Abstract
Phenylketonuria (PKU) is an inherited metabolic disease characterized by a defective conversion of phenylalanine (Phe) to tyrosine, potentially leading to Phe accumulation in the brain. Dietary restriction since birth has led to normal cognitive development. However, PKU patients can still develop cognitive or behavioral abnormalities and subtle neurological deficits. Despite the increasing evidence in the field, the assessment of neurocognitive, psychopathological, and neurological follow-up of PKU patients at different ages is still debated. The high interindividual variability in the cognitive outcome of PKU patients makes the specificity of the neurocognitive and behavioral assessment extremely challenging. In the present paper, a multidisciplinary panel of Italian PKU experts discussed different tools available for cognitive, psychopathological, and neurological assessment at different ages based on the existing literature and daily clinical practice. This study aims to provide evidence and a real-life-based framework for a specific clinical assessment of pediatric, adolescent, and adult patients affected by PKU.
Similar content being viewed by others
Background
Phenylketonuria (PKU) is a rare inherited metabolic disorder (IMD) caused by a deficiency in the phenylalanine (Phe) hydroxylase (PAH) enzyme, impairing the conversion of the amino acid Phe to tyrosine. The incidence of PKU in Europe is around 1/10,000–1/15,000 births, but it is higher in some countries, including Italy, where it reaches 1/4500 [1]. Deficiency of the hepatic PAH leads to a broad spectrum of hyperphenylalaninemia (HPA). HPAs are classified according to the treatment options: non-PKU HPA (Phe concentration ranging from 120 to 360 μmol/L) and PKU HPA (blood Phe concentration > 360 μmol/L) [2, 3]. The consequent accumulation of Phe to toxic concentrations in the brain results in severe clinical, neuropsychological, neurophysiologic, biochemical, and imaging alterations in untreated patients [4,5,6,7]. In particular, high Phe levels (> 600 μmol/L) could be associated with different neurotransmitters deficits and white matter alterations [8]. Thanks to the neonatal screening for PKU, patients can be treated in their early days while growing up, thus avoiding severe neurological deficits. However, a relevant percentage of patients treated early in their childhood still exhibit subtle cognitive deficits and psychosocial alterations in adulthood [9, 10]. In PKU patients treated early, prolonged high levels of Phe, particularly in adolescence, could negatively impact the individual’s cognitive functions [7, 11]. Unfortunately, nowadays, the chance of a pre-screening patient with a severe cognitive deficit arriving at the center is still possible.
There is a large consensus about the importance of analyzing the impact of neurocognitive deficits in PKU patients; however, it seems difficult to define a standardized and systematic neurocognitive patient assessment, as this strictly depends on age and severity of deficits [12].
The first-line treatment of PKU is based on a low Phe diet in combination with a protein substitute (mixtures of amino acids Phefree). Adherence to diet commonly decreases from childhood to adulthood; this event should be avoided, as hyperphenylalaninemia also impacts the adult brain [13, 14].
Until 2018, the only pharmacological therapy approved for PKU was the supplementation of tetrahydrobiopterin (BH4), an enzymatic co-factor of PAH. The tetrahydrobiopterin drug (Kuvan®) is the oral form of sapropterin dihydrochloride [15]. BH4 is not available worldwide, and only a proportion (estimated 30%) of PKU patients can respond to this treatment [16]. In 2018 and 2019, the US Food and Drug Administration (FDA) and the European Medicine Agency (EMA) approved pegvaliase (Palynziq®, BioMarin Pharmaceutical), respectively; pegvaliase is a pegylated recombinant Anabaena variabilis-derived Phe ammonia lyase able to reduce blood Phe concentration by substituting for Phe hydroxylase and converting Phe to ammonia and trans-cinnamic acid [17]. With pegvaliase, approved for patients ˃ 16 years old and with Phe levels > 600 μmol/L, patients can follow a diet with an amount of protein intake meeting the recommended dietary intake for the general population and even liberalize their diet [18, 19].
Outcomes in PKU and available tools for the assessment
Cognitive functions
Several single and multicenter studies showed that children, adolescents, and adults with PKU, even if treated from birth, may exhibit deficits in several domains [20,21,22,23], mainly executive functions (CFx) and attention [24,25,26,27]. CFx are responsible for goal-directed or future-oriented behavior, including initiating activity, impulse control, self-regulation, working memory, mental flexibility, planning, and organization ability [28]. The most consistent impairments of CFx in PKU patients have been observed in working memory, sustained attention, and inhibitory control [10, 29]. However, the degree of deficits and impairments broadly vary among different studies [10, 30]. This may be due to researchers' different ways of conceptualizing CFx and employing various CFx assessment tasks [31].
Several neuropsychological tests are available to assess cognitive performance in PKU patients but finding the best tool for the specific patient and impairment is not trivial, as no standard method for PKU patients exists. On the one hand, intellectual quotient (IQ) evaluation usually provides a reliable assessment of general cognitive functioning; on the other, it is not sensitive enough to detect minor neurocognitive dysfunctions [32]. As neuropsychological and behavioral alterations in PKU are heterogeneous in terms of degree and domains impaired, it is essential to identify the right tool for the right patient (according to the phenotype and age). Moreover, identifying a tool/pool of tools able to assess the overall burden of illness of PKU patients is crucial [33].
The central issue in assessing CFx in PKU populations is the lack of consistent use of valid and sensitive tests suitable for both children and adults [29]. Moreover, many traditional CFx tasks depend on multiple cognitive processes and show significant variability in the results. In the future, it will be essential to define a specific set of neuropsychological tasks to be used across international PKU centers [10, 14].
Quality of life, emotional and behavioral symptoms in PKU
PKU is associated with an increased incidence of emotional and behavioral problems [34,35,36] that could impair the Quality of Life (QoL) of patients [11]. Children and adults with PKU show emotional troubles such as low self-esteem, lower achievement motivation, decreased autonomy and reduced social competence. In contrast, adolescents and adults tend to have mood and anxiety disorders and social isolation [11, 37,38,39]. Patients with PKU often avoid meeting with friends, traveling, and performing sports, and recreational activities, with a significant impact on their QoL [40]. The management of a PKU patient should include an emotional and behavioral assessment and be aimed at identifying psychiatric disorders to allow for early treatment. The presence of emotional and behavioral troubles in PKU patients is possibly the consequence of growing up and living with a chronic disease [39].
Despite the evidence mentioned above, studies assessing the QoL of PKU patients provided conflicting results; in some cases, the results were similar to those of the general population [41,42,43]. In others, the studies showed a worsening of this parameter [44, 45]. Future studies, as recommended by European (EU) guidelines [14], should use the recently developed PKU-QoL questionnaire that is specifically designed to detect the impact of PKU on all aspects of a patient's life [46, 47].
Neurological outcome
Neurological signs (i.e., tremor, spastic paraparesis, and ataxia) are described in approximately 90% of untreated PKU patients and in a high proportion of late-treated PKU patients [48]. However, also in early treated PKU patients, some neurological signs, such as brisk tendon reflexes, clumsy motor coordination, and tremor, are frequently reported [47,48,49]. More recently, in a cohort of French adult PKU patients, the incidence of neurological complications has accounted for 5.1% [50].
Neuroimaging studies revealed that early-treated PKU adults exhibit a wide range of brain abnormalities, mostly related to white matter involvement [9]. Most patients exhibit mild to moderate white matter hyperintensities with no cortical atrophy or gray matter lesions [8, 9]. The degree of white matter alterations has been associated with mean Phe levels, but there are contradicting data addressing the relationship between dietary adherence and the severity of brain abnormalities [9]. No studies show a strict correlation between the degree of burden of white matter hyperintensities and the severity of cognitive or behavioral abnormalities, making magnetic resonance imaging (MRI) assessment questionable, except in a research setting. Nevertheless, the paper by Jaulent and colleagues recently showed that in a limited number of patients, who resumed or initiated a low-Phe diet, there was a partial/total regression of white matter abnormalities [50].
Indeed, the conventional brain MRI [(FLAIR/T2-weighted imaging and diffusion-weighted imaging (DWI)] is a powerful, readily available, noninvasive tool for detecting brain changes in PKU patients [9]. In line with this, EU guidelines and the Italian national consensus statement on management and pharmacological treatment of PKU suggest that neuroimaging examinations should be reserved only for those patients presenting with an atypical clinical course and/or unexpected neurological deficits, or for research purposes [3, 14].
Aim
Available scientific literature highlights the importance of a specific neurocognitive, psychopathological, and neurological assessment in PKU [9].
The different degrees of neurological and behavioral abnormalities of early-treated PKU patients (especially adults) are still debated, and the choice of the “best” neurocognitive test, sensitive to high levels of Phe, remains a challenge. To make things more complicated, a remarkable interindividual variability in the cognitive outcome and an inconsistent correlation between cognitive performances and biochemical control have been observed, suggesting the presence of an individual resilience or vulnerability to Phe in young early-treated adults [51].
Therefore, there is a significant need to reach an agreement on an appropriate set of tests according to the age of patients. The tasks should be suitable for use in everyday clinical practice. To fill this gap, a multidisciplinary group of Italian experts in the PKU field has assembled to propose a more comprehensive neurocognitive, psychopathological, and neurological assessment of PKU patients based on the existing literature and their clinical experience.
Methods
The panel of experts
The panelists, also authors of this study, gathered in two meetings. The six panelists work in Italian centers with extensive experience in PKU management and different medical specialties (neurology, neuropsychiatry, psychology, and inherited metabolic diseases). In particular, the panel was constituted of two adult neurologists (Alessandro Burlina and Andrea Pilotto), three psychologists (Stefania Caviglia, Chiara Cazzorla, Annamaria Dicintio), and one child neuropsychiatrist (Filippo Manti).
Expert opinion
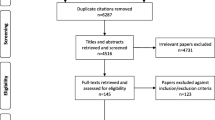
The Expert Opinion was shaped through two alignment meetings and one survey (Fig. 1). The first alignment meeting discussed the results of one preliminary questionnaire administered to participants to assess their agreement/disagreement on the main topics of PKU management. The questionnaire consisted of seven questions with a voting possibility from 1 (total disagreement) to 9 (complete agreement). Marks ≥ 5 were considered in agreement, while ˂ 5 were in disagreement. Results were then extensively discussed with the help of a professional facilitator.
Program of the Expert meetings. The expert panel included six experts, two adult neurologists, three psychologists, and one child neuropsychiatrist. The first alignment meeting discussed the agreement concerning the main topics of PKU management; the second meeting defined the main issues affecting the neurocognitive assessment. The survey defined the set of tests and the flow chart for the neurocognitive assessment of the patients
During the second alignment meeting, participants were interviewed about their setting and experience with the main issues affecting the neurocognitive assessment process in real-life PKU management.
The survey aimed to collect the recommendation of tools for neurocognitive and psychological follow-up of PKU patients in routine clinical evaluation.
Last, the experts were asked to define a chronological flow chart for PKU patients' cognitive, psychological, and neurological screening and follow-up.
Results
Level of agreement/disagreement of the experts on the principal topics of neurocognitive management of PKU patients
The participants discussed the results of the preliminary questionnaire in depth. The discussion focused mainly on questions correlating the frequency of neurological, neuropsychological, and psychiatric assessments with worsening school performance or comorbidities. At the end of the discussion, participants reached a high level of agreement on the neurocognitive assessment of PKU patients.
During the discussion, experts stated that the neurological assessment is to be performed at each visit. Visits are scheduled according to the age and needs of the patient. Neurological examinations should be performed repeatedly in children and adolescent, whereas, for adults, the guidelines suggest at least once a year in the absence of complications [3]. The frequency of the neurocognitive follow-up is increased according to the patient’s clinical and life conditions (causing clinical worsening/poor therapeutic compliance/comorbidity). IQ should be evaluated at 12 years and 18 years (as suggested by Burlina et al. [3]); a cognitive evaluation of pediatric patients could be necessary, for example, before starting the primary school. As already outlined by the national consensus document on PKU's management and pharmacological treatment, the multidisciplinary care team should include neuropsychiatrists, psychiatrists, psychologists, neurologists, metabolic pediatricians, and dietitians for the routine evaluation [3].
Main issues affecting the cognitive, psychological, and neurological assessment process in real-life management of PKU patients
The main issues affecting the neurocognitive, psychopathological, and neurological assessment process in the daily clinical practice of the experts were assessed during the second session (Table 1).
The panel agreed that while for pediatric and adolescent patients the main obstacles for adequate neurocognitive and psychopathological evaluation are logistical and operational, for adults there are factors related to acceptance of the medical condition, self-image, and the patient's perception/predisposition to risk.
Tools for the cognitive, psychological, and neurological assessment of PKU patients according to their age
In choosing the examinations, the experts considered, on the one hand, the clinical significance and reliability of the test and, on the other, the feasibility of the examination in a context of daily clinical practice. The list was discussed and agreed by the experts.
Table 2 outlines the tests suggested for the clinical evaluation of PKU patients. Tests were subdivided for the pediatric, adolescent, and adult patients.
The tests to assess the IQ selected by the panel of experts are universally recognized for the assessment of intellectual abilities and allow both clinical and diagnostic evaluation.
The rationale for the selection of the tests for the assessment of the CFx, was their good level of acceptance by patients and the specificity according to patient age. The experts selected tests which allows to evaluate specific skills. All selected tests are already widely used in the scientific literature for the analysis of other non-inherited metabolic diseases.
For the behavioral and emotional profile, experts chose the ASEBA scale (CBCL 1½-5yy; CBCL 6-18yy; YSR; ASR), one of the most widely used tool and the BDI and STAI scales.
For the QoL assessment, the panel of experts suggested the use PKU-QoL for all ages considered, as it was developed and validated specifically for patients with PKU [45].
The experts selected the age-specific tests according to five criteria: a) specificity by age, b) ability to detect dysfunctions, c) specificity for particular cases (e.g., foreign patients who do not have a good command of Italian), d) ease of administration, e) ability in detecting disease-related changes in QoL. As expected, no test met all five criteria; the main criterion for the choice of the individual task in each age group is listed below.
Pediatric patient
-
test specificity by age: Griffiths-III, WPPSI-IV, WISC-IV, BRIEF-P, BRIEF-2, VMI, CBCL 1 ½-5, CBCL 6-18, Bells Test;
-
ability to detect dysfunctions: WPPSI-IV, WSCT, TOL, ROCF copy and memory, DSST, VMI, DGS (Forward and Reverse), Bells Test, Semantic fluency, Phonemic fluency, Word List, CBCL 1 ½-5, CBCL 6-18;
-
test specificity for particular cases: LEITER-3;
-
ease of administration: BRIEF-P, BRIEF-2, DSST, DGS (Forward and Reverse), Bells Test, Semantic fluency, Phonemic fluency;
-
specificity of the test in detecting disease-related changes: PKU-QoL.
Adolescent patient
-
test specificity by age: WISC-IV, WAIS-IV, BRIEF-2, VMI, CBCL 6-18, YSR;
-
ability to detect dysfunctions: WISC-IV, WAIS-IV, WSCT, TMT A-B, TOL, Semantic fluency, Phonemic fluency, ROCF copy and memory, Corsi Test (Forward and Reverse), DSST, TMT A, VMI, DGS (Forward and Reverse), RAVLT, Story Recall Test, CBCL 6-18, YSR;
-
test specificity for particular cases: LEITER-3;
-
ease of administration: BRIEF-2, TMT A-B, Semantic fluency, Phonemic fluency, DSST, TMT A, DGS (Forward and Reverse), Story Recall Test;
-
specificity of the test in detecting disease-related changes: PKU-QoL.
Adult patient
-
test specificity by age: WAIS-IV, BRIEF-Adult, ASEBA/ASR, BDI-II, STAI;
-
ability to detect dysfunctions: WAIS-IV, WCST, TMT A-B, TOL, Semantic fluency, Phonemic fluency, SCWT, ROCF copy and memory, Corsi Test (Forward and Reverse), DSST, TMT-A, VMI, DGS (Forward and Reverse), RAVLT, Story Recall Test, ASEBA/YSR/ASR, BDI-II, STAI;
-
test specificity for particular cases: LEITER-3;
-
ease of administration: BRIEF-Adult, TMT A-B, Semantic fluency, Phonemic fluency, DSST, TMT-A, DGS (Forward and Reverse), Story Recall Test;
-
specificity of the test in detecting disease-related changes: PKU-QoL.
Chronological flow chart diagram for cognitive, psychological, and neurological screening and follow-up of PKU patients
Figures 2 and 3 show a step-by-step chronological program proposed by the six experts involved in the study for the follow-up of PKU patients.
Discussion
This paper intends to provide practical recommendations for the assessment of cognitive, psychological, and neurological outcomes in pediatric, adolescent, and adult patients with PKU. Since PKU is a disease characterized by subtle and heterogeneous neuropsychological and behavioral abnormalities, a specific set of cognitive tests should be implemented for PKU patients of different ages [27, 40]. The purpose of this paper was to reach an agreement on the selection of a panel of validated tests which could be administered to PKU patients from the pediatric age to adulthood. In the literature, only the PKU-QoL has been specifically developed to measure the QoL in PKU patients [46]. Therefore, for cognitive examination, we decided to have a different approach. We selected the most appropriate tests to analyze specific functions, which could be altered in PKU patients according to the impaired domains and corresponding to the age of the patients. Therefore, the major advantage of this panel of tests is that it focuses on specific domains, for a personalized approach to the PKU patient. We also considered the possibility to have the same test available in other local languages, to allow putative comparison of the analyzed cohorts of patient among different centers and countries.
For the neurological assessment, we strongly believe that a complete neurological examination should always be performed, especially for adult PKU patients and at least at the first visit.
We have identified two limitations in our work. First, the selection of a panel of tests has been necessarily done within a panel of tests developed for other medical settings rather than cognitive and psychological assessment given that no specific tests for PKU patients have been developed so far. However, the final choice was the result of the expert panelists who had previously applied these tests several times during their clinical practice with PKU patients. Second, our group involved only Italian centers, which may just reflect our clinical experience and approach to the PKU patient.
We hope this paper may stimulate the discussion on the most appropriate neuropsychological assessment of PKU patients, thus helping clinicians to better define the best clinical monitoring and improve their therapeutic management.
Availability of data and materials
Data sharing not applicable to this article as no datasets were produced or analyzed during the study.
Change history
03 March 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13023-023-02644-2
References
Hillert A, Anikster Y, Belanger-Quintana A, Burlina A, Burton BK, Carducci C, et al. The genetic landscape and epidemiology of phenylketonuria. Am J Hum Genet. 2020;107(2):234–50.
van Spronsen FJ, van Wegberg AM, Ahring K, Bélanger-Quintana A, Blau N, Bosch AM, et al. Key European guidelines for the diagnosis and management of patients with phenylketonuria. Lancet Diabetes Endocrinol. 2017;5(9):743–56.
Burlina A, Biasucci G, Carbone MT, Cazzorla C, Paci S, Pochiero F, et al. Italian national consensus statement on management and pharmacological treatment of phenylketonuria. Orphanet J Rare Dis. 2021;16(1):476.
Blau N, van Spronsen FJ, Levy HL. Phenylketonuria. Lancet. 2010;376(9750):1417–27.
Mitchell JJ, Trakadis YJ, Scriver CR. Phenylalanine hydroxylase deficiency. Genet Med. 2011;13(8):697–707.
Pilotto A, Zipser CM, Leks E, Haas D, Gramer G, Freisinger P, et al. Phenylalanine effects on brain function in adult phenylketonuria. Neurology. 2021;96(3):e399–411.
Waisbren SE, Noel K, Fahrbach K, Cella C, Frame D, Dorenbaum A, et al. Phenylalanine blood levels and clinical outcomes in phenylketonuria: a systematic literature review and meta-analysis. Mol Genet Metab. 2007;92(1–2):63–70.
Anderson PJ, Leuzzi V. White matter pathology in phenylketonuria. Mol Genet Metab. 2010;99(Suppl 1):S3-9.
Burlina AP, Lachmann RH, Manara R, Cazzorla C, Celato A, van Spronsen FJ, et al. The neurological and psychological phenotype of adult patients with early-treated phenylketonuria: a systematic review. J Inherit Metab Dis. 2019;42(2):209–19.
Hofman DL, Champ CL, Lawton CL, Henderson M, Dye L. A systematic review of cognitive functioning in early treated adults with phenylketonuria. Orphanet J Rare Dis. 2018;13(1):150.
Ashe K, Kelso W, Farrand S, Panetta J, Fazio T, De Jong G, et al. Psychiatric and cognitive aspects of phenylketonuria: the limitations of diet and promise of new treatments. Front Psychiatry. 2019;10:561.
Cazzorla C, Bensi G, Biasucci G, Leuzzi V, Manti F, Musumeci A, et al. Living with phenylketonuria in adulthood: the PKU ATTITUDE study. Mol Genet Metab Rep. 2018;16:39–45.
Koch R, Burton B, Hoganson G, Peterson R, Rhead W, Rouse B, et al. Phenylketonuria in adulthood: a collaborative study. J Inherit Metab Dis. 2002;25(5):333–46.
van Wegberg AMJ, MacDonald A, Ahring K, Bélanger-Quintana A, Blau N, Bosch AM, et al. The complete European guidelines on phenylketonuria: diagnosis and treatment. Orphanet J Rare Dis. 2017;12(1):162.
Muntau AC, Röschinger W, Habich M, Demmelmair H, Hoffmann B, Sommerhoff CP, et al. Tetrahydrobiopterin as an alternative treatment for mild phenylketonuria. N Engl J Med. 2002;347(26):2122–32.
Ho G, Christodoulou J. Phenylketonuria: translating research into novel therapies. Transl Pediatr. 2014;3(2):49–62.
Mahan KC, Gandhi MA, Anand S. Pegvaliase: a novel treatment option for adults with phenylketonuria. Curr Med Res Opin. 2019;35(4):647–51.
Longo N, Dimmock D, Levy H, Viau K, Bausell H, Bilder DA, et al. Evidence- and consensus-based recommendations for the use of pegvaliase in adults with phenylketonuria. Genet Med. 2019;21(8):1851–67.
Zori R, Ahring K, Burton B, Pastores GM, Rutsch F, Jha A, et al. Long-term comparative effectiveness of pegvaliase versus standard of care comparators in adults with phenylketonuria. Mol Genet Metab. 2019;128(1–2):92–101.
Araujo GC, Christ SE, Steiner RD, Grange DK, Nardos B, McKinstry RC, et al. Response monitoring in children with phenylketonuria. Neuropsychology. 2009;23(1):130–4.
Diamond A, Prevor MB, Callender G, Druin DP. Prefrontal cortex cognitive deficits in children treated early and continuously for PKU. Monogr Soc Res Child Dev. 1997;62(4):1–208.
Welsh MC, Pennington BF, Ozonoff S, Rouse B, McCabe ER. Neuropsychology of early-treated phenylketonuria: specific executive function deficits. Child Dev. 1990;61(6):1697–713.
Sharman R, Sullivan K, Young R, McGill J. Biochemical markers associated with executive function in adolescents with early and continuously treated phenylketonuria. Clin Genet. 2009;75(2):169–74.
Bilder DA, Noel JK, Baker ER, Irish W, Chen Y, Merilainen MJ, et al. Systematic review and meta-analysis of neuropsychiatric symptoms and executive functioning in adults with phenylketonuria. Dev Neuropsychol. 2016;41(4):245–60.
Cappelletti S, Cotugno G, Goffredo BM, Nicolò R, Bernabei SM, Caviglia S, et al. Cognitive findings and behavior in children and adolescents with phenylketonuria. J Dev Behav Pediatr. 2013;34(6):392–8.
Jahja R, Huijbregts SCJ, de Sonneville LMJ, van der Meere JJ, Legemaat AM, Bosch AM, et al. Cognitive profile and mental health in adult phenylketonuria: a PKU-COBESO study. Neuropsychology. 2017;31(4):437–47.
Aitkenhead L, Krishna G, Ellerton C, Moinuddin M, Matcham J, Shiel L, et al. Long-term cognitive and psychosocial outcomes in adults with phenylketonuria. J Inherit Metab Dis. 2021;44(6):1353–68.
Anderson P. Assessment and development of executive function (EF) during childhood. Child Neuropsychol. 2002;8(2):71–82.
van Spronsen FJ, Huijbregts SC, Bosch AM, Leuzzi V. Cognitive, neurophysiological, neurological and psychosocial outcomes in early-treated PKU-patients: a start toward standardized outcome measurement across development. Mol Genet Metab. 2011;104(Suppl):S45-51.
Moyle JJ, Fox AM, Arthur M, Bynevelt M, Burnett JR. Meta-analysis of neuropsychological symptoms of adolescents and adults with PKU. Neuropsychol Rev. 2007;17(2):91–101.
Stemerdink NB. Comments on neuropsychological approaches to treatment policy issues in phenylketonuria. Eur J Pediatr. 2000;159(Suppl 2):S87–8.
Lezak M. Neuropsychological assessment. 3rd ed. New York: Oxford University Press; 1995.
Quinn J, Georgiadis A, Lewis HB, Jurecki E. Measuring burden of illness in phenylketonuria (PKU): development of the PKU symptom severity and impacts scale as a robust patient-reported outcome. Adv Ther. 2021;66:1–21.
Vilaseca MA, Lambruschini N, Gómez-López L, Gutiérrez A, Fusté E, Gassió R, et al. Quality of dietary control in phenylketonuric patients and its relationship with general intelligence. Nutr Hosp. 2010;25(1):60–6.
Romani C, Palermo L, MacDonald A, Limback E, Hall SK, Geberhiwot T. The impact of phenylalanine levels on cognitive outcomes in adults with phenylketonuria: effects across tasks and developmental stages. Neuropsychology. 2017;31(3):242–54.
Pietz J, Dunckelmann R, Rupp A, Rating D, Meinck HM, Schmidt H, et al. Neurological outcome in adult patients with early-treated phenylketonuria. Eur J Pediatr. 1998;157(10):824–30.
Brumm VL, Bilder D, Waisbren SE. Psychiatric symptoms and disorders in phenylketonuria. Mol Genet Metab. 2010;99(Suppl 1):S59-63.
Gentile JK, Ten Hoedt AE, Bosch AM. Psychosocial aspects of PKU: hidden disabilities—a review. Mol Genet Metab. 2010;99(Suppl 1):S64–7.
Manti F, Nardecchia F, Chiarotti F, Carducci C, Carducci C, Leuzzi V. Psychiatric disorders in adolescent and young adult patients with phenylketonuria. Mol Genet Metab. 2016;117(1):12–8.
Quinn J, Georgiadis A, Lewis HB, Jurecki E. Measuring burden of illness in phenylketonuria (PKU): development of the PKU symptom severity and impacts scale as a robust patient-reported outcome. Adv Ther. 2022;39:971–91.
Bik-Multanowski M, Didycz B, Mozrzymas R, Nowacka M, Kaluzny L, Cichy W, et al. Quality of life in noncompliant adults with phenylketonuria after resumption of the diet. J Inherit Metab Dis. 2008;31(Suppl 2):S415–8.
Douglas TD, Ramakrishnan U, Kable JA, Singh RH. Longitudinal quality of life analysis in a phenylketonuria cohort provided sapropterin dihydrochloride. Health Qual Life Outcomes. 2013;11:218.
Gassió R, Campistol J, Vilaseca MA, Lambruschini N, Cambra FJ, Fusté E. Do adult patients with phenylketonuria improve their quality of life after introduction/resumption of a phenylalanine-restricted diet? Acta Paediatr. 2003;92(12):1474–8.
Demirdas S, Maurice-Stam H, Boelen CC, Hofstede FC, Janssen MC, Langendonk JG, et al. Evaluation of quality of life in PKU before and after introducing tetrahydrobiopterin (BH4); a prospective multi-center cohort study. Mol Genet Metab. 2013;110(Suppl):S49-56.
Cotugno G, Nicolò R, Cappelletti S, Goffredo BM, Dionisi Vici C, Di Ciommo V. Adherence to diet and quality of life in patients with phenylketonuria. Acta Paediatr. 2011;100(8):1144–9.
Regnault A, Burlina A, Cunningham A, Bettiol E, Moreau-Stucker F, Benmedjahed K, et al. Development and psychometric validation of measures to assess the impact of phenylketonuria and its dietary treatment on patients’ and parents’ quality of life: the phenylketonuria—quality of life (PKU-QOL) questionnaires. Orphanet J Rare Dis. 2015;10:59.
Cazzorla C, Cegolon L, Burlina AP, Celato A, Massa P, Giordano L, et al. Quality of life (QoL) assessment in a cohort of patients with phenylketonuria. BMC Public Health. 2014;14:1243.
Pietz J. Neurological aspects of adult phenylketonuria. Curr Opin Neurol. 1998;11(6):679–88.
Pérez-Dueñas B, Valls-Solé J, Fernández-Alvarez E, Conill J, Vilaseca MA, Artuch R, et al. Characterization of tremor in phenylketonuric patients. J Neurol. 2005;252(11):1328–34.
Jaulent P, Charriere S, Feillet F, Douillard C, Fouilhoux A, Thobois S. Neurological manifestations in adults with phenylketonuria: new cases and review of the literature. J Neurol. 2020;267(2):531–42.
Manti F, Nardecchia F, Paci S, Chiarotti F, Carducci C, Carducci C, et al. Predictability and inconsistencies in the cognitive outcome of early treated PKU patients. J Inherit Metab Dis. 2017;40(6):793–9.
Acknowledgements
The authors are grateful to Akros Bioscience for medical writing assistance, Damiano Sergio Massaro (BioMarin) for his supervision and contribution as project manager, and to Alessandro Urbani (external consultant) for methodological support and facilitation of discussions.
Funding
BioMarin funded the advisory board and the development of this manuscript. Writing and editorial services were provided by Akros Bioscience, Pomezia (RM) Italy and funded by BioMarin International Ltd.
Author information
Authors and Affiliations
Contributions
FM and AB conducted the discussion in consensus conferences. Each author gave peculiar contribution to the development and discussion of statements related to the clinical topics analyzed during the working group. AP and AB were responsible for the development of the neurologic issue; FM, SC, CC, and AD were responsible for the development of the cognitive and psychological issues. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors received financial reimbursement from BioMarin at fair market value for their participation in virtual advisory boards. The manuscript was developed by the authors and reviewed by BioMarin. BioMarin provided project management; editorial and writing support was provided by an independent medical communication agency. F. Manti received advisory board honoraria from BioMarin; A. Pilotto is supported by IMI H2020 initiative (MI2-2018-15-06) paid to the university of Brescia Italian Ministry of Health paid to the university of Brescia; he received Lectures honoraria from Bial, BioMarin, Abbvie, Chiesi and Zambon pharmaceuticals-payment made to A. Pilotto as an individual; he received research support from Bial, BioMarin, Abbvie, Chiesi and Zambon pharmaceuticals-payment made to the Institution University of Brescia; S. Caviglia received advisory board honoraria from BioMarin; A. Dicintio received advisory board honorarium and speaker fee from BioMarin; C. Cazzorla received advisory board honorarium from BioMarin; A. Burlina received advisory board honorarium from BioMarin; A. Burlina received advisory board and lectures honoraria from Amicus Therapeutics, BioMarin, Chiesi, Freeline Therapeutics, PIAM, Sanofi, Takeda.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
“The original version of this article was revised: Table 2, column “Pediatric Patient”/DGS (Forward and Reverse); Corsi Test (Forward and Reverse) has been corrected to - “DGS (Forward and Reverse)”. Reference 40. Quinn J, Georgiadis A, Lewis HB, Jurecki E. Measuring burden of illness in phenylketonuria (PKU): development of the PKU symptom severity and impacts scale as a robust patient-reported outcome. Adv Ther. 2021;6:66 has been corrected to: 40. Quinn J, Georgiadis A, Lewis HB, Jurecki E. Measuring burden of illness in phenylketonuria (PKU): development of the PKU symptom severity and impacts scale as a robust patient-reported outcome. Adv Ther. 2022;39:971-91.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Manti, F., Caviglia, S., Cazzorla, C. et al. Expert opinion of an Italian working group on the assessment of cognitive, psychological, and neurological outcomes in pediatric, adolescent, and adult patients with phenylketonuria. Orphanet J Rare Dis 17, 443 (2022). https://doi.org/10.1186/s13023-022-02488-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-022-02488-2