Abstract
Background
Origin of anorectal malformations (ARM) are considered multifactorial. Several genetic and non-genetic risk factors are discussed in literature. Maternal periconceptional medical drug use as possible risk factor, however, has not been reviewed systematically.
Methods
Studies published between 1977 and April 2017 were reviewed through systematic search in PubMed, ISI Web of Knowledge and Scopus databases. Furthermore, related and cross-referencing publications were reviewed. Pooled odds ratios (95% confidence intervals) were determined to quantify associations of maternal periconceptional use of folic acid, multivitamins, anti-asthma medication (separated in any anti-asthma medication, inhaled corticosteroids and salbutamol), thyroid hormone supplements, psychiatric drugs (separated in antidepressants, any selective serotonin reuptake inhibitors [SSRI], sertraline, citalopram, fluoxetine, paroxetine, hypnotics and benzodiazepine) and aspirin with ARM using meta-analyses.
Results
Thirty-seven studies that reported on the association between maternal periconceptional drug intake and infants born with ARM were included in this review. These were conducted in the United States of America (n = 14), Sweden (n = 6), Hungary (n = 5), Germany (n = 3), the Netherlands (n = 3), Denmark (n = 2), France (n = 2), Norway (n = 1) and the UK (n = 1). However, only few of these studies reported on the same risk factors. Studies were heterogeneous with respect to case numbers, period ingestion of medical drug use, control selection and adjustment for covariates. Consistently increased risks were observed for any anti-asthma medication, and hypnotics and benzodiazepine, but not for folic acid, multivitamins, inhaled corticosteroids, salbutamol, thyroid hormone supplements, antidepressants, any SSRI, sertraline, citalopram, fluoxetine, paroxetine and aspirin. In meta-analyses, pooled odds ratios (95% confidence intervals) for any anti-asthma medication, and hypnotics and benzodiazepine were 1.64 (1.22–2.21), and 2.43 (1.03–5.73), respectively.
Conclusion
Evidence on maternal drug use before conception and during pregnancy as risk factor for ARM from epidemiological studies is still very limited. Nevertheless, the few available studies indicate any anti-asthma medication, and hypnotics and benzodiazepine to be associated with increased risks. Further, ideally large-scale multicenter and register-based studies are needed to clarify the role of maternal drug intake for the development of ARM.
Similar content being viewed by others
Background
Anorectal malformations (ARM) are rare birth defects concerning anus and rectum. Approximately 1 in 2500 to 1 in 5000 new born babies are affected [1,2,3]. Different degrees of severity are distinguished, ranging from mild anal stenosis over anal atresia with or without fistula to persistent cloaca or even cloacal exstrophy [4]. Furthermore, approximately 64% of all ARM patients have one or more additional extra-anal anomalies [5]. ARM affect several socioeconomic and ethnic groups [6,7,8,9,10]. Boys seem to be at a slightly higher risk than girls (1.3:1) [11]. It is assumed that the defects occur during the 4th to 8th week of fetal development [12,13,14,15,16,17]. Knowledge about the causes, however, is still sparse. There are assumptions that genetic factors encourage the development of ARM [18,19,20,21,22,23,24,25], but no single gene or chromosomal locus has been identified so far as the cause of all or even of a majority of ARM. In recent years, several potential non-genetic risk factors for ARM were assessed, with often contrary results, among them prenatal exposures of the parents to lifestyle factors (tobacco, alcohol, caffeine, illicit drugs) and occupational hazards [26], to chronic diseases [27, 28], fever [27, 29] and injuries [30]. Maternal overweight, obesity and diabetes, however, indicate to be associated with increased risks for ARM [26]. In addition, a relationship between a single umbilical artery and ARM is suspected [31]. Assisted reproductive techniques also pose a strongly increased risk for ARM [32,33,34,35,36,37,38], but it remains unclear whether the procedure itself or underlying parental infertility cause the defects. Besides these non-genetic factors, the influence of maternal drug intake before and during pregnancy, such as vitamin A overdose [39] or deficiency [40], multivitamin [27], folic acid [27, 41], anti-asthmatic drugs [42] or benzodiazepine lorazepam [43], is subject to ongoing debate.
We conducted a systematic review and meta-analysis of epidemiological studies to summarize current evidence on the relationship between maternal drug intake and ARM, and to identify knowledge deficits that need to be addressed in future research.
Methods
Identification of studies and study selection
A literature search was carried out to identify epidemiological studies assessing the association between maternal medical drug intake before conception and during the first trimester of pregnancy and anorectal malformations. Relevant studies published in English were systematically searched in PubMed, ISI Web of Knowledge and Scopus databases by using various combinations of the following terms: (congenital malformation(s), congenital abnormality, congenital abnormalities, birth defect(s), anorectal malformation(s), anorectal atresia, anal atresia, imperforate anus) AND (medical drug(s), drugs(s), medication, medicament, medicine, pharmaceutical, dietary supplements, folic acid, (multi-)vitamins, vitamin A, vitamin B, vitamin C, iron). Duplicate articles were deleted. Each title and abstract was checked for relevance. The full text was reviewed if the abstract indicated that the article reported an association between ARM and maternal use of medical drugs. Furthermore, the identified articles were reviewed for related articles and cross-referring publications.
Inclusion criteria
Articles were included if they reported on associations of anorectal malformations with maternal medical drug intake. When available, data of ARM infants with isolated anomalies (no additional major defects) were preferred to data of ARM infants with multiple defects. Articles were excluded if the reported number of ARM cases was less than two. ARM infants analyzed only in a group with other anomalies like intestinal or tracheo-esophageal atresias were also excluded because of concern that associations of risk factors with these anomalies might be different from associations with ARM. In addition, articles describing medical drug use in animal models were also excluded. Searches were restricted to English-language articles.
Data extraction
Two reviewers independently assessed the articles and extracted the following key information in a standardized manner: first author, year, country, study design, characteristics of the study population, period of data acquisition, assessed medical drug(s) and the respective measures of odds ratio or risk ratio (see below), as well as covariates adjusted for in the analysis. Initial disagreements on classifications of study characteristics were resolved by discussion within the team of authors. Such disagreements included the presentation of case and control numbers in some studies as well as the presentation of the maternal age at the time of data acquisition. In such a case, the authors came together and discussed the topics. As one result, footnotes were included in Table 1 to offer the opportunity to present case and control numbers even more accurately.
Associations between maternal medical drug intake and ARM are presented by odds ratios (OR) and their 95% confidence intervals (CI). Alternatively, reported risk ratios (RR) are shown. In one case, only prevalence values were presented. Unadjusted values were recalculated by the Review Manager Software, version 5.3.5 (The German Cochrane Centre, Freiburg, Germany) to validate the results. When measures of associations were not explicitly reported, they were derived from data provided in the articles.
Meta-analyses
Meta-analyses were performed for risk factors for which results were available from at least three studies. Heterogeneity was assessed by the χ2 and I2 statistics. When the number of studies is low or when sample sizes are small, the power of the χ2 test is low. The I2 measure describes the proportion of total variation in effect estimates across studies that is due to heterogeneity rather than sampling error [44]. Fixed and random effects models were calculated by the R© software, version 3.2.4 (The R Foundation for Statistical Computing, Vienna) using standard meta-analysis methods. The fixed effects model was used to estimate the variance of the summary odds ratio when study heterogeneity was low (I2 ≤ 25) and the random effects model when study heterogeneity was moderate to high (I2 > 25) [45, 46]. Indication of publication bias was assessed by Begg and Mazumdar rank correlation test [47] and Egger’s test [48] (P < 0.1).
Results
Literature search result
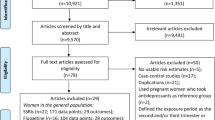
In total, 146,491 articles were found (Fig. 1). After removal of 52,657 duplicates, 93,834 titles and abstracts were reviewed. Sixty-three articles appeared to be potentially relevant for inclusion in the review. Of these, two articles were excluded because they were published in Spanish or French, seven articles because they described the use of medical drugs in animal models, five articles because of too low case numbers (n < 2), nine articles because they referred to results of already selected articles and further three articles because they reported on ARM cases analyzed in a group with other anomalies. Finally, 37 articles were included in the review. Among the included studies, 10 provided data on the association of ARM with maternal periconceptional dietary supplements, including folic acid, iron and (multi-)vitamin use, five to asthma medication, three to thyroid medication, nine to psychiatric drugs, four to painkiller, four to anti-infectives, two to drugs against nausea and vomiting, two to sexual hormones and further two to other medical drugs.
Studies included in this review
Details on the 37 studies, which were published from 1977 to April 2017, are shown in Table 1. Studies were mainly conducted in the USA (n = 14). The remaining studies were conducted in Sweden (n = 6), Hungary (n = 5), Germany (n = 3), the Netherlands (n = 3), Denmark (n = 2), France (n = 2), Norway (n = 1) and the UK (n = 1). Recruitment was population−/national-based in 30 studies, province-based in one study and hospital-based in four studies. For data acquisition, two studies relied on register-based data [49, 50]. Data acquisition periods varied from 2 years [28, 51] to 22 years [43].
Case numbers ranged from six ARM cases [43] to 799 ARM cases [52]. Children with known chromosomal anomalies were excluded in 20 studies [27, 28, 41, 42, 49, 50, 53,54,55,56,57,58,59,60,61,62,63,64,65,66]. Twenty-one studies used infants with no (major) birth defects as control group [6, 27, 28, 41, 54, 55, 58,59,60,61,62,63,64,65,66,67,68,69,70,71,72] and four studies used malformed infants with other anomalies than ARM [50, 53, 73, 74]. Controls of the remaining 11 studies were all infants born in the same settings during the respective study period [42, 43, 49, 51, 52, 56, 57, 75,76,77,78]. One study only reported on prevalences and did not use a control group [79]. Only nine studies examined the association between maternal medical drug intake and ARM infants with isolated anomalies [41, 53, 57, 59, 65, 69,70,71, 73].
Most of the studies asked for a period ingestion of medical drug use before and during pregnancy. However, there was no unique definition of the “periconceptional” period of time, varying from 3 months before conception until the end of the third month in pregnancy [6, 28, 53, 61, 66] or through the last month of pregnancy [57], from 2 months before conception though 1 month in pregnancy [33], from 4 weeks before conception until 10 weeks after conception [27, 41] or until 3 months in pregnancy [54, 59, 63, 64, 68], from 2 weeks before conception until 2 weeks after conception [69] or until 4 weeks up to 3 months after conception [65, 71]. Other studies asked there participants for a period ingestion of medical drug use in the first trimester of pregnancy, defined as start of pregnancy until 12 weeks after pregnancy [42, 43, 49, 51, 58, 60, 62, 67, 68, 73, 78] or as the period from the first day of the last menstrual period up to the 12th week of gestation [50, 52], or in general for the use in early pregnancy [56, 75,76,77] or through the whole pregnancy [70, 74, 79]. Dosage was reported in 12 studies [49, 57, 59, 62, 65,66,67,68,69,70,71, 78], exact timing/frequency and/or duration in 16 studies [49, 54, 57,58,59,60,61,62,63, 65,66,67, 69,70,71, 78]. The exact international World Health Organization’s Anatomical Therapeutic Chemical (ATC) classification [80, 81] was used in seven studies [50, 52, 56, 73, 75, 76, 78]. In addition, nine studies linked all medication to the Slone Drug Dictionary [82], a computerized coding system [54, 57,58,59, 61,62,63, 67, 68].
Findings for the reviewed risk factors
Study results as well as the covariates adjusted for are shown in Tables 2, 3, 4, 5, 6, 7, 8, 9 and 10.
Dietary supplements
Ten studies reported on the association between maternal use of dietary supplements before or during pregnancy and infants born with an anorectal malformation, among them seven studies on folic acid, six studies on multivitamins, and each one study on vitamin E and iron intake (Table 2).
The study by Czeizel et al. [66] reported on a significantly protective association of folic acid supplementation with ARM when mothers used it in the second month of gestation (ORcrude, 0.4; 95% CI, 0.17–0.88; P = 0.01). In contract, the use of folic acid in the first month of gestation was not significant (ORcrude, 0.5; 95% CI, 0.17–1.23; P = 0.12). In the study by Myers et al. [51] different ARM groups were used. There was a significantly protective association with all ARM cases (RRcrude, 0.5; 95% CI, 0.29–0.88) and a marginally protective association with ARM cases with no additional external anomalies (RRcrude, 0.5; 95% CI, 0.24–1.04). After adjustment for maternal age the association with all ARM cases was weakened (RRadj, 0.6; 95% CI, 0.33–1.07) and the association with ARM cases with no additional external anomalies became insignificant (RRadj, 0.7; 95% CI, 0.31–1.42).
A marginally increased risk for multivitamins was only reported in the study by van Rooij et al. [27] (ORcrude, 1.6; 95% CI, 1.0–2.7; P = 0.09). No other study could confirm an association with ARM. The study by Gilboa et al. [57] categorized maternal vitamin E intake during and before pregnancy into three classes (daily total intake of 5.13–7.79 mg, daily total intake of 7.80–14.19 mg, daily total intake of > 14.19 mg). A marginally increased risk was observed for the exposure group 7.80–14.19 mg per day only (ORadj, 1.7; 95% CI, 1.01–2.72). There was no association with maternal iron intake before or during pregnancy.
The result of the meta-analysis on the association between maternal use of folic acid and ARM infants is shown in Fig. 2. From the study by Zwink and Choinitzki et al. [53] we used the OR calculated with the group of control infants with esophageal atresia with or without tracheoesophageal fistula, from the study by Czeizel et al. [66] the OR calculated for supplementation in the second month of gestation as ARM is known to develop between the 5th–8th week of gestation, from the study by Wijers et al. [41] the OR calculated for all ARM cases, and from the study by Myers et al. [51] the RR calculated with all ARM cases. The I2 statistic indicated heterogeneity across studies (χ2 = 7.71; P = 0.26; I2 = 22.2%). The estimated heterogeneity variance was tau2 = 0.0226. In meta-analysis, no significant association was observed in pooled analyses using the fixed effects model (OR, 0.93; 95% CI, 0.77–1.13; P = 0.47). There was a weak evidence of publication bias (Kendall’s tau = − 1.65, P = 0.10; Egger’s t value = − 1.72, P = 0.15).
The result of the meta-analysis on the association between maternal use of multivitamins and ARM infants is shown in Fig. 3. From the study by Zwink and Choinitzki et al. [53] we used the OR calculated with the group of control infants with esophageal atresia with or without tracheoesophageal fistula. The I2 statistic indicated low heterogeneity across studies (χ2 = 6; P = 0.31; I2 = 16.7%). The estimated heterogeneity variance was tau2 = 0.0523. No significant association was observed in pooled analyses using a fixed effects model (OR, 1.24; 95% CI, 0.87–1.78; P = 0.23). There was no evidence of publication bias (Kendall’s tau = − 1.32, P = 0.19; Egger’s t value = − 1.61, P = 0.18).
Asthma medication
Five studies reported on the association between maternal use of asthma medication before or during pregnancy and infants born with an anorectal malformation (Table 3). The use of any anti-asthma medication showed a significant association with ARM in the studies by Källén and Otterblad Olausson [42] (ORadj, 1.7; 95% CI, 1.11–2.56) and Garne et al. [73]. In the latter study two different control groups were used. Both, the comparison of ARM with non-chromosomal anomalies (ORadj, 1.6; 95% CI, 1.08–2.51) and the comparison of ARM with chromosomal anomalies (ORadj, 2.0; 95% CI, 1.30–3.20) was significant for any anti-asthma medication. In contrast, the study by Zwink and Choinitzki et al. [53] could not find an association with ARM. The study by Lin et al. [59] observed an association between anti-inflammatory use and ARM (ORadj, 2.1; 95% CI, 1.09–4.12).
The use of inhaled corticosteroids showed a significant risk for ARM in the study by Garne et al. [73], independent of the used control group (ARM vs. non-chromosomal anomalies: ORcrude, 2.0; 95% CI, 1.10–3.51; P = 0.04 and ARM vs. chromosomal anomalies: ORcrude, 3.3; 95% CI, 1.81–5.98; P = 0.02). Both results remain significant after adjustment for center and maternal age (ARM vs. non-chromosomal anomalies: ORadj, 2.0; 95% CI, 1.09–3.48 and ARM vs. chromosomal anomalies: ORadj, 2.8; 95% CI, 1.48–5.17). However, results became insignificant after adjustment for more than those two covariates. The study by Källén and Otterblad Olausson [42] observed a marginally increased risk for inhaled corticosteroids (ORadj, 1.9; 95% CI, 1.00–3.22).
Beta-2-agonists in general were not associated with ARM, whereas inhaled beta-2-agonists showed a significant association with ARM in the study by Garne et al. [73] (ARM vs. non-chromosomal anomalies: ORcrude, 1.7; 95% CI, 1.08–2.80; P = 0.03 and ARM vs. chromosomal anomalies: ORcrude, 2.3; 95% CI, 1.39–3.75; P = 0.003). After adjustment for covariates the association with the non-chromosomal anomaly control group became insignificant, the association with the chromosomal anomaly control group was weakened (ORadj, 1.8; 95% CI, 0.92–3.44). A suggestive association with ARM was observed for the use of budesonide in the study by Källén and Otterblad Olausson [42] (ORadj, 1.9; 95% CI, 0.95–3.42).
The result of the meta-analysis on the association between maternal use of any anti-asthma medication and ARM infants is shown in Fig. 4. From the study by Garne et al. [73] we used the OR calculated with the non-chromosomal anomaly control group and from the study by Zwink and Choinitzki et al. [53] the OR calculated with the group of control infants with esophageal atresia with or without tracheoesophageal fistula. The I2 statistic indicated homogeneity across the three studies (χ2 = 0.19; P = 0.91; I2 = 0%). In meta-analysis, a significant association was found for maternal use of any anti-asthma medication before or during pregnancy using a fixed effects model (OR, 1.64; 95% CI, 1.22–2.21; P = 0.001). There was no evidence of publication bias (Kendall’s tau = − 1.57, P = 0.12; Egger’s t value = − 1.96, P = 0.30).
Thyroid medication
Three studies reported on the association between maternal use of thyroid medication before or during pregnancy and infants born with an anorectal malformation (Table 4). The study by Browne et al. [61] reported on a significant association between anti-thyroid medication and ARM (ORcrude, 8.6; 95% CI, 1.7–40.2; P = 0.005) and the study by Källén et al. [75] on a marginally increased risk for thyroxin intake (RRcrude, 1.9; 95% CI, 1.00–1.85). In contrast, the study by Zwink and Choinitzki et al. [53] could not confirm the finding.
Psychiatric drugs
Nine studies reported on the association between maternal use of psychiatric drugs before or during pregnancy and infants born with an anorectal malformation (Table 5). The study by Wemakor et al. [50] reported a significant association for any selective serotonin reuptake inhibitors (SSRI) (ORadj, 2.5; 95% CI, 1.06–5.68). In addition, the study by Furu et al. [52] observed a suggestive association with any SSRI (ORcrude, 1.5; 95% CI, 0.95–2.37; P = 0.08). The result became insignificant after adjustment for covariates (ORadj, 1.4; 95% CI, 0.88–2.32). Neither the study by Alwan et al. [68] nor the study by Louik et al. [64] could confirm an association of any SSRI with ARM. Individual SSRI classes were assessed by Furu et al. [62] and Louik et al. [64]. Both studies reported on an increased risk for sertraline during and before pregnancy (Furu et al.: ORadj, 2.5; 95% CI, 1.09–5.57; Louik et al.: ORadj, 4.4; 95% CI, 1.2–16.4). Due to the small sample size, confidence intervals were very wide in both studies. However, there was no increased risk for citalopram.
Three studies assessed antidepressants in general [54, 56, 76]. None of them could find an association with ARM.
A marginally increased risk for diazepam was found in the study by Czeizel et al. [65] in both, in the entire pregnancy (ORadj, 1.9; 95% CI, 1.1–3.3) and in the second-third months of gestation (ORadj, 5.2; 95% CI, 1.4–19.7). The study by Bonnot et al. [43] showed a significant association between the use of lorazepam before or during pregnancy and ARM (ORadj, 6.2; 95% CI, 2.44–15.74). No association could be found in the study by Källén et al. [76] for other sedatives or hypnotics (RRcrude, 1.2; 95% CI, 0.33–3.06). A suggestive association with ARM was observed for the use of anticonvulsants in the study by Källén et al. [76] (RRcrude, 2.9; 95% CI, 0.96–6.86).
The result of the meta-analysis on the association between maternal use of antidepressants and ARM infants is shown in Fig. 5. The I2 statistic indicated homogeneity across the three studies (χ2 = 0.05; P = 0.97; I2 = 0%). No significant association was found for maternal use of antidepressants before or during pregnancy using a fixed effects model (OR, 1.16; 95% CI, 0.72–1.86; P = 0.54). There was no evidence of publication bias (Kendall’s tau = − 1.57, P = 0.12; Egger’s t value = − 2.73, P = 0.22).
The result of the meta-analysis on the association between maternal use of any SSRI and ARM infants is shown in Fig. 6. The I2 statistic indicated heterogeneity across studies (χ2 = 4.57; P = 0.2061; I2 = 34%). The estimated heterogeneity variance was tau2 = 0.0744. No significant association was observed in pooled analyses using the random effects model (OR, 1.48; 95% CI, 0.94–2.32; P = 0.093). There was no evidence of publication bias (Kendall’s tau = − 0.68, P = 0.50; Egger’s t value = 0.05, P = 0.97).
The result of the meta-analysis on the association between maternal use of citalopram and ARM infants is shown in Fig. 7. The I2 statistic indicated homogeneity across the three studies (χ2 = 0.39; P = 0.82; I2 = 0%). No significant association was found for maternal use of citalopram before or during pregnancy using a fixed effects model (OR, 1.68; 95% CI, 0.82–3.45; P = 0.15). There was no evidence of publication bias (Kendall’s tau = 1.57, P = 0.12; Egger’s t value = 4.48, P = 0.14).
The result of the meta-analysis on the association between maternal use of hypnotics and benzodiazepine and ARM infants is shown in Fig. 8. The I2 statistic indicated heterogeneity across studies (χ2 = 6.13; P = 0.047; I2 = 67.4%). The estimated heterogeneity variance was tau2 = 0.3820. In meta-analysis, a weak association was observed in pooled analyses using the random effects model (OR, 2.43; 95% CI, 1.03–5.73; P = 0.042). There was no evidence of publication bias (Kendall’s tau = − 0.52, P = 0.60; Egger’s t value = 0.22, P = 0.86).
Painkiller
Four studies reported on the association between maternal use of painkillers before or during pregnancy and infants born with an anorectal malformation (Table 6). Only the study by Czeizel et al. [71] found a suggestive association between acetylsalicylic acid and ARM (ORadj, 2.3; 95% CI, 0.9–5.6) when using a population control group, including maternal self-reported and medical documented drug use.
Anti-infectives
Among the four studies that reported on the association between maternal use of anti-infectives before or during pregnancy and infants born with an anorectal malformation (Table 7), none could find an association with ARM.
Drugs against nausea and vomiting
Two studies reported on the association between maternal use of drugs against nausea and vomiting before or during pregnancy and infants born with an anorectal malformation (Table 8). The study by Källén and Mottet [78] found a marginally increased risk for meclozine intake (RR, 2.3; 95% CI, 0.99–4.50). There was no association with metoclopramide and ARM (PORadj, 0.8; 95% CI, 0.36–1.66) [49].
Sexual hormones
Among the two studies that reported on the association between maternal use of sexual hormones before or during pregnancy and infants born with an anorectal malformation (Table 9), neither the study by Reefhuis et al. [55] not the study by Stoll et al. [72] could find an association for clomiphene citrate (ORadj, 1.2; 95% CI, 0.6–2.3) or estrogens (OR, 0.1; 95% CI, 0.03–0.63).
Other medical drugs
Among the two studies that reported on the association between maternal use of other medical drugs, among them antispasmodics, other miscellaneous medication and mixed preparations, before or during pregnancy and infants born with an anorectal malformation (Table 10), none could find an association with ARM.
Discussion
This systematic review and meta-analysis summarized the results of 37 epidemiological studies on the association between maternal medical drug intake and infants born with an anorectal malformation reported between 1977 and April 2017. The majority of the studies were conducted in the United States. Case numbers ranged from six ARM cases in the study by Bonnot et al. [43] to 799 ARM cases in the study by Furu et al. [52]. Studies were also heterogeneous with respect to period ingestion of medical drug use, control selection and adjustment for covariates. Less than half of the studies classified the administrated medical drug either by the international ATC classification or linked medication to the Slone Drug Dictionary [50, 52, 54, 56,57,58,59, 61,62,63, 67, 68, 73, 75, 76, 78]. Meta-analysis was done for medical drugs reported on in at least three studies, i.e. maternal use of folic acid, multivitamins, any anti-asthma medication, any selective serotonin reuptake inhibitors (SSRI), antidepressants, citalopram,, and hypnotics and benzodiazepine.
There is a great discrepancy in the reported results on the association between the different maternal medical drugs and ARM which impede comparability. As the exact active agent, dose and frequency of medical drug use is not reported in all studies, one can only speculate about possible detrimental effects on embryogenesis due to high dose/overdose of medical drugs. Such effects have been already observed in previous studies with vitamin A and etretinate for other birth defects [39, 83]. On the other hand, a vitamin A deficiency during pregnancy may also lead to birth defects like ARM [40]. To our knowledge, no previous epidemiological study exists assessing the association between vitamin A and ARM. However, six studies assessed multivitamins in general, resulting in no association with ARM in meta-analysis.
In contrast, the use of folic acid before and during pregnancy is discussed as having a protective effect for birth defects, among them neutral tube defects, cleft lip and cleft palate and heart defects [84,85,86]. The German Society for Nutrition (DGE) [87] recommends a daily folic acid intake of 400 micrograms per day at least 4 weeks before conception and later 450–550 micrograms per day for all pregnant women. Unwanted side effects with the intake of folic acid are not known. Our meta-analysis, however, could not show any association with ARM. In contrast, the study by Faria et al. [88] observed in their experimental model a reducing effect in the incidence of ARM when inducing ethylenethiourea in rats.
Depressions are common in pregnancy. Previous studies have been shown that approximately 10–15% of all women suffer from peripartum depression [89]. It is suggested that depression during pregnancy might be a risk factor for preterm birth and small-for-gestational-age, and possibly also for low birthweight [90, 91]. Depending on the strength of the symptoms, depression can be either treated with psychotherapy, medical drug intake or in case of severe depression with clinical stay. Antidepressant use in first trimester pregnancy has been estimated at 1–8% [92,93,94]. The most frequently used antidepressants are selective serotonin reuptake inhibitors (SSRIs). Up to 2005, SSRIs were regarded to be safe in pregnancy. Thereafter, its safety was questioned as different studies reported on an association between congenital malformations and SSRI use in first trimester of pregnancy [52, 56, 95,96,97]. A consistently risk, however, could only be observed for congenital heart defects, including septal heart defects [98]. There are assumptions that the risk further strongly increases when using several SSRI before and during pregnancy [97]. With respect to interactions with other drugs, citalopram, escitalopram and sertraline are assumed to be better than other SSRIs [99]. In Germany, citalopram is the most common prescribe medical drug, followed by sertraline and escitalopram [100]. In this meta-analysis, no association was found for antidepressants or any SSRIs with ARM. Hypnotics and benzodiazepine, including diazepam, larozepam and sedatives or hypnotics, showed a more than doubled risk for ARM.
The prevalence of asthma in pregnancy is estimated to be 4–12% [101, 102]. Mothers with this chronic disease are recommended to continue their medication during pregnancy. Its medical treatment includes the use of beta-2-agonists for symptom relief (rescue treatment) and/or anti-inflammatory medications for reducing and preventing chronic inflammation in the airways. In literature, an increased risk with specific birth defects, among them malformations of the nervous system, respiratory system, and digestive system, esophageal atresia, omphalocele, cardiac defects, facial clefts and gastroschisis, could be observed [59, 73, 103]. However, it remains unclear whether the medication increases the risk for congenital malformations or the disease itself. In this meta-analysis, we could also confirm an increased risk for ARM. The risk was almost doubled in mothers who used any anti-asthma medication before and during pregnancy.
Disorders of thyroid function are divided into hypothyroidism with an extremely low level of metabolism hormone thyroxine, and hyperthyroidism with an excessive production of thyroid hormones. In general, changes in thyroid function are available in up to 15% of all pregnancies, with a prevalence of overt and subclinical hypothyroidism of approximately 0.4% and 2–3%, respectively, and of overt and subclinical hyperthyroidism of approximately 0.1–0.4% and 2%, respectively [104, 105]. An untreated hypo- or hyperthyroidism seems to increase the risk for early or stillbirths and underweight babies [106]. With a physician well-controlled medication intake, however, no adverse effects on the unborn child could be verified. Furthermore, only few studies reported on an association between thyroid medication and congenital malformations, with almost inconsistent results [79, 107,108,109,110]. The findings suggest an association for heart defects, central nervous system defects, intestinal defects, hypospadias, and limb deficiencies. For ARM, available results were contradictory and did not allow any conclusion.
When available, data on ARM infants with isolated anomalies (no additional major defects) were preferred in this review to data on ARM infants with multiple defects. Only three of the 37 reviewed studies looked at both groups [41, 59, 73]. Analyses, however, showed nearly the same results. Further six studies reported on isolated ARM cases only [53, 57, 65, 69,70,71]. The three studies by Wikner et al. [111], Yuskiv et al. [112] and Mastroiacovo et al. [113] were excluded because they analyzed ARM in a group with other major congenital malformations that could be not clearly differentiated and individually assigned to medical exposure, and which might thereby mix or dilute potential effects in case of diverse etiologies. The excluded studies did not find an association with the examined risk factors (multivitamin and vitamin A, respectively).
Looking at some other gastrointestinal malformations, asthma medication use during pregnancy also seem to increase the risk for esophageal atresia, omphalocele and gastroschisis [59, 73]. There is a suggestive association between any antibiotics and small intestinal atresia/stenosis as well as between any antibiotics and gastroschisis [63]. In addition, the use of SSRIs in pregnancy is also reported to be a risk for omphalocele and gastroschisis [50, 52, 54, 64, 68]. The use of vasoactive medication, including pseudoephedrine, acetaminophen, phenylpropanolamine, aspirin, ibuprofen, and acetaminophen, was reported to be an elevated risk for gastroschisis and small intestinal atresia [67, 114,115,116,117,118]. Furthermore, the use of anticonvulsants as well as a daily intake of vitamin E of more than 7.8 mg might increase the risk for small intestinal atresia/stenosis [57, 76].
The significant associations with ARM and some other gastro-intestinal malformations show clearly the need of a physician well-controlled medication intake during pregnancy to early detect a possible overdose or incorrect intake or even interactions due to multiple medication intake.
Our review has a number of limitations mostly resulting from the overall scarcity of published evidence. First, our meta-analysis was limited by the data provided in the individual studies. Not all studies provided risk estimates adjusted for potentially influential confounders, such as maternal age, periconceptional smoking, pregnancy BMI, race/ethnicity, education and parity. A homogenous epidemiological study is almost impossible to get. It is essential to adjust for potentially confounders, including interaction between various drugs. Doing not so makes a direct comparison of the results difficult and thus the interpretation in meta-analyses. Furthermore, so called “ad hoc” studies would be desirable. However, in studies assessing rare diseases, high efforts and costs are needed to achieve a suitable sample size. Due to the small number of studies, we decided to pool adjusted and crude values for meta-analyses. Second, the used medical drug was almost not exactly described in the studies, including medication classification with its active agents, dose and frequency of medical drug use, and the intake of multiple medications simultaneously and thereby possible occurring interactions. Third, studies did not differentiate between ARM phenotypes ranking from lower to higher forms with different genetic background [18]. Fourth, some studies used affected (malformed) control groups. Other studies used mixed controls of live-born malformed and healthy babies. A potential advantage of using malformed controls is potential reduction of response bias or recall bias that may occur when a non-malformed control group is used. On the other hand, observed associations may be biased if the risk factors of interest are also associated with the malformations of controls. Fifth, most sample sizes were small, so the power to detect associations was low. Sixth, despite the lack of indication of major publication bias, it is impossible to be ruled out completely, especially in the light of the low number of studies. Seventh, although we searched in three databases (PubMed, ISI Web of Knowledge and Scopus) and completed our search by reviewing related and cross-referencing literature, existence of relevant missing or up to now unpublished studies cannot be excluded. In addition, we had no contact to authors to help ensure all relevant studies were included. However, as part of the international network on anorectal malformations (ARM-Net), we were in regular contact with its experts. Finally, the restriction to English-language articles might also have an influence to the limited evidence for ARM. Nevertheless, non-English-language articles are also not all available on databases such as PubMed, ISI Web of Knowledge and Scopus.
Conclusions
To our knowledge, our article is the first systematic review and meta-analysis that provides an overview of the available epidemiological studies that reported on the association between maternal medical drug use before and during pregnancy and ARM. Adequate evidence is still very limited, especially in regard to gene interaction. Separate report of isolated ARM and those cases with multiple defects should become standard. Due to small sample sizes, it is understandable that data are very often analyzed together. Approximately 64% of all ARM patients have one or more additional extra-anal anomalies and only 36% have an isolated ARM (no further major birth defect) [5]. Nevertheless, results may be biased if the potential risk factor of interest is associated with an additional extra-anal anomaly, such as kidney, renal or heart defect. To facilitate drug comparison and obtain meaningful results, international classifications such as the World Health Organization’s Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD) [80, 81], are required to specify exactly medical drugs as well as to prescribe its dose and frequency. In addition, the intake of multiple medications simultaneously and thereby possible occurring interactions must be considered. Furthermore, it may be an inherent bias source to distinguish between parental chronic disease and their drug treatment. For example, in a previous study [28], we found maternal respiratory disease as a periconceptional risk factor, but it remains unclear whether the disease or the medication (agents or additives) treatment represents the risk factor. The same was observed in the study by Acs et al. [119] with maternal dyspepsia. Thus, further symptoms have been to be investigated. Further multicenter or register-based studies are needed to clarify the role of maternal medical drug intake for the development of ARM.
Abbreviations
- ARM:
-
Anorectal malformations
- ATC/DDD:
-
The World Health Organization’s Anatomical Therapeutic Chemical classification system with Defined Daily Doses
- CI:
-
Confidence interval
- DGE:
-
The German Society for Nutrition
- OR:
-
Odds ratio
- RR:
-
Risk ratio
- SSRI:
-
Selective serotonin reuptake inhibitors
- USA:
-
United States of America
References
Forrester MB, Merz RD. Risk of selected birth defects with prenatal illicit drug use, Hawaii, 1986-2002. J Toxicol Environ Health A. 2007;70:7–18.
International Clearinghouse for Birth Defects Surveillance and Research (ICBDSR). Annual report 2014. http://www.icbdsr.org. Accessed 21 Sept 2017.
Jenetzky E. Prevalence estimation of anorectal malformations using German diagnosis related groups system. Pediatr Surg Int. 2007;23:1161–5.
Cho S, Moore S, Fangman T. One hundred three consecutive patients with anorectal malformations and their associated anomalies. Arch Pediatr Adolesc Med. 2001;155:587–91.
Cuschieri A, EUROCAT Working Group. Descriptive epidemiology of isolated anal anomalies: a survey of 4.6 million births in Europe. Am J Med Genet. 2001;103:207–15.
Correa A, Botto L, Liu Y, Mulinare J, Erickson JD. Do multivitamin supplements attenuate the risk for diabetes-associated birth defects? Pediatrics. 2003;111:1146–51.
Leck I, Lancashire R. Birth prevalence of malformations in members of different ethnic groups and in the offspring of matings between them, in Birmingham, England. J Epidemiol Community Health. 1995;49:171–9.
Louw J. Congenital abnormalities of the rectum and anus. Curr Probl Surg. 1965;2:1–64.
Moore S, Alexander A, Sidler D, Alves J, Hadley GP, Numanoglu A, et al. The spectrum of anorectal malformations in Africa. Pediatr Surg Int. 2008;24:677–83.
Murphy F, Puri P, Hutson JM, Holschneider AM. Incidence and frequency of different types and classification of Anorectal malformations. In: Holschneider AM, Hutson JM, editors. Anorectal Malformations in Children: Embryology, Diagnosis, Surgical Treatment, Follow-up. Berlin: Springer; 2006. p. 163–84.
Stephens FD, Smith ED, Paul NW. Anorectal malformations in children: update 1988. Birth Defects Orig Artic Ser. 1988;24:1–604.
Fitzgerald JT, Fitzgerald M. Human Embryology: A Human Approach. Philadelphia: Bailliere Tindall; 1994.
Froster U, Wallner S, Reusche E, Schwinger E, Rehder H. VACTERL with hydrocephalus and branchial arch defects: prenatal, clinical, and autopsy findings in two brothers. Am J Med Genet. 1996;62:169–72.
Hutson M, v Putte SCJ, Penington E, Kluth D, Fiegel H. The Embryology of Anorectal Malformations. In: Holschneider AM, Hutson JM, editors. Anorectal Malformations in Children: Embryology, Diagnosis, Surgical Treatment, Follow-up. Berlin: Springer; 2006. p. 49–63.
Kluth D, Hillen M, Lambrecht W. The principles of normal and abnormal hindgut development. J Pediatr Surg. 1995;30:1143–7.
Martínez-Frías M, Frías J, Opitz J. Errors of morphogenesis and developmental field theory. Am J Med Genet. 1998;76:291–6.
Nievelstein R, van der Werff J, Verbeek F, Valk J, Vermeij-Keers C. Normal and abnormal embryonic development of the anorectum in human embryos. Teratology. 1998;57:70–8.
Falcone RJ, Levitt M, Peña A, Bates M. Increased heritability of certain types of anorectal malformations. J Pediatr Surg. 2007;42:124–7.
Schramm C, Draaken M, Tewes G, Bartels E, Schmiedeke E, Märzheuser S, et al. Autosomal-dominant non-syndromic anal atresia: sequencing of candidate genes, array-based molecular karyotyping, and review of the literature. Eur J Pediatr. 2011;170:741–6.
Bartels E, Draaken M, Kazmierczak B, Spranger S, Schramm C, Baudisch F, et al. De novo Partial Trisomy 18p and Partial Monosomy 18q in a Patient with Anorectal Malformation. Cytogenet Genome Res. 2011;134:243–8.
Schramm C, Draaken M, Bartels E, Boemers TM, Schmiedeke E, Grasshoff-Derr S, et al. De novo duplication of 18p11.21-18q12.1 in a female with anorectal malformation. Am J Med Genet A. 2011;155A:445–9.
Draaken M, Prins W, Zeidler C, Hilger A, Mughal SS, Latus J, et al. Involvement of the WNT and FGF signaling pathways in non-isolated anorectal malformations: sequencing analysis of WNT3A, WNT5A, WNT11, DACT1, FGF10, FGFR2 and the T gene. Int J Mol Med. 2012;30:1459–64.
Dworschak GC, Draaken M, Marcelis C, de Blaauw I, Pfundt R, van Rooij IA, et al. De novo 13q deletions in two patients with mild anorectal malformations as part of VATER/VACTERL and VATER/VACTERL-like association and analysis of EFNB2 in patients with anorectal malformations. Am J Med Genet A. 2013;161A:3035–41.
van de Putte R, Wijers CH, de Blaauw I, Marcelis CL, Sloots CE, Brooks AS, et al. Previous miscarriages and GLI2 are associated with anorectal malformations in offspring. Hum Reprod. 2017;32:299–306.
Zhu Z, Peng L, Chen G, Jiang W, Shen Z, Du C, et al. Mutations of MYH14 are associated to anorectal malformations with recto-perineal fistulas in a small subset of Chinese population. Clin Genet. 2017;92:503-9.
Zwink N, Jenetzky E, Brenner H. Parental risk factors and anorectal malformations: systematic review and meta-analysis. Orphanet J Rare Dis. 2011;6:25.
van Rooij I, Wijers C, Rieu P, Hendriks HS, Brouwers MM, Knoers NV, et al. Maternal and paternal risk factors for anorectal malformations: a Dutch case-control study. Birth Defects Res A Clin Mol Teratol. 2010;88:152–8.
Zwink N, Rissmann A, Pötzsch S, Reutter H, Jenetzky E, CURE-Net Consortium. Parental risk factors of anorectal malformations: Analysis with a regional population-based control group. Birth Defects Res A Clin Mol Teratol. 2016;106:133–41.
Wijers C, de Blaauw I, Marcelis C, Wijnen RM, Brunner H, Midrio P, et al. Research perspectives in the etiology of congenital anorectal malformations using data of the International Consortium on Anorectal Malformations: evidence for risk factors across different populations. Pediatr Surg Int. 2010;26:1093–9.
Tinker S, Reefhuis J, Dellinger A, Jamieson DJ. Maternal injuries during the periconceptional period and the risk of birth defects, National Birth Defects Prevention Study, 1997-2005. Paediatr Perinat Epidemiol. 2011;25:487–96.
Lilja M. Infants with single umbilical artery studied in a national registry. General epidemiological characteristics. Paediatr Perinat Epidemiol. 1991;5:27–36.
Zwink N, Jenetzky E, Schmiedeke E, Schmidt D, Märzheuser S, Grasshoff-Derr S, et al. Assisted reproductive techniques and the risk of anorectal malformations: a German case-control study. Orphanet J Rare Dis. 2012;7:65.
Reefhuis J, Honein MA, Schieve LA, Correa A, Hobbs CA, Rasmussen SA, et al. Assisted reproductive technology and major structural birth defects in the United States. Hum Reprod. 2009;24:360–6.
Ericson A, Källén B. Congenital malformations in infants born after IVF: a population-based study. Hum Reprod. 2001;16:504–9.
Källén B, Finnström O, Lindam A, Nilsson E, Nygren KG, Otterblad PO. Congenital malformations in infants born after in vitro fertilization in Sweden. Birth Defects Res A Clin Mol Teratol. 2010;88:137–43.
Källén B, Finnström O, Nygren K, Olausson PO. In vitro fertilization (IVF) in Sweden: risk for congenital malformations after different IVF methods. Birth Defects Res A Clin Mol Teratol. 2005;73:162–9.
Midrio P, Nogare C, Di Gianantonio E, Clementi M. Are congenital anorectal malformations more frequent in newborns conceived with assisted reproductive techniques? Reprod Toxicol. 2006;22:576–7.
Wijers C, van Rooij I, Rassouli R, Wijnen MH, Broens PM, Sloots CE, et al. Parental subfertility, fertility treatment, and the risk of congenital anorectal malformations. Epidemiology. 2015;26:169–76.
Rothman K, Moore L, Singer M, Nguyen US, Mannino S, Milunsky A. Teratogenicity of high vitamin A intake. N Engl J Med. 1995;333:1369–73.
Huang Y, Zheng S. The effect of vitamin A deficiency during pregnancy on anorectal malformations. J Pediatr Surg. 2011;46:1400–5.
Wijers C, de Blaauw I, Zwink N, Draaken M, van der Zanden LF, Brunner HG, et al. No major role for periconceptional folic acid use and its interaction with the MTHFR C677T polymorphism in the etiology of congenital anorectal malformations. Birth Defects Res A Clin Mol Teratol. 2014;100:483–92.
Källén B, Otterblad OP. Use of anti-asthmatic drugs during pregnancy. 3. Congenital malformations in the infants. Eur J Clin Pharmacol. 2007;63:383–8.
Bonnot O, Vollset S, Godet P, D'Amato T, Robert E. Maternal exposure to lorazepam and anal atresia in newborns: results from a hypothesis-generating study of benzodiazepines and malformations. J Clin Psychopharmacol. 2001;21:456–8.
Higgens J, Simon G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Higgins J, Thompson S, Deeks J, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Ioannidis J, Patsopoulos N, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335:914–6.
Begg C, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Pasternak B, Svanström H, Mølgaard-Nielsen D, Melbye M, Hviid A. Metoclopramide in pregnancy and risk of major congenital malformations and fetal death. JAMA. 2013;310:1601–11.
Wemakor A, Casson K, Garne E, Bakker M, Addor MC, Arriola L, et al. Selective serotonin reuptake inhibitor antidepressant use in first trimester pregnancy and risk of specific congenital anomalies: a European register-based study. Eur J Epidemiol. 2015;30:1187–98.
Myers M, Li S, Correa-Villaseñor A, Li Z, Moore CA, Hong SX, et al. Folic acid supplementation and risk for imperforate anus in China. Am J Epidemiol. 2001;154:1051–6.
Furu K, Kieler H, Haglund B, Engeland A, Selmer R, Stephansson O, et al. Selective serotonin reuptake inhibitors and venlafaxine in early pregnancy and risk of birth defects: population based cohort study and sibling design. BMJ. 2015;350:h1798.
Zwink N, Choinitzki V, Baudisch F, Hölscher A, Boemers TM, Turial S, et al. Comparison of environmental risk factors for esophageal atresia, anorectal malformations, and the combined phenotype in 263 German families. Dis Esophagus. 2016;29:1032–42.
Polen K, Rasmussen S, Riehle-Colarusso T, Reefhuis J, National Birth Defects Prevention Study. Association between reported venlafaxine use in early pregnancy and birth defects, national birth defects prevention study, 1997-2007. Birth Defects Res A Clin Mol Teratol. 2013;97:28–35.
Reefhuis J, Honein M, Schieve L, Rasmussen SA, National Birth Defects Prevention Study. Use of clomiphene citrate and birth defects, National Birth Defects Prevention Study, 1997-2005. Hum Reprod. 2011;26:451–7.
Reis M, Källén B. Delivery outcome after maternal use of antidepressant drugs in pregnancy: an update using Swedish data. Psychol Med. 2010;40:1723–33.
Gilboa S, Lee K, Cogswell M, Traven FK, Botto LD, Riehle-Colarusso T, et al. Maternal intake of vitamin E and birth defects, national birth defects prevention study, 1997 to 2005. Birth Defects Res A Clin Mol Teratol. 2014;100:647–57.
Hernandez R, Werler M, Romitti P, Sun L, Anderka M, National Birth Defects Prevention Study. Nonsteroidal antiinflammatory drug use among women and the risk of birth defects. Am J Obstet Gynecol. 2012;206:228.e1-8.
Lin S, Munsie J, Herdt-Losavio M, Druschel CM, Campbell K, Browne ML, et al. Maternal asthma medication use and the risk of selected birth defects. Pediatrics. 2012;129:e317–24.
van Gelder M, Roeleveld N, Nordeng H. Exposure to non-steroidal anti-inflammatory drugs during pregnancy and the risk of selected birth defects: a prospective cohort study. PLoS One. 2011;6:e22174.
Browne M, Rasmussen S, Hoyt A, Waller DK, Druschel CM, Caton AR, et al. Maternal thyroid disease, thyroid medication use, and selected birth defects in the National Birth Defects Prevention Study. Birth Defects Res A Clin Mol Teratol. 2009;85:621–8.
Carter T, Druschel C, Romitti P, Bell EM, Werler MM, Mitchell AA, et al. Antifungal drugs and the risk of selected birth defects. Am J Obstet Gynecol. 2008;198:191.e1-7.
Crider K, Cleves M, Reefhuis J, Berry RJ, Hobbs CA, Hu DJ. Antibacterial medication use during pregnancy and risk of birth defects: National Birth Defects Prevention Study. Arch Pediatr Adolesc Med. 2009;163:978–85.
Louik C, Lin A, Werler M, Hernández-Díaz S, Mitchell AA. First-trimester use of selective serotonin-reuptake inhibitors and the risk of birth defects. N Engl J Med. 2007;356:2675–83.
Czeizel A, Erös E, Rockenbauer M, Sørensen HT, Olsen J. Short-Term Oral Diazepam Treatment during Pregnancy: A Population-Based Teratological Case-Control Study. Clin Drug Investig. 2003;23:451–62.
Czeizel A. The primary prevention of birth defects: Multivitamins or folic acid? Int J Med Sci. 2004;1:50–61.
Yau W, Mitchell A, Lin K, Werler MM, Hernández-Díaz S. Use of decongestants during pregnancy and the risk of birth defects. Am J Epidemiol. 2013;178:198–208.
Alwan S, Reefhuis J, Rasmussen S, Olney RS. Friedman JM; National Birth Defects Prevention Study. Use of selective serotonin-reuptake inhibitors in pregnancy and the risk of birth defects. N Engl J Med. 2007;356:2684–92.
Czeizel A, Dobó M, Vargha P. Hungarian cohort-controlled trial of periconceptional multivitamin supplementation shows a reduction in certain congenital abnormalities. Birth Defects Res A Clin Mol Teratol. 2004;70:853–61.
Czeizel A, Rockenbauer M, Sørensen H, Olsen J. Use of cephalosporins during pregnancy and in the presence of congenital abnormalities: a population-based, case-control study. Am J Obstet Gynecol. 2001;184:1289–96.
Czeizel A, Rockenbauer M, Mosonyi A. A population-based case-control teratologic study of acetylsalicylic acid treatments during pregnancy. Pharmacoepidemiol Drug Saf. 2000;9:193–205.
Stoll C, Alembik Y, Roth M, Dott B. Risk factors in congenital anal atresias. Ann Genet. 1997;40:197–204.
Garne E, Hansen A, Morris J, Zaupper L, Addor MC, Barisic I, et al. Use of asthma medication during pregnancy and risk of specific congenital anomalies: A European case-malformed control study. J Allergy Clin Immunol. 2015;136:1496–502.
Angerpointner T, Radtke W, Murken J. Catamnestic investigations in children with malformations of the gastrointestinal tract and the abdominal wall. Z Kinderchir. 1981;32:129–44.
Källén B, Norstedt WB. Maternal hypothyroidism in early pregnancy and infant structural congenital malformations. J Thyroid Res. 2014; https://doi.org/10.1155/2014/160780.
Källén B, Borg N, Reis M. The use of central nervous system active drugs during pregnancy. Pharmaceuticals (Basel). 2013;6:1221–86.
Källén B. Congenital malformations in infants whose mothers reported the use of folic acid in early pregnancy in Sweden. A prospective population study. Congenit Anom (Kyoto). 2007;47:119–24.
Källén B, Mottet I. Delivery outcome after the use of meclozine in early pregnancy. Eur J Epidemiol. 2003;18:665–9.
Heinonen OP, Slone D, Shapiro S. Birth Defects and Drugs in Pregnancy. Littleton: Publishing Sciences Group, Inc; 1977.
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2013. 16th ed. Oslo: Norwegian Institute of Public Health; 2012. https://www.whocc.no/filearchive/publications/1_2013guidelines.pdf. Accessed 21 Sept 2017
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2017. http://www.whocc.no/atc_ddd_index. Accessed 21 Sept 2017.
Slone Epidemiology Center at Boston University. The Slone Drug Dictionary. 2017. https://www.bu.edu/slone/drug-dictionary. Accessed 21 Sept 2017.
Bitoh Y, Shimotake T, Kubota Y, Kimura O, Iwai N. Impaired distribution of retinoic acid receptors in the hindgut-tailgut region of murine embryos with anorectal malformations. J Pediatr Surg. 2001;36:377–80.
De-Regil L, Peña-Rosas J, Fernández-Gaxiola A, Rayco-Solon P. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst Rev. 2015; https://doi.org/10.1002/14651858.
van Beynum I, Kapusta L, Bakker M, den Heijer M, Blom HJ, de Walle HE. Protective effect of periconceptional folic acid supplements on the risk of congenital heart defects: a registry-based case-control study in the northern Netherlands. Eur Heart J. 2010;31:464–71.
Rozendaal A, van Essen A, te Meerman G, Bakker MK, van der Biezen JJ, Goorhuis-Brouwer SM, et al. Periconceptional folic acid associated with an increased risk of oral clefts relative to non-folate related malformations in the Northern Netherlands: a population based case-control study. Eur J Epidemiol. 2013;28:875–87.
The German Society for Nutrition (DGE). [Folsäure in der Prävention]. 2008. https://www.dge.de. Accessed 21 Sept 2017.
Faria D, Simões Mde J, Martins J. Is it possible folic acid reduce anorectal malformations ethylenethiourea induced in rats? Acta Cir Bras. 2015;30:517–22.
O'Keane V, Marsh M. Depression during pregnancy. BMJ. 2007;334:1003–5.
Szegda K, Markenson G, Bertone-Johnson E, Chasan-Taber L. Depression during pregnancy: a risk factor for adverse neonatal outcomes? A critical review of the literature. J Matern Fetal Neonatal Med. 2014;27:960–7.
Lefkovics E, Baji I, Rigó J. Impact of maternal depression on pregnancies and on early attachment. Infant Ment Health J. 2014;35:354–65.
Nordeng H, van Gelder M, Spigset O, Koren G, Einarson A, Eberhard-Gran M. Pregnancy outcome after exposure to antidepressants and the role of maternal depression: results from the Norwegian Mother and Child Cohort Study. J Clin Psychopharmacol. 2012;32:186–94.
Charlton R, Jordan S, Pierini A, Garne E, Neville AJ, Hansen AV, et al. Selective serotonin reuptake inhibitor prescribing before, during and after pregnancy: a population-based study in six European regions. BJOG. 2015;122:1010–20.
Cooper W, Willy M, Pont S, Ray WA. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196:544.e1-5.
Vasilakis-Scaramozza C, Aschengrau A, Cabral HJ, Jick SS. Antihypertensive drugs and the risk of congenital anomalies. Pharmacotherapy. 2013;33:476–82.
Oberlander T, Warburton W, Misri S, Riggs W, Aghajanian J, Hertzman C. Major congenital malformations following prenatal exposure to serotonin reuptake inhibitors and benzodiazepines using population-based health data. Birth Defects Res B Dev Reprod Toxicol. 2008;83:68–76.
Pedersen L, Henriksen T, Vestergaard M, Olsen J, Bech BH. Selective serotonin reuptake inhibitors in pregnancy and congenital malformations: population based cohort study. BMJ. 2009;339:b3569.
Gentile S. Early pregnancy exposure to selective serotonin reuptake inhibitors, risks of major structural malformations, and hypothesized teratogenic mechanisms. Expert Opin Drug Metab Toxicol. 2015;11:1585–97.
Benkert O, Hippius H. Kompendium der Psychiatrischen Pharmakotherapie. 9th ed. Berlin: Springer; 2013.
Schwabe U, Paffrath D. Arzneiverordnungs-Report 2012. 1st ed. Berlin: Springer; 2012.
Kwon H, Belanger K, Bracken M. Asthma prevalence among pregnant and childbearing-aged women in the United States: estimates from national health surveys. Ann Epidemiol. 2003;13:317–24.
Charlton R, Pierini A, Klungsøyr K, Neville AJ, Jordan S, de Jong-van den Berg LT, et al. Asthma medication prescribing before, during and after pregnancy: a study in seven European regions. BMJ. 2016;6:e009237.
Blais L, Kettani F, Elftouh N, Forget A. Effect of maternal asthma on the risk of specific congenital malformations: A population-based cohort study. Birth Defects Res A Clin Mol Teratol. 2010;88:216–22.
Tirosh D, Benshalom-Tirosh N, Novack L, Press F, Beer-Weisel R, Wiznitzer A, et al. Hypothyroidism and diabetes mellitus - a risky dual gestational endocrinopathy. PeerJ. 2013;1:e52.
Ahmad S, Geraci S, Koch C. Thyroid disease in pregnancy: (Women's Health Series). South Med J. 2013;106:532–8.
Negro R, Mestman J. Thyroid disease in pregnancy. Best Pract Res Clin Endocrinol Metab. 2011;25:927–43.
Wikner B, Sparre L, Stiller C, Källén B, Asker C. Maternal use of thyroid hormones in pregnancy and neonatal outcome. Acta Obstet Gynecol Scand. 2008;87:617–27.
Khoury M, Becerra J, d'Almada P. Maternal thyroid disease and risk of birth defects in offspring: a population-based case-control study. Paediatr Perinat Epidemiol. 1989;3:402–20.
Queisser-Luft A, Eggers I, Stolz G, Kieninger-Baum D, Schlaefer K. Serial examination of 20,248 newborn fetuses and infants: correlations between drug exposure and major malformations. Am J Med Genet. 1996;63:268–76.
Lee L, Canfield M, Hashmi S, Moffitt KB, Marengo L, Agopian AJ, et al. Association between thyroxine levels at birth and choanal atresia or stenosis among infants in Texas, 2004-2007. Birth Defects Res A Clin Mol Teratol. 2012;94:951–4.
Wikner BN, Stiller C-O, Bergman U, Asker C, Källén B. Use of benzodiazepines and benzodiazepine receptor agonists during pregnancy: neonatal outcome and congenital malformations. Pharmacoepidemiol Drug Saf. 2007;16:1203–10.
Yuskiv N, Honein M, Moore C. Reported multivitamin consumption and the occurrence of multiple congenital anomalies. Am J Med Genet A. 2005;136:1–7.
Mastroiacovo P, Mazzone T, Addis A, Elephant E, Carlier P, Vial T, et al. High vitamin A intake in early pregnancy and major malformations: a multicenter prospective controlled study. Teratology. 1999;59:7–11.
Werler M, Sheehan J, Mitchell A. Maternal medication use and risks of gastroschisis and small intestinal atresia. Am J Epidemiol. 2002;155:26–31.
Martínez-Frías M, Rodríguez-Pinilla E, Prieto L. Prenatal exposure to salicylates and gastroschisis: a case-control study. Teratology. 1997;56:241–3.
Torfs C, Katz E, Bateson T, Lam PK, Curry CJ. Maternal medications and environmental exposures as risk factors for gastroschisis. Teratology. 1996;54:84–92.
Werler M, Mitchell A, Shapiro S. First trimester maternal medication use in relation to gastroschisis. Teratology. 1992;45:361–7.
Drongowski R, Smith RJ, Coran A, Klein MD. Contribution of demographic and environmental factors to the etiology of gastroschisis: a hypothesis. Fetal Diagn Ther. 1991;6:14–27.
Acs N, Bánhidy F, Puhó EH, Czeizel AE. A possible association between maternal dyspepsia and congenital rectal/anal atresia/stenosis in their children: a population-based case-control study. Acta Obstet Gynecol Scand. 2009;88:1017–23.
Acknowledgements
Not applicable.
Funding
NZ and EJ are members of the “Network for the Systematic Investigation of the Molecular Causes, Clinical Implications, and Psychosocial Outcome of Congenital Uro-Rectal Malformations (CURE-Net)”, which was supported by a research grant from the German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung, BMBF), funding code 01GM08107 (2009–2012). Statistical calculations were supported by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG) under the funding code JE681/3–1 (2013–2016).
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
Conception and design was done by NZ and EJ. Literature review, data extraction and statistical analysis were carried out by NZ and EJ. Drafting of the article was done by NZ. Revision of the article was done by NZ and EJ. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zwink, N., Jenetzky, E. Maternal drug use and the risk of anorectal malformations: systematic review and meta-analysis. Orphanet J Rare Dis 13, 75 (2018). https://doi.org/10.1186/s13023-018-0789-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-018-0789-3