine CLN7 model animals have been identified in the ~ 300 member M. fuscata colony.
Krabbe disease (GALC)
Krabbe disease, also known as globoid cell leukodystrophy (GLD), is an autosomal recessive lysosomal storage disease associated with demyelination in the central and peripheral nervous systems. Patients with ‘classic’ or ‘infantile’ disease typically present with notable spasticity and developmental delay within the first 6 months of life, and patients typically succumb to death by 2 years of age [90]. Later onset disease, classified as ‘late infantile’ presenting at 6 months-3 years, and ‘juvenile’ presenting at 3–8 years of age, have slower disease progression and exhibit a range of symptoms that can include vision loss, cognitive decline, seizures, hypotonia, ataxia or spastic paraplegia. Disease severity is variable even within families [91]. Imaging and post-mortem studies of classic cases identify cerebral and cerebellar demyelination, as well as multinuclear (globoid) macrophages in the white matter [92]. In 1971, an association was reported between beta galactocerebrosidase deficiency and the morphologic characteristics of Krabbe disease [93]. This association was supported by the subsequent discovery of a homozygous nonsense mutation in the beta-galactocerebrosidase (GALC) gene in a patient with ‘classic’ Krabbe disease [94], which was followed by numerous reports of missense, insertion, and deletion variants in the GALC gene of Krabbe disease patients [90].
A naturally occurring rhesus macaque model of Krabbe disease was discovered at the Tulane National Primate Research Center (TNPRC) more than two decades ago [95] (Fig. 2). The model was identified following the death of infant at 2 weeks of age, which had a neuropathology similar to human Krabbe disease [96]. Low GALC activity was measured in the infant’s mother, and cDNA sequencing revealed a homozygous, two base pair deletion in GALC exon 4 of the affected individual (c.387delAC; p.Leu130HisfsTer15) [95]. Subsequent breeding of the Krabbe disease carriers enabled additional characterization of the model. Longitudinal studies identified clinical signs of muscle tremors of head and limbs, hypertonia, progressive difficulty ambulating, ataxia, hypermetria, proprioceptive deficits, and respiratory abnormalities. At necropsy, microscopic analysis revealed a striking lack of myelin in the peripheral and central nervous system, and the cerebral, cerebellar, and spinal cord white matter was infiltrated with multinucleated globoid cells [97, 98]. The utility of this macaque model was demonstrated by a study exploring the therapeutic potential of intracranially administered mesenchymal stem cells (MSCs) to treat early onset Krabbe disease. The treatment elicited transient improvements in coordination, ambulation, cognition, and large motor skills, providing preliminary support for further study of MSCs for the treatment of lysosomal storage diseases [99].
The development of a nonhuman primate model of Krabbe disease. A Among other pathogenic mutations, a deletion in humans eliminates the 3’ region of GALC, in rhesus macaques a 2 base pair deletion in exon 4 creates a frameshift and truncated protein in much the same manner. Wild-type initiation and termination positions are shown to the left of the exon model while causative mutations resulting in truncated transcripts are shown to the right. B A pedigree focused on the initial affected individuals (solid gray) identified carriers (half-gray) of the causative genetic mutation. Figure created with BioRender.com
CLCN2-related leukodystrophy (CLCN2)
CLCN2-related leukoencephalopathy (CC2L) is a rare autosomal recessive, neurological disease, previously called Leukoencephalopathy with Ataxia (LKPAT). The discovery of loss of function mutations in the chloride-gated voltage channel 2 (CLCN2) gene among six unrelated patients clarified the molecular basis of the neurological features [100]. The spectrum of symptoms range from childhood onset with mild ataxia, learning disabilities, and headaches to adult onset with mild ataxia and decreased vision. Infertility has been reported in two adult males [100, 101]. MRI analysis identifies white matter abnormalities in CC2L cases. Affected individuals have decreased apparent diffusion coefficient values in the posterior limbs of the internal capsules, middle cerebral peduncles, pyramidal tracts in the pons, and middle cerebellar peduncles. The findings indicate myelin microvacuolation within certain brain regions [100].
A novel leukodystrophy case was identified in a juvenile rhesus macaque born at the ONPRC. Close observation identified three short seizure type periods and repeated episodes of hand and arm tremors. A “star gazing” behavior, typical of macaques with impaired vision, was also noted. At necropsy, primary findings included laminar cerebral neuronal necrosis, and diffuse marked vacuolation of the central nervous system white matter. Pedigree analysis identified the case to be the product of a consanguineous mating, suggesting a possible genetic link to the neurological symptoms. Subsequent genomic sequencing of the proband revealed a homozygous CLCN2 missense mutation (c.1412G > A; p.Arg471His) that is identical to human ClinVar allele 214,433 (p.Arg471His) and associated with CC2L [102]. The same macaque allele has been detected in both the Wisconsin National Primate Research Center (WNPRC) and ONPRC breeding colonies, and has an overall a minor allele frequency of 0.0098 in the mGAP database. Taken together, the clinical, histological and genetic findings suggest this to be the first identified case of nonhuman primate CC2L.
Pelizaeus–Merzbacher disease (PLP1)
Pelizaeus–Merzbacher disease (PMD) is the most common leukodystrophy associated with hypomyelination, affecting approximately 1 in 400,000 individuals [103]. PMD symptoms range in severity, with mild cases developing spastic paraplegia over time, and severe cases presenting with hypotonia, nystagmus, respiratory distress, and stridor shortly after birth [104]. PMD is caused by mutations in the proteolipid apoprotein (PLP1) gene, an X-linked gene that encodes a lipid binding protein that is reported to stabilize myelin [105, 106]. While PLP1 gene duplications, deletions and point mutations have been linked to PMD, the most severe cases have frequently been associated with missense mutations in exons 2 and 4 [107].
A rhesus macaque model of PMD was recently identified at the ONPRC, following the clinical and genetic analysis of three male neonates exhibiting neurological deficits [108]. The infants displayed profound intention tremors, head bobbing, nystagmus and reduced respiratory capacity. Histopathological analyses of brain tissue obtained following necropsy revealed a CNS dysmyelinating disorder, as initially assessed by Luxol fast blue staining. Immunohistochemical analysis identified, a complete lack of the myelin protein PLP throughout the corpus callosum, a marked reduction in the expression of myelin binding protein (MBP), and a lack of clear myelinated structures. Pedigree analysis identified all three males to be related, and genomic sequencing identified a missense mutation within the PLP1 gene (PLP1: n.682 T > C; p.Cys228Arg) [108]. To date, the PLP1 missense mutation has only been detected at the ONPRC and has a minor allele frequency of 0.0004 among the 2,054 rhesus macaques reported in the macaque Gentoype and Phenotype database (mGAP) [23].
Achromatopsia (PDE6C)
Achromatopsia, or rod monochromacy, is characterized by the loss of macular function critical for high acuity vision, as well as color perception. A progressive disorder, initial vision problems manifest in childhood with a gradual decline until adulthood by which time cone photoreceptors are lost completely. People with achromatopsia are also photophobic due to their dependence on rod photoreceptors. This disease is genetically heterogenous in humans with mutations inherited in an autosomal recessive manner.
Colony staff at California National Primate Research Center (CNPRC) identified two juvenile rhesus macaques that displayed evidence of visual impairment. Whole genome sequencing of these animals revealed that both are homozygous for a missense mutation in the gene PDE6C that inactivates the catalytic domain of this enzyme [35]. Ophthalmic examinations showed that the affected macaques have essentially normal function of their rod photoreceptors, but little or no cone photoreceptor function. This is logical because PDE6C is expressed in cone but not rod photoreceptors; loss of cone function will impair high acuity vision and color perception but preserves peripheral vision. PDE6C is one of six genes associated with achromatopsia in humans [109]. Macaques with PDE6C mutations also show evidence of difficulty in bright light. Subsequent genotyping of additional CNPRC rhesus macaques has identified a number of heterozygous carriers, and a breeding program has been established to produce additional homozygotes.
Bardet-Beidl syndrome (BBS7)
Bardet-Biedl Syndrome (BBS) is a complex disorder exhibiting variable phenotypic expression, but generally including retinal degeneration, obesity, and kidney dysfunction along with various other symptoms. Although syndromic with broad systemic effects, the most common indication of the disease is severe vision loss during childhood. BBS is a ciliopathy affecting cell structures involved in cell–cell communication and development. Approximately 1 in 250,000 individuals have BBS and there is currently no cure for the disease. More than 20 different genes have been implicated in BBS and mutations are commonly recessive and often oligogenic [110].
Several rhesus macaques from the ONPRC were recognized as having both spontaneous retinal degeneration and kidney disease [111]. Initially, a female rhesus macaque presented with significant visual impairment and multiple structural and histological problems affecting the kidneys. Genetic analyses found that this animal was homozygous for a single base deletion in exon 3 of the gene BBS7. Analyses of other rhesus macaques heterozygous and homozygous for the exon 3 deletion confirmed the genetic association and diagnosis as Bardet-Biedl Syndrome. The additional genetically validated and affected animals similarly displayed the range of deficits described in human BBS7 disease. Moreover, the retinal pathology involved loss of function of photoreceptors and closely parallels the disease progression described in human Bardet-Biedl Syndrome [111, 112].
Thyroid dyshormonogenesis (TG)
Thyroid dyshormogenesis occurs when the pathway leading to the synthesis of the hormonally active iodothyronines, T4 and T3, is defective. This leads to hypothyroidism and goiter. The downstream effects of congenital hypothyroidism are numerous including poor growth and delayed development particularly when untreated.
Genetic mutations leading to defects in thyroid hormone synthesis account for 15–20% of all cases of congenital hypothyroidism in humans, representing approximately 1:25,000 neonates [113]. The genes most commonly affected are DUOX2, SLC5A5, TG, and TPO. Mutations, almost always inherited in a recessive manner, result in abnormally low thyroid hormone levels [114].
Dyshormonogenetic goiter due to a defect in TG has been recognized in rhesus macaques at ONPRC. The initially identified animal was euthanized due to musculoskeletal abnormalities. The thyroid gland was markedly enlarged, pink, and fleshy. Microscopically, the follicular epithelium was hypertrophic and hyperplastic with diffuse colloid atrophy. The long bones exhibited epiphyseal immaturity and dysplasia, typical of congenital hypothyroidism. This animal was homozygous for a frame-shift deletion in the TG gene (c.5513_5514delAA, p.Lys1838fs). Two additional stillborn animals were identified with similar gross and microscopic appearance of the thyroid gland; one was confirmed as homozygote and the other was the offspring of a heterozygote dam. Of note, phenotypically similar cases of hypothyroidism associated with congenital goiters were previously described in this colony [115]. The three affected animals were offspring of the same parents. Two of the affected animals lived to adulthood; the other was stillborn following prolonged gestation. The adult animals exhibited abnormal facial features suggestive of delayed bone growth. The underlying genetic defect was not identified.
Type 3 von Willebrand’s disease (VWF)
Von Willebrand’s disease (VWD) represents the most commonly inherited disorder of human coagulation and afflicts up to 1% of the population [116]. It occurs in multiple primary types, with type 1 representing reduced quantity of Von Willebrand’s factor (VWF), type 2 representing reduced function of VWF, and type 3 representing an absence of VWF [116]. Each of these types can lead to bleeding due to VWF’s role in platelet adhesion and aggregation. There are over 1000 described mutations that result in VWD and those are most commonly associated with type 2 or 3 disease. Type 3 VWD is inherited in either a recessive or co-dominant fashion with absence of VWF owing to mutations in the VWF gene that render the individual to have no circulating VWF [116].
Type 3 VWD has been described in a family of rhesus macaques where one young monkey had no measurable VWF activity [117]. This disease was identified at the New England Primate Research Center in an individual that was found to be persistently bleeding despite only minor injuries at a young age [117]. The disease was found to be familial on screening of nuclear family members where reduced VWF levels were identified in other adults macaques [117]. These findings are typical in type 3 VWD in humans where heterozygous individuals may have reduced VWF but do not spontaneously bleed [116, 117]. This rhesus model of type 3 VWD was proposed to be autosomal recessive in its pattern of inheritance, however no genetic study of mutations underlying this disorder in this pedigree was performed [117].
Lynch syndrome (MLH1)
Lynch Syndrome is the most common form of hereditary colorectal cancer. The disease is caused by inheritance of damaging mutations in one of four DNA mismatch repair genes that code for proteins essential to the DNA repair mechanisms in human cells. People who inherit a dysfunctional copy of one of these four genes (MLH1, MSH2, MSH6 or PMS2) are at dramatically increased risk for colorectal cancer as well as tumors of the ovary, endometrium, stomach and other organs. More than one million people in the United States carry a Lynch Syndrome mutation that raises their cancer risk [118] with mean age of onset in their 40’s. In addition to mutations leading to tumorigenesis, Lynch Syndrome patients also experience insertion/deletion mutations in microsatellite repeats within protein coding genes. These indel mutations generate novel peptide sequences (neoantigens) that can be used to stimulate the native immune system and thus to attack tumor cells.
More than 60 cases of spontaneous colorectal cancer have been identified in rhesus macaques at the Keeling Center for Comparative Medicine and Research, part of the University of Texas MD Anderson Cancer Center [78]. The tumors observed in these animals are generally located in the ileocecal junction, proximal colon or cecum, highly reminiscent of human Lynch Syndrome tumors. In addition, significant histological similarities were identified, and immunohistochemistry showed that the tumors generally lacked expression of MLH1 and PMS2 proteins [78]. Subsequent DNA sequencing showed that macaques suffering these tumors had significantly elevated frequencies of a stop codon in MLH1 (c.1029C < G, p.Tyr343Ter). Furthermore, carriers of this mutation showed substantial instability in microsatellite sequences across the macaque genome, a widely used indicator of Lynch Syndrome pathology in humans. Following these initial genomic analyses, gene expression analyses have shown that the macaque tumors exhibit transcription profiles very similar to those in human Lynch Syndrome tumors [119].
Epidermolysis Bullosa simplex (KRT5)
Epidermolysis bullosa simplex (EBS) is one of the most common genetic bullous skin diseases. It is characterized by the separation of the skin at the basal keratinocytes region after trauma and blister formation. The prevalence is estimated to be 1 per 25,000–50,000 births, and depending on the mutation, can follow either recessive or dominant inheritance [120]. EBS is a heterogenous group of diseases, which range from localized to severe effects. Mutations in keratin 5 (KRT5) and keratin 14 (KRT14) genes account for the majority of EBS cases [121]. Phenotype–genotype analysis of patients has shown that mutations that disrupt the central alpha-helical rod of the keratin protein are associated with a more severe disease phenotype [122].
A natural rhesus macaque model of EBS was recently reported at the ONPRC. Two stillborn macaques were initially recognized as being likely EBS cases based on the appearance of widespread sloughing of skin at delivery. Microscopic findings in both animals included multifocal to coalescing, variably sized intraepidermal clefts, with prominent basal cell vacuolation and fragmentation. Retrospective DNA sequence analysis determined that the two cases were both homozygous for a 34 bp insertion within KRT5 exon 5 (p.Lys363fs), predicted to disrupt the 4th coil of the alpha-helical rod. At the time of discovery, the mGAP database included 278 genomes and the KRT5 mutation occurred at 0.0054 frequency, with no other homozygotes detected. Six asymptomatic individuals with heterozygous KRT5 insertion mutations were subsequently identified, based on pedigree relationship to the focal cases [123].
Implications for future work
Genetic diseases in humans are also present in nonhuman primates. While this simple fact has been long recognized, it has been difficult to take advantage for developing research models. The spontaneous and irregular emergence of animals with disease phenotypes often could not be duplicated, particularly for diseases that caused premature death or diminished reproductive capacity. Advances in our fundamental understanding of primate genomes, the reduced cost of whole genome sequencing, and the subsequent large-scale identification of nonhuman primate genetic variation have not only allowed for a better understanding of the molecular underpinnings of disease in nonhuman primates, but they also allow for greater control over the production of these models.
The identification of disease-causing mutations in nonhuman primates is an important advance for biomedical research; it allows for the purposeful breeding of animal models to study human disease. These models often faithfully and accurately recapitulate human disease in both presentation and etiology, allowing for the discovery of relevant biomarkers and the pre-symptomatic or longitudinal study of disease pathology. The full range of state-of-the-art biomedical techniques, including advanced imaging, electrophysiology, auditory, optical, and cognitive measures can be monitored. Post-mortem gross and microscopy histology can be used to study disease-associated molecular and cellular changes with minimal confounding factors. Importantly, the relevance of the findings are directly translational to the human condition.
One of the most exciting aspects of the genetically parallel, NHP disease models are the associated opportunities to develop and test promising approaches to the treatment or cure of these human diseases. Development of treatments in utero or otherwise prior to symptom emergence is now feasible in ways that were previously inaccessible. Genomic medicine approaches, including protein replacement, gene silencing or editing, and stem cell therapies can be evaluated in these translational models to insure efficient delivery, distribution, and longevity. Pre-clinical testing in an anatomically and physiologically relevant, large animal model will also be key for optimizing the efficacy, safety, and specificity of such treatments. The recent advances in NHP rare disease model development are both timely and critical as these emerging genomic-based approaches are likely to be the best, if not only, way to effectively treat many of these debilitating or fatal rare diseases.
Conclusions
Nonhuman primates represent an important model organism for biomedical research. Importantly, they can also serve a valuable role as genetic models of disease, including rare disease. Taking advantage of the genetic similarities between humans and NHPs and the recent advances in next generation sequencing technology that have allowed for increasingly comprehensive catalogs of NHP variation, new models of human rare disease are emerging. These offer the possibility for new therapeutic development and understandings of disease that have been previously elusive.
Availability of data and material
Genomic data is available at http://mgap.ohsu.edu or from the corresponding author on reasonable request.
References
Haendel M, Vasilevsky N, Unni D, Bologa C, Harris N, Rehm H, et al. How many rare diseases are there? Nat Rev Drug Discov. 2020;19(2):77–8.
Wolpert L. Positional information and pattern formation in development. Dev Genet. 1994;15(6):485–90.
Simmons D. The use of animal models in studying genetic disease: transgenesis and induced mutation. Nature Education. 2008;1:70.
Phillips KA, Bales KL, Capitanio JP, Conley A, Czoty PW, Hart BA, et al. Why primate models matter. Am J Primatol. 2014;76(9):801–27.
Bryda EC. The mighty mouse: the impact of rodents on advances in biomedical research. Mo Med. 2013;110(3):207–11.
Perlman RL. Mouse models of human disease: an evolutionary perspective. Evol Med Publ Health. 2016;2016(1):170–6.
Doyle A, McGarry MP, Lee NA, Lee JJ. The construction of transgenic and gene knockout/knockin mouse models of human disease. Transgenic Res. 2012;21(2):327–49.
Vandamme TF. Use of rodents as models of human diseases. J Pharmacy Bioallied Sci. 2014;6(1):2.
Wolfe JH. Gene therapy in large animal models of human genetic diseases. ILAR J. 2009;50(2):107–11.
Bergen WG, Mersmann HJ. Comparative aspects of lipid metabolism: impact on contemporary research and use of animal models. J Nutr. 2005;135(11):2499–502.
Gordon CJ. The mouse thermoregulatory system: its impact on translating biomedical data to humans. Physiol Behav. 2017;179:55–66.
Vallender EJ, Miller GM. Nonhuman primate models in the genomic era: a paradigm shift. ILAR J. 2013;54(2):154–65.
Pinnapureddy AR, Stayner C, McEwan J, Baddeley O, Forman J, Eccles MR. Large animal models of rare genetic disorders: sheep as phenotypically relevant models of human genetic disease. Orphanet J Rare Dis. 2015;10(1):1–8.
Lindblad-Toh K. What animals can teach us about evolution, the human genome, and human disease. Ups J Med Sci. 2020;125(1):1–9.
Tavaré S, Marshall CR, Will O, Soligo C, Martin RD. Using the fossil record to estimate the age of the last common ancestor of extant primates. Nature. 2002;416(6882):726–9.
Finstermeier K, Zinner D, Brameier M, Meyer M, Kreuz E, Hofreiter M, et al. A mitogenomic phylogeny of living primates. PLoS ONE. 2013;8(7):e69504.
Reis MD, Gunnell GF, Barba-Montoya J, Wilkins A, Yang Z, Yoder AD. Using phylogenomic data to explore the effects of relaxed clocks and calibration strategies on divergence time estimation: primates as a test case. Syst Biol. 2018;67(4):594–615.
Steiper ME, Young NM. Primate molecular divergence dates. Mol Phylogenet Evol. 2006;41(2):384–94.
Pozzi L, Hodgson JA, Burrell AS, Sterner KN, Raaum RL, Disotell TR. Primate phylogenetic relationships and divergence dates inferred from complete mitochondrial genomes. Mol Phylogenet Evol. 2014;75:165–83.
Perelman P, Johnson WE, Roos C, Seuánez HN, Horvath JE, Moreira MAM, et al. A molecular phylogeny of living primates. PLoS Genet. 2011;7(3):e1001342.
Gibbs RA, Rogers J, Katze MG, Bumgarner R, Weinstock GM, Mardis ER, et al. Evolutionary and biomedical insights from the rhesus macaque genome. Science. 2007;316(5822):222–34.
Warren WC, Harris RA, Haukness M, Fiddes IT, Murali SC, Fernandes J, et al. Sequence diversity analyses of an improved rhesus macaque genome enhance its biomedical utility. Science. 2020;370(6523):eabc6617.
Bimber BN, Yan MY, Peterson SM, Ferguson B. mGAP: the macaque genotype and phenotype resource, a framework for accessing and interpreting macaque variant data, and identifying new models of human disease. BMC Genomics. 2019;20(1):176.
McBride JL, Neuringer M, Ferguson B, Kohama SG, Tagge IJ, Zweig RC, et al. Discovery of a CLN7 model of Batten disease in non-human primates. Neurobiol Dis. 2018;119:65–78.
Comuzzie AG, Cole SA, Martin L, Carey KD, Mahaney MC, Blangero J, et al. The baboon as a nonhuman primate model for the study of the genetics of obesity. Obes Res. 2003;11(1):75–80.
Jasinska AJ, Schmitt CA, Service SK, Cantor RM, Dewar K, Jentsch JD, et al. Systems biology of the vervet monkey. ILAR J. 2013;54(2):122-43.
The Marmoset Genome Sequencing and Analysis Consortium. The common marmoset genome provides insight into primate biology and evolution. Nat Genet. 2014;46(8):850.
Sasaki E. Creating genetically modified marmosets. In: Marini RP, Wachtman LM, Tardif SD, Mansfield K, Fox JG, editors. The common marmoset in captivity and biomedical research. London: Elsevier; 2019. p. 335–53.
Vallender EJ. The genome of the common marmoset. In: Marini RP, Wachtman LM, Tardif SD, Mansfield K, Fox JG, editors. The common marmoset in captivity and biomedical research. London: Elsevier; 2019. p. 313–33.
Ezran C, Karanewsky CJ, Pendleton JL, Sholtz A, Krasnow MR, Willick J, et al. The mouse lemur, a genetic model organism for primate biology, behavior, and health. Genetics. 2017;206(2):651–64.
Martin RD. Primates. Curr Biol. 2012;22(18):R785–90.
Rowe MH. Trichromatic color vision in primates. News Physiol Sci. 2018;17:93–8.
Schwab IR. Evolution’s witness: How eyes evolved. Oxford: Oxford University Press; 2012.
Picaud S, Dalkara D, Marazova K, Goureau O, Roska B, Sahel JA. The primate model for understanding and restoring vision. Proceedings of the National Academy of Sciences of the United States of America. 2019.
Moshiri A, Chen R, Kim S, Harris RA, Li Y, Raveendran M, et al. A nonhuman primate model of inherited retinal disease. J Clin Invest. 2019;129(2):863–74.
Smith GE. The evolution of man. Annual Report of the Board of Regents of the Smithsonian Institution for the Year Ending June 30 1912. Washington, D.C.: Government Printing Office; 1913. p. 553–73.
Cartmill M. Rethinking primate origins. Science. 1974;184(4135):436–43.
Sayers K. Models of primate evolution. eLS. 2015:1-0. doi:https://doi.org/10.1002/9780470015902.a0026406
Preuss TM. Evolutionary specializations of primate brain systems. In: Ravosa MJ, Dagosto M, editors. Primate origins: adaptations and evolution. New York: Springer; 2007. p. 625–75.
Genovesio A, Wise SP, Passingham RE. Prefrontal–parietal function: from foraging to foresight. Trends Cogn Sci. 2014;18(2):72–81.
Sayers K, Menzel CR. Memory and foraging theory: chimpanzee utilization of optimality heuristics in the rank-order recovery of hidden foods. Anim Behav. 2012;84(4):795–803.
Menzel CR. Spontaneous use of matching visual cues during foraging by long-tailed macaques (Macaca fascicularis). J Comp Psychol. 1996;110:370–6.
Roberts AC, Clarke HF. Why we need nonhuman primates to study the role of ventromedial prefrontal cortex in the regulation of threat-and reward-elicited responses. Proc Natl Acad Sci. 2019;116(52):26297–304.
Glickman SE, Sroges RW. Curiosity in zoo animals. Behaviour. 1966;26:151–88.
Menzel EW, Menzel CR. Cognitive, developmental and social aspects of responsiveness to novel objects in a family group of marmosets (Saguinus fuscicollis). Behaviour. 1979;70(3–4):251–79.
Johnson Z, Brent L, Alvarenga JC, Comuzzie AG, Shelledy W, Ramirez S, et al. Genetic influences on response to novel objects and dimensions of personality in Papio baboons. Behav Genet. 2015;45(2):215–27.
Beran MJ, Menzel CR, Parrish AE, Perdue BM, Sayers K, Smith JD, et al. Primate cognition: attention, episodic memory, prospective memory, self-control, and metacognition as examples of cognitive control in nonhuman primates. Wiley Interdiscipl Rev Cogn Sci. 2016;7(5):294–316.
Arnsten AFT, Datta D, Wang M. The genie in the bottle-magnified calcium signaling in dorsolateral prefrontal cortex. Mol Psychiatry. 2021;26(8):3684–700.
Goldman-Rakic PS. The prefrontal landscape: implications of functional architecture for understanding human mentation and the central executive. Philos Trans R Soc Lond B Biol Sci. 1996;351(1346):1445–53.
Szczepanski SM, Knight RT. Insights into human behavior from lesions to the prefrontal cortex. Neuron. 2014;83(5):1002–18.
Wheeler MA, Stuss DT, Tulving E. Toward a theory of episodic memory: the frontal lobes and autonoetic consciousness. Psychol Bull. 1997;121(3):331–54.
Cuevas K, Bell MA. Infant attention and early childhood executive function. Child Dev. 2014;85(2):397–404.
Welsh MC, Pennington BF, Ozonoff S, Rouse B, McCabe ER. Neuropsychology of early-treated phenylketonuria: specific executive function deficits. Child Dev. 1990;61(6):1697–713.
Berenguer C, Roselló B, Colomer C, Baixauli I, Miranda A. Children with autism and attention deficit hyperactivity disorder. Relationships between symptoms and executive function, theory of mind, and behavioral problems. Res Dev Disabil. 2018;83:260–9.
Menzel CR. Solving ecological problems. In: Mitani JC, Call J, Kappeler PM, Palombit RA, Silk JB, editors. The evolution of primate societies. Chicago: The University of Chicago Press; 2012. p. 609–27.
Sayers K, Evans TA, Menzel E, Smith JD, Beran MJ. The misbehaviour of a metacognitive monkey. Behaviour. 2015;152:727–56.
Kummer H. Primate societies: group techniques of ecological adaptation. Arlington Heights: Harlan Davidson; 1971. p. 1971.
King FA, Yarbrough CJ, Anderson DC, Gordon TP, Gould KG. Primates. Science. 1988;240(4858):1475–82.
Harding JD. Nonhuman primates and translational research: progress, opportunities, and challenges. ILAR J. 2017;58(2):141–50.
Bauer C. The baboon (Papio sp.) as a model for female reproduction studies. Contraception. 2015;92(2):120–3.
Rogers J, Gibbs RA. Comparative primate genomics: emerging patterns of genome content and dynamics. Nat Rev Genet. 2014;15(5):347–59.
Rogers J. In transition: primate genomics at a time of rapid change. ILAR J Natl Res Council Inst Lab Anim Resour. 2013;54(2):224–33.
Huang YS, Ramensky V, Jasinska AJ, Jung Y, Choi OW, et al. Sequencing strategies and characterization of 721 vervet monkey genomes for future genetic analyses of medically relevant traits. BMC Biol. 2015;13(1):1–10.
Feng G, Jensen FE, Greely HT, Okano H, Treue S, Roberts AC, et al. Opportunities and limitations of genetically modified nonhuman primate models for neuroscience research. Proc Natl Acad Sci USA. 2020;117(39):24022–31.
Zhou Y, Sharma J, Ke Q, Landman R, Yuan J, Chen H, et al. Atypical behaviour and connectivity in SHANK3-mutant macaques. Nature. 2019;570(7761):326–31.
Yang W, Guo X, Tu Z, Chen X, Han R, Liu Y, et al. PINK1 kinase dysfunction triggers neurodegeneration in the primate brain without impacting mitochondrial homeostasis. Protein Cell. 2022;13(1):26–46.
Fox AS, Harris RA, Rosso LD, Raveendran M, Kamboj S, Kinnally EL, et al. Infant inhibited temperament in primates predicts adult behavior, is heritable, and is associated with anxiety-relevant genetic variation. Mol Psychiatry. 2021;26(11):6609–18.
Rogers J, Shelton SE, Shelledy W, Garcia R, Kalin NH. Genetic influences on behavioral inhibition and anxiety in juvenile rhesus macaques. Genes Brain Behav. 2008;7(4):463–9.
Williamson DE, Coleman K, Bacanu SA, Devlin BJ, Rogers J, Ryan ND, et al. Heritability of fearful-anxious endophenotypes in infant rhesus macaques: a preliminary report. Biol Psychiatry. 2003;53(4):284–91.
Fawcett GL, Dettmer AM, Kay D, Raveendran M, Higley JD, Ryan ND, et al. Quantitative genetics of response to novelty and other stimuli by infant rhesus macaques (Macaca mulatta) across three behavioral assessments. Int J Primatol. 2014;35(1):325–39.
Kanthaswamy S, Reader R, Tarara R, Oslund K, Allen M, Ng J, et al. Large scale pedigree analysis leads to evidence for founder effects of hypertrophic cardiomyopathy in rhesus macaques (Macaca mulatta). J Med Primatol. 2014;43(4):288–91.
Reader JR, Canfield DR, Lane JF, Kanthaswamy S, Ardeshir A, Allen AM, et al. Left ventricular hypertrophy in rhesus macaques (Macaca mulatta) at the California National Primate Research Center (1992–2014). Comp Med. 2016;66(2):162–9.
Bose T, Voruganti VS, Tejero ME, Proffitt JM, Cox LA, VandeBerg JL, et al. Quantitative loci regulating plasma levels of gamma glutamyl transferase and albumin and their genetic correlations with cardiovascular risk factors. Exp Biol Med. 2009;234(12):1519–24.
Rainwater DL, Kammerer CM, Mahaney MC, Rogers J, Cox LA, Schneider JL, et al. Localization of genes that control LDL size fractions in baboons. Atherosclerosis. 2003;168(1):15–22.
Ueda Y, Kovacs S, Reader R, Roberts JA, Stern JA. Heritability and pedigree analyses of hypertrophic cardiomyopathy in rhesus macaques (Macaca mulatta). Front Vet Sci. 2021;8:540493.
Cai G, Cole SA, Tejero ME, Proffitt JM, Freeland-Graves JH, Blangero J, et al. Pleiotropic effects of genes for insulin resistance on adiposity in baboons. Obes Res. 2004;12(11):1766–72.
Simmons HA, Mattison JA. The incidence of spontaneous neoplasia in two populations of captive rhesus macaques (Macaca mulatta). Antioxid Redox Signal. 2011;14(2):221–7.
Dray BK, Raveendran M, Harris RA, Benavides F, Gray SB, Perez CJ, et al. Mismatch repair gene mutations lead to lynch syndrome colorectal cancer in rhesus macaques. Genes Cancer. 2018;9(3–4):142–52.
Barr CS. Non-human primate models of alcohol-related phenotypes: the influence of genetic and environmental factors. Curr Top Behav Neurosci. 2013;13:223–49.
Vallender EJ, Rüedi-Bettschen D, Miller GM, Platt DM. A pharmacogenetic model of naltrexone-induced attenuation of alcohol consumption in rhesus monkeys. Drug Alcohol Depend. 2010;109(1–3):252–6.
Barr CS, Chen SA, Schwandt ML, Lindell SG, Sun H, Suomi SJ, et al. Suppression of alcohol preference by naltrexone in the rhesus macaque: a critical role of genetic variation at the micro-opioid receptor gene locus. Biol Psychiatry. 2010;67(1):78–80.
Barr CS, Schwandt M, Lindell SG, Chen SA, Goldman D, Suomi SJ, et al. Association of a functional polymorphism in the mu-opioid receptor gene with alcohol response and consumption in male rhesus macaques. Arch Gen Psychiatry. 2007;64(3):369–76.
Tapmeier TT, Rahmioglu N, Lin J, De Leo B, Obendorf M, Raveendran M, et al. Neuropeptide S receptor 1 is a nonhormonal treatment target in endometriosis. Sci Transl Med. 2021;13(608):eaab6469.
Anderson GW, Goebel HH, Simonati A. Human pathology in NCL. Biochim Biophys Acta. 2013;1832(11):1807–26.
Cooper JD, Tarczyluk MA, Nelvagal HR. Towards a new understanding of NCL pathogenesis. Biochim Biophys Acta. 2015;1852(10 Pt B):2256–61.
Palmer DN, Barry LA, Tyynela J, Cooper JD. NCL disease mechanisms. Biochim Biophys Acta. 2013;1832(11):1882–93.
Radke J, Stenzel W, Goebel HH. Human NCL neuropathology. Biochim Biophys Acta. 2015;1852(10 Pt B):2262–6.
Carcel-Trullols J, Kovacs AD, Pearce DA. Cell biology of the NCL proteins: What they do and don’t do. Biochim Biophys Acta. 2015;1852(10 Pt B):2242–55.
Siintola E, Topcu M, Aula N, Lohi H, Minassian BA, Paterson AD, et al. The novel neuronal ceroid lipofuscinosis gene MFSD8 encodes a putative lysosomal transporter. Am J Hum Genet. 2007;81(1):136–46.
Wenger DA, Rafi MA, Luzi P, Datto J, Costantino-Ceccarini E. Krabbe disease: genetic aspects and progress toward therapy. Mol Genet Metab. 2000;70(1):1–9.
Tappino B, Biancheri R, Mort M, Regis S, Corsolini F, Rossi A, et al. Identification and characterization of 15 novel GALC gene mutations causing Krabbe disease. Hum Mutat. 2010;31(12):E1894–914.
Fiumara A, Barone R, Arena A, Filocamo M, Lissens W, Pavone L, et al. Krabbe leukodystrophy in a selected population with high rate of late onset forms: longer survival linked to c.121G>A (p.Gly41Ser) mutation. Clin Genet. 2011;80(5):452–8.
Suzuki Y, Suzuki K. Krabbe’s globoid cell leukodystrophy: deficiency of glactocerebrosidase in serum, leukocytes, and fibroblasts. Science. 1971;171(3966):73–5.
Sakai N, Inui K, Fujii N, Fukushima H, Nishimoto J, Yanagihara I, et al. Krabbe disease: isolation and characterization of a full-length cDNA for human galactocerebrosidase. Biochem Biophys Res Commun. 1994;198(2):485–91.
Luzi P, Rafi MA, Victoria T, Baskin GB, Wenger DA. Characterization of the rhesus monkey galactocerebrosidase (GALC) cDNA and gene and identification of the mutation causing globoid cell leukodystrophy (Krabbe disease) in this primate. Genomics. 1997;42(2):319–24.
Baskin G, Alroy J, Li Y, Dayal Y, Raghavan S, Sharer L, editors. Galactosylceramide-lipidosis in rhesus-monkeys. Laboratory investigation. Baltimore: Williams & Wilkins; 1989. p. 21201–2436.
Baskin GB, Ratterree M, Davison BB, Falkenstein KP, Clarke MR, England JD, et al. Genetic galactocerebrosidase deficiency (globoid cell leukodystrophy, Krabbe disease) in rhesus monkeys (Macaca mulatta). Lab Anim Sci. 1998;48(5):476–82.
Borda JT, Alvarez X, Mohan M, Ratterree MS, Phillippi-Falkenstein K, Lackner AA, et al. Clinical and immunopathologic alterations in rhesus macaques affected with globoid cell leukodystrophy. Am J Pathol. 2008;172(1):98–111.
Isakova IA, Baker KC, Dufour J, Phinney DG. Mesenchymal stem cells yield transient improvements in motor function in an infant rhesus macaque with severe early-onset krabbe disease. stem Cells Transl Med. 2017;6(1):99–109.
Depienne C, Bugiani M, Dupuits C, Galanaud D, Touitou V, Postma N, et al. Brain white matter oedema due to ClC-2 chloride channel deficiency: an observational analytical study. Lancet Neurol. 2013;12(7):659–68.
Di Bella D, Pareyson D, Savoiardo M, Farina L, Ciano C, Caldarazzo S, et al. Subclinical leukodystrophy and infertility in a man with a novel homozygous CLCN2 mutation. Neurology. 2014;83(13):1217–8.
van der Knaap MS, Depienne C, Sedel F, Abbink TEM. CLCN2-Related Leukoencephalopathy: University of Washington, Seattle, Seattle (WA); 1993 1993.
Osorio MJ, Goldman SA. Neurogenetics of Pelizaeus-Merzbacher disease. Handb Clin Neurol. 2018;148:701–22.
Singh R, Samanta D. Pelizaeus-Merzbacher Disease. StatPearls [Internet]. 2021.
Hodes ME, Pratt VM, Dlouhy SR. Genetics of Pelizaeus-Merzbacher disease. Dev Neurosci. 1993;15(6):383–94.
Jurevics H, Hostettler J, Sammond DW, Nave KA, Toews AD, Morell P. Normal metabolism but different physical properties of myelin from mice deficient in proteolipid protein. J Neurosci Res. 2003;71(6):826–34.
Cailloux F, Gauthier-Barichard F, Mimault C, Isabelle V, Courtois V, Giraud G, et al. Genotype-phenotype correlation in inherited brain myelination defects due to proteolipid protein gene mutations. Clinical European Network on Brain Dysmyelinating Disease. Eur J Hum Genet. 2000;8(11):837–45.
Sherman LS, Su W, Johnson AL, Peterson SM, Cullin C, Lavinder T, et al. A novel non-human primate model of Pelizaeus-Merzbacher disease. Neurobiol Dis. 2021;158: 105465.
Thiadens AA, den Hollander AI, Roosing S, Nabuurs SB, Zekveld-Vroon RC, Collin RW, et al. Homozygosity mapping reveals PDE6C mutations in patients with early-onset cone photoreceptor disorders. Am J Hum Genet. 2009;85(2):240–7.
Priya S, Nampoothiri S, Sen P, Sripriya S. Bardet-Biedl syndrome: Genetics, molecular pathophysiology, and disease management. Indian J Ophthalmol. 2016;64(9):620–7.
Peterson SM, McGill TJ, Puthussery T, Stoddard J, Renner L, Lewis AD, et al. Bardet–Biedl Syndrome in rhesus macaques: a nonhuman primate model of retinitis pigmentosa. Exp Eye Res. 2019;189:107825.
Aleman TS, O’Neil EC, O’Connor K, Jiang YY, Aleman IA, Bennett J, et al. Bardet-Biedl syndrome-7 (BBS7) shows treatment potential and a cone-rod dystrophy phenotype that recapitulates the non-human primate model. Ophthalmic Genet. 2021;42(3):252–65.
Knobel M, Medeiros-Neto G. An outline of inherited disorders of the thyroid hormone generating system. Thyroid. 2003;13(8):771–801.
Park SM, Chatterjee VK. Genetics of congenital hypothyroidism. J Med Genet. 2005;42(5):379–89.
Olson LC, Palotay JL, Haines JE, Hanada J, Bergquist DY. Compensated, goitrous hypothyroidism in rhesus macaques. Lab Anim Sci. 1985;35(6):629–34.
Yadegari H, Oldenburg J. The current understanding of molecular pathogenesis of quantitative von willebrand disease, types 1 and 3. Hamostaseologie. 2020;40(1):105–18.
Patterson MM, Jackson LR, Brooks MB, Catalfamo JL. Type-3 von willebrand’s disease in a rhesus monkey (Macaca mulatta). Comp Med. 2002;52(4):368–71.
Win AK, Jenkins MA, Dowty JG, Antoniou AC, Lee A, Giles GG, et al. Prevalence and penetrance of major genes and polygenes for colorectal cancer. Cancer Epidemiol Biomarkers Prev. 2017;26(3):404–12.
Ozirmak Lermi N, Gray SB, Bowen CM, Reyes-Uribe L, Dray BK, Deng N, et al. Comparative molecular genomic analyses of a spontaneous rhesus macaque model of mismatch repair-deficient colorectal cancer. PLoS Genet. 2022;18(4):e1010163.
Khani P, Ghazi F, Zekri A, Nasri F, Behrangi E, Aghdam AM, et al. Keratins and epidermolysis bullosa simplex. J Cell Physiol. 2018;234(1):289–97.
Bolling MC, Lemmink HH, Jansen GH, Jonkman MF. Mutations in KRT5 and KRT14 cause epidermolysis bullosa simplex in 75% of the patients. Br J Dermatol. 2011;164(3):637–44.
Uitto J, Richard G. Progress in epidermolysis bullosa: from eponyms to molecular genetic classification. Clin Dermatol. 2005;23(1):33–40.
Johnson AL, Peterson SM, Terry MML, Ferguson B, Colgin LM, Lewis AD. Spontaneous KRT5 gene mutation in rhesus macaques (Macaca mulatta): a novel nonhuman primate model of epidermolysis bullosa simplex. Vet Pathol. 2020;57(2):344–8.
Acknowledgements
The authors acknowledge their fellow NHP New Model Development working group members for feedback and support.
Funding
This work was supported by R24 OD021324 and by P51 OD010425, P51 OD011092, P51 OD011104, P51 OD011106, P51 OD011107, P51 OD011132, and P51 OD011133.
Author information
Authors and Affiliations
Contributions
EJV, CH, ADL, JR, JAS, SMP, BF and KS wrote sections of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All studies using animals referenced in the above manuscript were completed in compliance with the “Guide for Care and Use of Laboratory Animals” and IACUC approved. Facilities are accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International (AAALAC) and are regularly assessed for compliance with the Animal Welfare Act of the United States.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vallender, E.J., Hotchkiss, C.E., Lewis, A.D. et al. Nonhuman primate genetic models for the study of rare diseases. Orphanet J Rare Dis 18, 20 (2023). https://doi.org/10.1186/s13023-023-02619-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-023-02619-3