Abstract
Objective
To investigate how the ulcerative colitis (UC) be treated with Chinese herbal medicines (CHM), using Chinese medicine (CM) pattern (zheng) identification, in the current clinical practice.
Methods
A total of 7 electronic databases were systematically searched for UC clinical studies with CHM interventions (including single herbs and CHM formulas) published in English and Chinese from the date of their inception to November 25, 2020. Descriptive statistics were adopted to demonstrate the characteristics of study design, and to collate the commonly CM patterns of UC and frequently used CHM herbs and formulas. Further, IBM SPSS Modeler 18.0 and Cytoscape 3.7.1 software were used to analyze and visualize the associations between different categories of CHM and their zheng indications.
Results
A total of 2311 articles were included in this study, of which most (> 90%) were RCTs with CHM formulas. The most common zheng of UC was Large intestine dampness-heat, while the basic type of CM patten was Spleen deficiency. The most frequently used classical formula was Bai-Tou-Weng-Tang, followed by Shen-Ling-Bai-Zhu-San, and the commonly used proprietary CHM was Xi-Lei-San (enema). Sulfasalazine and Mesalazine are commonly used as concomitant western medicines. The most frequently used single medicinals were Huang Lian and Bai Zhu, which also identified as the core herbs for different CM patterns.
Conclusion
This study examined the application of CHM interventions for UC and summarized their characteristics in clinical practice. These data indicated there were limited information about the safety assessment of CHM formulas and further RCTs including CM pattern(s) with strict design are necessary.
Similar content being viewed by others
Background
Ulcerative Colitis (UC), which is one type of inflammatory bowel disease (IBD, another is Crohn’s Disease), is a chronic, progressive and disabling condition [1]. The clinical manifestation of UC mainly includes mucus bloody stool, recurrent diarrhea, and abdominal pain [2]. As a lifelong disease, the symptoms of UC can lead to a substantial negative impact on patient quality of life and incur a significant economic burden, including both direct medical costs and indirect costs associated with absenteeism and productivity loss [3]. The etiology of UC, however, remains not well identified and it may result from environmental factors, genetic predisposition, microbial dysbiosis, and immune dysregulation [4, 5]. The incidence of UC, a disease which previously more prevalent in high-income countries of Europe and North America has shifted towards industrialized countries such as Asia [6]. As a result, it has become a global refractory disease with worldwide shifting epidemiological characteristics [7].
There is no successful therapy that can treat UC so far, even surgery may be followed by ongoing morbidity [8]. Currently, the optimal strategy of management includes remission maintenance, prevention of disease-related complication, improvement of health-related quality of life and promotion of mucosal healing [9]. Pharmacological therapies, including 5-aminosalicylic acid, corticosteroids, immunosuppressants, biological agents, and other promising treatments (e.g., fecal microbiota transplantation) have been continuous developed, but some patients may experience gradual loss of response to the therapy while others may show intolerance to adverse effects of drugs, such as allergic reactions, digestive tract symptoms (e.g., flatulence, abdominal pain, nausea, and diarrhea), headache, and hypertension [10, 11]. As a result, an increasing number of UC patients (ranging between 21 and 60%) seek help from complementary and alternative medicine (CAM), especially Chinese medicine (CM) therapies, which has been practiced in Asia for thousands of years [12, 13].
As the most common interventions in CM practice, Chinese herbal medicines (CHM) have been widely used for UC due to the unique advantages of efficacy and safety [14]. An increasing number of evidence have shown that CHM have potentially positive effects on the relief of abdominal pain, diarrhea, and inflammation [15,16,17]. In CM theory, CHM interventions include Chinese medicinal substances (single herbs) and CHM formulas (namely “Fu-Fang”, or specific combinations of generally more than two Chinese medicinal substances). Since disease is a dynamic process, there may be different patterns in different phases of a disease. The success in deciding on a CHM prescription depends on an accurate pattern (zheng) diagnosis known as Bian-Zheng-Lun-Zhi (e.g., treatment based on pattern differentiation) [18]. However, previous studies published regarding the effectiveness of CM interventions for UC paid little attention to the application of pattern identification [19, 20]. In addition, we found that there is no latest review so far to provide the current clinical practice of CHM used for UC and its characteristics in study design [21].
This study aimed to investigate CHM applications for UC, especially based on CM pattern identification. The objectives were as follows: (1) to summarize the general characteristics of published UC clinical studies with CHM intervention(s); (2) to review the most frequently used CHM herbs and formulas, and the common types of CM patterns in UC; (3) to analyze the herbal correlations based on different pattern indications. The review will determine the current practice of CHM treatments for UC, and also identify the common problems (if any) in the previous research. These results will provide the basis for further studies regarding CHM based on pattern identification for UC.
Methods
Inclusion and exclusion criteria
This study included clinical studies of UC with CHM intervention(s) published in English and Chinese up to November 25, 2020. We included studies on subjects given the diagnosis of UC defined by clear diagnostic criteria or references, regardless of age, gender, course of disease and severity. The CHM interventions are typically administered as either single herbs or formulas (e.g., fixed or individualized formula, patent proprietary formula), which may have been administered alone or in combination with other interventions of conventional Western Medicine (WM) or CAM. No limitation on their formulation, preparation, dosage, dosage form or route of administration. The control intervention could be active, conventional medicine, placebo, no treatment, or other CAM treatments, etc. There were no limitations in the assessed outcomes. We considered randomized controlled trials (RCTs), quasi-randomized controlled trials, non-randomized controlled trials, observational clinical studies (e.g., cohort study or cross-sectional study) including the control group(s), case–control studies for inclusion. We excluded the following studies: repeated and withdrawal publications, studies with non-CHM interventions, comprehensive interventions focused on pharmacological treatment (or other CAM treatment) rather than CHM, plant extracts (e.g., plant-derived chemicals or synthetic chemicals which contain constituents of plants), clinical studies without a comparison or control group(s), study protocols, reviews, case series, case reports, abstracts or full-text reports not found, non-human studies, and non-English or non-Chinese language reports.
Search strategy
The following 7 databases, EMBASE, MEDLINE, Evidence-Based Medicine (EBM) Reviews, Allied and Complementary Medicine (AMED), The China National Knowledge Infrastructure (CNKI), VIP database, and Wanfang database were searched from the date of their inception to November 25, 2020. Languages were restricted to English and Chinese. The search terms were “ulcerative colitis”, “inflammatory bowel disease”, “Chinese medicine”, “Chinese materia medica”, “herbal formula”, “controlled trial”, “randomization”, and “clinical trial”, etc. The detailed search strategy is given in Additional file 1: Appendix S1. It is noted that the trial registration platforms (e.g., ClinicalTrials.gov) are not included in our search databases because (i) the records of some completed trials were duplication with their final publications, and (ii) some ongoing trials presented inadequate or absent details of CHM interventions which cannot meet the requirements of data collection in this review.
Screening
The titles and abstracts of the records were independently screened by two researchers (XHW and YX) based on inclusion and exclusion criteria, and the full texts of potentially suitable articles were retrieved for further assessment. Disagreements, if any, were resolved by discussion or consultation with the third researcher (XZ).
Data extraction
For each study, the following information was collected: article title, year of publication, study design and setting, sample size, clinical phases of UC, CM patterns (if any), CM treatment principles (if any), types and details of CHM interventions (including name, composition, preparation, dosage, dosage form, and administration route), integrative application of CHM and WM drugs (if any), treatment regimen (including duration of intervention and follow-up period), categories of the controls and outcomes, and safety evaluation. Each item was extracted by two researchers independently. Before extraction, they received a data extraction form and trained by an experienced researcher (XZ) to understand the criteria for each item. A third researcher (LZ) checked the extracted data based on Visual Basic for Applications (VBA) and made corrections (Additional file 1: Appendix S2). Any uncertainty regarding a particular data were resolved by consultation with the principal investigator (ZXB).
Data standardization
Due to a variety of expressions for the similar/same CM patterns and treatment principles, we standardize the data as a uniform and internationally recognized terminology which is easier for categorization and calculation. For example, we classified the phrases of “draining dampness”, “drying dampness”, “eliminating dampness”, “resolving dampness”, “dampness-dispelling” as one treatment principle. Also, we grouped pattern/syndrome of “dampness obstruction”, “dampness accumulation”, “dampness immersion”, and “dampness steaming” as the same type of CM pattern. All Chinese-to-English translations of terminology were deduced primarily from the international standards of “WHO International Standard Terminologies on Traditional Medicine in the West Pacific Region” and/or the “International Standard Chinese-English Basic Nomenclature of Chinese Medicine”, which were published by World Federation of Chinese Medicine Societies in 2007 [22,23,24]. The name of CHM interventions (including the herbs and formulas) was translated according to the Chinese Pharmacopoeia 2020 [25].
Statistical analysis
(1) Descriptive statistics: All data were collected and recorded in Microsoft Office Excel (Version 2016). Descriptive data were presented as number (n) and percent (%), or mean and standard deviations (SD). Data analyses were performed using SPSS software, version 25.0. (2) Association Rule Mining (ARM): The association rule, a well-recognized data mining and knowledge discovery approach, has been widely applied in medical areas. Based on IBM SPSS Modeler 18.0 software, the CHM herbs and formulas were analyzed by frequency, clustering and high-frequency herb using association rule, e.g., Apriori algorithm, to attempt to find rules and associations that exist between the prescriptions and pattern identifications.
Specifically, based on the descriptive data regarding to the frequency of herbs and formulas in the treatment of UC with different CM patterns, we used Apriori algorithm to determine the commonly used herb group (two or three-herbs combinations) and network analysis to determine the correlation of different herbs. The strength of an association rule could be measured by its support and confidence. We used the support level to determine the probability that A and B occurred simultaneously. The support of the item set A: s(A) = σ(A)/N; support for rule A ⟶ B: s (A ⟶ B) = σ(A ∪ B)/N. We used confidence to determine how frequently B occurred in transactions containing A: c (A ⟶ B) = σ(A ∪ B)/σ(A). The minimum rule confidence level was set as 80%, which indicated when A herb appeared, the appearance of B herb would be 80%, and the minimum conditional support was set to 20%. In addition, we used the lift to observe whether the two item sets were dependent on each other, for which value larger than 1 indicated the two item sets depended on each other [26]. After data preprocessing and correlation analysis between herbs, a directed network was constructed to connect herbs that were used together to summarize prescriptions based on different CM patterns. We converted the text information in the data source to a vector form, marked the annotation name herbs as the feature vector, and input them to the 0/1 structured herbs prescription table. Then, the table was imported into IBM SPSS Modeler 18.0 to create association rules flow, which could output the associated node herbs and their weight values. According to the frequency correlation between various CHM herbs, the IBM SPSS Modeler 18.0 software was used to classify the frequency into three types of correlation degree, including weak, between weak and strong, and strong link. We filtered a total of sixteen herbs in each CM pattern, which presented a strong association with the core herb (e.g., frequency more than 20). Then, we numbered the output nodes with strong associations created a list of the combination of nodes list and edges list, which was imported into Cytoscape 3.7.1 software to perform network image visualization.
Results
Search
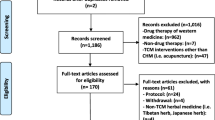
The initial search identified a total of 7890 records, of which 3238 relevant studies were retained after excluding duplicates and screening the titles and abstracts. After reviewing the full text of these publications, we identified 2311 articles for inclusion in our final analysis (Fig. 1).
Characteristics of included studies
The earliest clinical study of UC with CHM intervention included in this study was published in 1990. The total number particularly increased after 2007, reaching more than 100 per year and peaking during 2011–2016 (e.g., average number was 172 each year) (Fig. 2). The characteristics of included trials are shown in Table 1. Most included studies are RCT (93.6%) with parallel two arms (96.4%), but few included multicentre (2.9%) and blinding (3.0%) design. Sample size ranged from 10 to 2568, median 78 (inter-quartile range 60–100). Commonly, the clinical studies focused on active UC (71.2%), CHM formula interventions (99.1%) and active control (54.9%). There were 895 (38.7%) studies that considered CM pattern in the inclusion of UC participants, but 29.1% of them did not provide the diagnosis criteria. The fixed formula (58.1%) and decoction (87.2%) were reported in a majority among CHM formulas. Further, 38.6% CHM formulas were combined with Western medicine(s) in the application of clinical practice. In terms of administration route of CHM therapies for UC, external delivery (41.2%) is more common than oral route (34.9%). Few trials included CM-related indicators (22.7%), such as CM pattern scale questionnaire, and safety assessment (30.2%) in the outcomes. Among 697 studies that considered the adverse effect (AE) of CHM interventions, 67% identified no AEs while 33% reported the specific AEs (Additional file 1: Appendix S3).
Description of CHM treatments for UC
Among 2311 included studies, we identified a total of 245 kinds of CHM formulas (Additional file 1: Appendix S4) and the most frequently used prescription was Bai-Tou-Weng-Tang (frequency = 466), followed by Shen-Ling-Bai-Zhu-San (frequency = 276), Shao-Yao-Tang (frequency = 180), Bu-Zhong-Yi-Qi-Tang (frequency = 139), and Tong-Xie-Yao-Fang (frequency = 133). Around 26.3% of these top five CHM formulas were commonly combined with western medicines, such as Sulfasalazine and Mesalazine, in clinical practice. Details of their compositions, actions and indications are summarized in Table 2. Moreover, the most common herb used in practice was Huang Lian (frequency = 1528), followed by Bai Zhu (frequency = 1275), Gan Cao (frequency = 1210), Bai Shao (frequency = 1115), and Bai Tou Weng (frequency = 1045) and so on. We listed the top ten frequently used single herbs in Table 3. The application of patent proprietary CHM formula is very convenient in practice, we thereby provided the top five commonly used proprietary CHMs in Table 4, including Xi-Lei-San (frequency = 48), Yun-Nan-Bai-Yao (frequency = 18), Fu-Fang-Ku-Shen-Jie-Chang-Rong-Jiao-Nang (frequency = 13), Bu-Pi-Yi-Chang-Wan (frequency = 7), and Shen-Ling-Bai-Zhu-San (frequency = 7). Together, we provided Fig. 3 to summarize the top 5 frequently used CHM interventions.
CM zheng‑based CHM application and their relationships
Among 895 individual studies including CM zheng, we identified a total of 43 different CM patterns (zheng) for UC and particularly listed the top ten in Table 5. The most common pattern was Large intestine dampness-heat (Da Chang Shi Re) (frequency = 517), followed by Spleen-kidney yang deficiency (Pi Shen Yang Xu) (frequency = 192), Liver depression and spleen deficiency (Gan Yu Pi Xu) (frequency = 154), Spleen-stomach weakness (Pi Wei Xu Ruo) (frequency = 143), and Spleen deficiency with dampness accumulation (Pi Xu Shi Yun) (frequency = 76). According to these top five CM zheng of UC, we analyzed the herbal application and their interactions based on each CM pattern (Fig. 4). Generally, the core herbs (the biggest node with the deepest colorful) of each CM zheng were Huang Lian for the pattern of Large intestine dampness-heat, and Bai Zhu for the other four patterns of Spleen-kidney yang deficiency, Liver depression and spleen deficiency, Spleen-stomach weakness, and Spleen deficiency with dampness accumulation. We also identified a total of fifteen commonly herbs which were closely related to the core herb of each pattern. The thicker lines with darker colorful represents the stronger correlation to the core herb in clinical application. For example, Huang Lian was closely related to Bai Tou Weng, Huang Bai, Huang Qin, Bai Shao, Mu Xiang, Bai Ji, Bai Zhu and Gan Cao for the treatment of Large intestine dampness-heat. Bai Zhu, as the core herb of other four CM zheng, was usually combined with Dang Shen, Fu Ling, Gan Cao, Huang Lian and Mu Xiang. But there were some differences in herbal compatibility for each CM pattern, which are presented in Fig. 4a–e.
Discussion
This study provides a comprehensive review of the characteristics of CHM treatments for UC in the past 30 years, which have identified a remarkable increase in the number of publications after 2007. In this review, we have identified that the most common studied condition(s), intervention(s) and comparison(s) of included articles were active UC, CHM fixed formula in decoction, and active control. Most included studies are RCT with design of parallel two arms, single centre, and open label. It is important to note that only 697 (30.2%) trials mentioned the safety assessment of CHM interventions, of which 230 (33.0%) articles reported the specific adverse effects (e.g., symptoms of the gastrointestinal tract, etc.). The reasons of there are less emphasized in safety consideration of clinical studies might be the mistakenly assumption of Chinese medicinal substances originating from natural sources are harmless [27]. However, adverse effects derive from unpredictable adverse events, improper use, contamination, misidentification, and herb-drug interactions [28]. Inadequate or absent reporting of safety evaluation on CHM interventions greatly degrades the scientific evidence of clinical trials. Therefore, we recommend that the future clinical studies should pay more attention to the high standard of study design, especially for the randomized, multicentre, double blind, placebo control (or double-dummy), and large sample size.
Moreover, although the CM pattern differentiation is critical in the determination of CHM interventions, there are only 895 (38.7%) studies that adopted the CM pattern diagnosis for the inclusion of UC participants and 524 (22.7%) articles that included CM-related outcomes, such as pattern scale questionnaire. In a CHM interventional trial, if the CM pattern is included, the concept of pattern differentiation should be carried out throughout the entire process with regard to the rationale of the study design, selection of inclusion and exclusion criteria, CHM formula prescription, selection of outcome measures and data interpretation, etc. In clinical practice, the CHM treatment is guided with CM principles and determined by pattern differentiation. If the pattern of a condition is misdiagnosed, the treatment principles will be incorrect, and its derivative CHM formula will be ineffective. Therefore, we recommend that the reporting of such studies should follow the guideline of “CONSORT Extension for Chinese Herbal Medicine Formulas 2017: Recommendations, Explanation, and Elaboration", especially for the reporting of details and rationale regarding the definite diagnostic criteria of studied CM pattern, correspondence between pattern identification and CHM formula (e.g., Fang-Zheng-Dui-Ying), and CM-related outcome(s) [29, 30].
In this review, we systematically examined the use of single herbs, CHM fixed formulas, individualized formulas and patent proprietary formulas, and the combination of CHM and Western medicine in the clinical practice of UC. We identified a total of 245 types of CHM formulas and further summarized the top five frequently used formulas and top ten commonly herbs. Specifically, the classic CHM formula included Bai-Tou-Weng-Tang, Shen-Ling-Bai-Zhu-San, Shao-Yao-Tang, Bu-Zhong-Yi-Qi-Tang, and Tong-Xie-Yao-Fang. Sulfasalazine and Mesalazine are the most common concomitant western medicines for CHM formulas. The patent proprietary CHM formulas are Xi-Lei-San (enema), Yun-Nan-Bai-Yao, Fu-Fang-Ku-Shen-Jie-Chang-Rong-Jiao-Nang, Bu-Pi-Yi-Chang-Wan, and Shen-Ling-Bai-Zhu-San. It is indicated that the administration route of CHM interventions for UC not only include oral delivery, but also have the external use with directly effect, such as enema. The most common herbs in practice mainly focused on the types of heat-clearing, dampness-draining, toxin-removing, spleen-invigorating, qi-moving, and blood-stopping, such as Huang Lian, Huang Bai, Bai Tou Weng, Bai Zhu, Gan Cao, Bai Shao, Huang Qi, Dang Shen, Mu Xiang, and Bai Ji. More than half of these identified CHM therapies are consistent with the recommendations of “Experts-based consensus of integrative Chinese and western medicine treatment for ulcerative colitis (2017 version)” [31]. Moreover, the results also provide the basis and reference for the future update of clinical practice guideline for UC in terms of CM diagnosis and treatment.
According to CM theory, zheng (pattern) is a pathological cluster or summary of signs and symptoms at a certain stage of a disease, which reflect the relationship between the pathogens and the body’s resistance [32]. Practically, pattern identification refers to the analysis and summarization of the clinical symptoms obtained through the four diagnostic methods of CM (inspection, auscultation and smell, inquiry, and pulse taking and palpation), after which CM practitioners can accordingly determine the therapeutic principles and select the appropriate CHM treatments based on the patient’s current essential pattern [33, 34]. In this study, we found that the most common CM zheng of UC patients were the patterns of Large intestine dampness-heat, Spleen-kidney yang deficiency, Liver depression and spleen deficiency, Spleen-stomach weakness, and Spleen deficiency with dampness accumulation, which reflected the progress of UC with different phases. Through the association analysis on herbal applications and their relationships, we formulated one core herb with fifteen commonly combined herbs for each CM pattern. Specifically, in the CM pattern of Large intestine dampness-heat, Huang Lian, a typical heat-clearing and dampness-drying medicinal, was more frequently combined with the following three categories of herbs: (i) dispelling and heat-clearing medicinal, including Bai Tou Weng, Huang Bai, and Huang Qin; (ii) harmonizing qi and blood medicinal, including Bai Shao, Mu Xiang, Dang Gui, and Bai Ji; and iii) tonifying qi and invigorating spleen medicinal, including Bai Zhu and Gan Cao. Among these, the compatibility of blood-activating and qi-moving medicinals was very important due to the identification of strong correlations between Mu Xiang and Bai Shao/Gan Cao. Besides, herbs of invigorating spleen and draining dampness (e.g., Dang Shen, Huang Qi, Fu Ling, Yi Yi Ren) and astringent hemostatic (e.g., Di Yu) could be supplemented in the CHM formula for the treatment of UC with Large intestine dampness-heat pattern (Fig. 4a).
For the remaining four CM patterns, Bai Zhu, as their common core herb, was usually combined with Dang Shen, Fu Ling, and Gan Cao to treat the pattern of spleen deficiency which is the basic type included in the four patterns. In addition, Huang Lian and Mu Xiang were commonly added in the prescriptions to treat the four patterns, due to their role of heat-clearing, dampness-drying, and qi-moving. However, there are some differences among each specific pattern. In terms of Spleen-kidney yang deficiency, herbs of warming and tonifying yang qi, astringing intestines and checking diarrhea were emphasized, including Bu Gu Zhi, Rou Dou Kou, Wu Zhu Yu, and Huang Qi (Fig. 4b). For the pattern of Liver depression and spleen deficiency, Bai Shao is another vital herb, similar to the core herb of Bai Zhu, which was associated with Chai Hu, Fang Feng and Chen Pi to achieve soothing liver, emolliating liver, regulating qi and relieving depression (Fig. 4c). Compared the two patterns of Spleen-stomach weakness and Spleen deficiency with dampness accumulation, the former presented more correlations between the core herb and tonifying qi and invigorating spleen medicinal, such as Shan Yao and Huang Qi (Fig. 4d); the latter focused on the draining or drying dampness medicinal, such as Yi Yi Ren, and added more herbs for clearing heat, removing toxin, cooling blood, and stopping bleeding, such as Di Yu, Bai Ji, Bai Jiang Cao, and Bai Tou Weng (Fig. 4e). Based on the results of herbal correlation analysis, the CM treatment principles for UC could be summarized as clear heat and dampness, tonify and strength spleen, and harmony qi and blood.
This study has some limitations. First, this review identified articles published up to 25 November 2020 in the targeted seven databases. Any records which had not been included in these databases by that cut-off period have not been included. In addition, we included only articles in English and Chinese because of language limitations. As such, we may not have captured otherwise eligible trials published in other languages. Second, the data were extracted from clinical studies that used seven different types of design, including both interventional and observational studies (e.g., RCTs, cohort study, case–control study, etc.). The quality of these studies varied and therefore it is difficult to compare them quantitatively. Thus, we only provided the descriptive analysis for the general characteristics of included studies, not included the methodology and reporting quality assessments.
Conclusion
This review examined the application of CHM interventions for UC and summarized the 10 most frequently used single herbs, the 5 most frequently used CHM formulas and patent proprietary formulas, and the combined use of CHM and Western medicine treatments. The characteristics of CM pattern identification in UC and their herbal prescription in practice were also analyzed.
Availability of data and materials
The data used for this study are included in the manuscript and additional file.
Abbreviations
- UC:
-
Ulcerative colitis
- CHM:
-
Chinese herbal medicines
- CAM:
-
Complementary and alternative medicine
- CM:
-
Chinese medicine
- WM:
-
Western Medicine
- RCTs:
-
Randomized controlled trials
- EBM:
-
Evidence-Based Medicine
- AMED:
-
Allied and Complementary Medicine
- CNKI:
-
China National Knowledge Infrastructure
- ARM:
-
Association Rule Mining
References
Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology. Practice Parameters Committee Am J Gastroenterol. 2010;105:501–23.
Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-De Acosta M, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis 2017;11:649–70.
Cohen RD, Yu AP, Wu EQ, Xie J, Mulani PM, Chao J. Systematic review: the costs of ulcerative colitis in Western countries. Aliment Pharmacol Ther. 2010;31:693–707.
Kugathasan S, Fiocchi C. Progress in basic inflammatory bowel disease research. Semin Pediatr Surg. 2007;16:146–53.
Dulai PS, Jairath V. Acute severe ulcerative colitis: latest evidence and therapeutic implications. Ther Adv Chronic Dis. 2018;9:65–72.
Targownik LE, Singh H, Nugent Z, Bernstein CN. The epidemiology of colectomy in ulcerative colitis: results from a population-based cohort. Am J Gastroenterol. 2012;107:1228–35.
Vegh Z, Kurti Z, Lakatos PL. Epidemiology of inflammatory bowel diseases from west to east. J Dig Dis. 2017;18(2):92–8.
Feuerstein JD, Cheifetz AS. Ulcerative colitis: epidemiology, diagnosis, and management. Mayo Clin Proc. 2014;89:1553–63.
Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019;114(3):384–413.
Regan BP, Bousvaros A. Pediatric ulcerative colitis: a practical guide to management. Paediatr Drugs. 2014;16:189–98.
Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18:191–8.
Nguyen GC, Croitoru K, Silverberg MS, Steinhart AH, Weizman AV. Use of complementary and alternative medicine for inflammatory bowel disease is associated with worse adherence to conventional therapy: the COMPLIANT study. Inflamm Bowel Dis. 2016;22(6):1412–7.
Langhorst J, Wulfert H, Lauche R, Klose P, Cramer H, Dobos GJ, et al. Systematic review of complementary and alternative medicine treatments in inflammatory bowel diseases. J Crohns Colitis. 2015;9(1):86–106.
Zhang C, Jiang M, Lu A. Considerations of traditional Chinese medicine as adjunct therapy in the management of ulcerative colitis. Clin Rev Allergy Immunol. 2013;44:274–83.
Dai YC, Zheng L, Zhang YL, Chen X, Chen DL, Tang ZP. Effects of Jianpi Qingchang decoction on the quality of life of patients with ulcerative colitis: A randomized controlled trial. Medicine. 2017;96:16.
Zhou TM, Yang SW, Wang JB. Effects of Shenlingbaizhu powder combined with mesalazine in the treatment of ulcerative colitis and the influence of NLRP3 inflammasome. Chin J Clin Pharm Therap. 2018;23:319–24.
Xiao HT, Peng J, Hu DD, Lin CY, Du B, Tsang SW, et al. Qing-dai powder promotes recovery of colitis by inhibiting inflammatory responses of colonic macrophages in dextran sulfate sodium-treated mice. Chin Med. 2015;10:29.
Chung V, Ho R, Wu X, Wu I. Incorporating traditional Chinese medicine syndrome differentiation in randomized trials: methodological issues. Eur J Integr Med. 2016;8:898–904.
Wang X, Zhao NQ, Sun YX, Bai X, Si JT, Liu JP, et al. Acupuncture for ulcerative colitis: a systematic review and meta-analysis of randomized clinical trials. BMC Complement Med Ther. 2020;20:309.
Sun YX, Wang X, Liao X, Guo J, Hou WB, Wang X, et al. An evidence mapping of systematic reviews and meta-analysis on traditional Chinese medicine for ulcerative colitis. BMC Complement Med Ther. 2021;21:228.
Zheng YY, Wang X, Si JT, Sun YX, Hou WB, Liu JP, et al. Randomized Clinical Trials of Traditional Chinese Medicines for Treating Ulcerative Colitis: A Scoping Review. World J Tradit Chin Med. 2021;7(3):326–31.
WHO Regional Office for the Western Pacific. WHO International Standard Terminologies on Traditional Medicine in the Western Pacific Region; 2007.
World Health Organization. Regional Office for the Western Pacific. WHO international standard terminologies on traditional medicine in the Western Pacific Region. Manila: WHO Regional Office for the Western Pacific; 2007. http://www.who.int/iris/handle/10665/206952.
Li ZJ. International standard Chinese-English basic nomenclature of Chinese medicine. Beijing: People’s Medical Publishing House; 2007.
Chinese Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China (Volume 1). 2020 Edition: China Medical Science Press; 2020.
Yang DH, Kang JH, Park YB, Park YJ, Oh HS, Kim SB. Association Rule Mining and Network Analysis in Oriental Medicine. PLoS ONE. 2013;8(3):e59241.
Ng SC, Lam YT, Tsoi KK, Chan FK, Sung JJ, Wu JC. Systematic review: the efficacy of herbal therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2013;38(8):854–63.
Wu TX, Li YP, Bian ZX, Li TQ, Li J, Dagenais S, et al. Consolidated standards for reporting trials of traditional Chinese medicine (CONSORT for TCM). Zhong Guo Xun Zheng Yi Xue Za Zhi. 2007;7:601–5.
Zhang X, Tian R, Zhao C, Birch S, Lee JA, Alraek T, et al. The use of pattern differentiation in WHO-registered traditional Chinese medicine trials - A systematic review. Eur J Integr Med. 2019;30:100945.
Cheng CW, Wu TX, Shang HC, Li YP, Altman DG, Moher D, et al. CONSORT Extension for Chinese Herbal Medicine Formulas 2017: Recommendations, Explanation, and Elaboration. Ann Intern Med. 2017;167(2):112–21.
Specialized Committee of Digestive System Diseases, Chinese Society of Integrative Medicine. Experts-based recommendations of integrative Chinese and western medicine treatment for ulcerative colitis. Chin J Integr Trad West Med Dig 2018;26(2):105–11.
Ma SR, Liu XR. The Foundations of Chinese Medicine. Beijing: China Press of Tradit Chin Med; 2015. p. 24–5.
Eisenstein M. Ulcerative colitis: towards remission. Nature. 2018;563(7730):S33.
David C. Why Chinese medicine is heading for clinics around the world. Nature. 2018;561(7724):448–50.
Acknowledgements
The authors acknowledge the financial supports of Health@InnoHK Initiative Fund of the Hong Kong Special Administrative Region Government (ITC RC/IHK/4/7), and China Center for Evidence Based Traditional Chinese Medicine, CCEBTM (2020YJSZX-5).
Funding
Health@InnoHK Initiative Fund of the Hong Kong Special Administrative Region Government (ITC RC/IHK/4/7), and China Center for Evidence Based Traditional Chinese Medicine, CCEBTM (2020YJSZX-5). The funders had no role in the design of the study, in the collection, analysis, and interpretation of data, nor in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
ZXB and XZ designed and drafted this article; XHW, YX, LZ and XZ searched and screened the articles; LZ, WFX, YX, XW, FL, CCZ, WCC and XZ extracted and checked the data; XZ, LZ, and CPC assessed and analyzed the data; JXM and ZXB provided critical comments for the article; XZ and ZXB revised and finalized the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix S1.
Search Strategy. Appendix S2. Correction script for data check. Appendix S3. Reported adverse effects of included studies. Appendix S4. Full name list of summarized CHM formulas.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, X., Zhang, L., Chan, J.C.P. et al. Chinese herbal medicines in the treatment of ulcerative colitis: a review. Chin Med 17, 43 (2022). https://doi.org/10.1186/s13020-022-00591-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-022-00591-x