Abstract
Background
The objective of this study is to investigate whether the use of antegrade perfusion with terminal non-cardioplegic warm blood (TNWB) before aortic unclamping in single-clamp technique coronary artery bypass has a positive impact on intraoperative heartbeat recovery.
Methods
Between December 2022 and May 2023, 40 consecutive patients undergoing coronary artery bypass using single-clamp technique were randomized into one of two groups: the TNWB group received an antegrade perfusion with TNWB before removing the aortic cross-clamp (n = 20), while the control group did not receive (n = 20). The time intervals between coronary perfusion and the onset of the first heartbeats and sinus rhythms, occurrences of spontaneous sinus rhythm, intraoperative defibrillation requirements, as well as postoperative CK-MB and troponin T levels were recorded and subjected to analysis.
Results
In the TNWB group, the median onset of the first heartbeats after the initiation of coronary perfusion was 34 s (4-100), while in the control group, it was 90 s (15–340) (p < 0.001). The median onset of the sinus rhythms was 100 s (28–290) in the TNWB group and was 132 s (45–350) in the control group (p = 0.023). The occurrence of intraoperative arrhythmias was 15% in the TNWB group compared to 50% in the control group (p = 0.018), and the incidence for internal defibrillation was 5% in the TNWB group and was 30% in the control group (p = 0.037). The TNWB group showed the median CK-MB levels at 6 h postoperative was 14.10 ng/mL (9.78–19.26), compared to 18.31 ng/mL (13.98–23.80) in the control group (p = 0.045).
Conclusions
During single clamp coronary artery bypass, administration TNWB into the aortic root before aortic unclamping has the potential to enhance heartbeat recovery, as evidenced by the shortened time to the initial heartbeat and the establishment of sinus beats following coronary perfusion.
Trial registration
Trial registration number (Study ID): TCTR20231002003.
Similar content being viewed by others
Background
A comprehensive myocardial preservation strategy is a tailored approach used by cardiac surgeons to protect the heart muscle during surgery, aiming to improve patient outcomes and minimize complications [1, 2]. Reperfusion with warm blood before aortic unclamping is crucial for minimizing ischemia-reperfusion injury and promoting recovery post-cardiac surgery, warranting careful consideration and ongoing research [3].
The single-clamp technique coronary artery bypass grafting (CABG) is a particular cardiac procedure, first described by Salerno in 1982, where gradual coronary reperfusion is achieved for each grafted coronary vessel throughout aortic cross-clamping [4, 5]. Following aortic unclamping and during cardiopulmonary bypass, the perfusion pressure tends to be lower than normal and lacks pulsatility during the initial phase. Heart distention, vasoconstriction, and vasodilatation result in uncontrolled coronary autoregulation. In the single-clamp technique coronary artery bypass, once all the anastomoses are completed, the opportunity to regulate and ensure sufficient coronary blood flow occurs solely before the aortic unclamping. While non-cardioplegic warm blood seems to enhance the energy charge for heartbeat recovery and washout of the waste products, there is a shortage of reports assessing the effectiveness of TNWB in the single-clamp technique for coronary artery bypass. We postulated that addition of TNWB before aortic unclamping might improve heartbeat recovery and provide smooth weaning from cardiopulmonary bypass.
Methods
Between December 2022 and May 2023, 40 consecutive patients undergoing coronary artery bypass using the single-clamp technique were randomized into two groups: the TNWB group, which received antegrade perfusion with TNWB before removing the aortic cross-clamp (n = 20), and the control group, which did not receive this perfusion (n = 20). We recorded and analyzed the time intervals between coronary perfusion and the onset of the first heartbeats and sinus rhythms, occurrences of spontaneous sinus rhythm, intraoperative defibrillation requirements, and perioperative CK-MB and troponin T levels.
This study has been approved by Human Ethics Committee of Thammasat University (MTU-EC-SU-1-051/66).
Patient selection
Patients with significant left anterior descending (LAD) artery stenosis and at least another major coronary artery stenosis planned for coronary artery bypass were included in the study. The exclusion criteria comprised (1) emergency surgery, (2) ejection fraction lower than 30%, (3) combined cardiac-associated operative procedure, (4) recent myocardial infarction (within the last 4 weeks), and (5) age exceeding 80 years. Randomization was performed by opening a sealed envelope at the time of incision. Patients whose left internal mammary artery (LIMA) to LAD anastomosis could not be achieved or who had an aortic clamp time exceeded 120 min were omitted from the study.
Sample size calculation
The sample size for this study was calculated to ensure sufficient statistical power to detect significant differences in heartbeat recovery outcomes between the TNWB and control groups. Using data from a previous study by Susumu et al. (2006) [12], the sample size was determined based on a standardized effect size, with an α of 0.05 and a β of 0.20. The estimated minimum sample size was 17 patients per group. To account for potential dropouts, an additional 10% was added, resulting in a target of 20 patients per group for the primary outcome analysis. Consequently, the research team estimates a total of 40 participants will be required for the study.
Randomization
Patients were block randomized according to a computer-generated list. The allocations were concealed until the date of the operation. Participants were recruited by the surgical team, and the allocation of groups was disclosed to the perfusionist at the beginning of the operation and to the surgeon after the proximal anastomosis was completed.
Operative technique
All patients received standard anesthesia. A median sternotomy was performed. Both the left internal mammary artery (LIMA) and arterial or venous grafts were prepared. Routine cardiopulmonary bypass (CPB) was carried out under mild hypothermia (32oC). Myocardial preservation was achieved using antegrade whole blood cardioplegia administered at a cold temperature. Distal and proximal anastomoses were consequently constructed during a single period of aortic cross-clamp. Additional cardioplegia was delivered upon completion of each proximal anastomosis or after 20 min. Finally, grafting of the left anterior descending artery with the left internal thoracic artery was performed following the sequential completion of arterial graft or saphenous vein graft anastomoses. The patient’s body temperature was maintained at 32 °C during cardiopulmonary bypass. Systemic rewarming commenced during the final construction of the proximal anastomosis and prior to grafting of the left anterior descending artery.
After completion of the procedure and adequate rewarming, weaning from cardiopulmonary bypass was conducted according to the established protocol. During this period, occurrences of arrhythmia, the need for defibrillation, and pacing requirements were recorded. The inotropic agent for the weaning-off process was primarily dobutamine at a dosage of 5 mcg/kg/min. Decannulation took place upon achieving hemodynamic stability.
Myocardial protection
Patient blood was obtained from the oxygenator and combined with a prepared cardioplegic solution (containing 16 mEq of potassium in 20 mL) to provide whole blood cardioplegia with a potassium concentration of 16 mEq/L. This mixture was delivered at a cold temperature (14–16 °C) through the antegrade route. The infusion protocol involved administering the initial dose of 20 mL/kg within 3 min, with subsequent doses administered following the completion of each proximal anastomosis or after 15–20 min, as needed.
Technique of TNWB
In the TNWB group, warm blood at 36 °C was infused into the aortic root via the antegrade cardioplegia cannula before aortic unclamping. This was maintained at a targeted flow rate of 250 ml/min for 3 min, which corresponds to normal resting coronary blood flow. For the safety reason, the pressure is limited at 150 mmHg to commence coronary perfusion. In the control group, coronary perfusion begins after aortic unclamping.
Endpoints
The primary endpoint for this study is heartbeat recovery, specifically the duration to the first heartbeat and sinus beat following coronary perfusion. First heartbeat referred to the first observable heart contraction following coronary perfusion. A sinus beat could describe based on the electrocardiogram (ECG), in which the P-wave was upright and preceded each QRS complex. Coronary perfusion began in the TNWB group with the initiation of TNWB, whereas in the control group, it commenced upon aortic unclamping. Spontaneous heartbeat recovery is evidenced when electrical activity in the monitor was observed, and the patient could wean off from cardiopulmonary bypass without the need for electrical defibrillation or pacing.
The secondary endpoint is the safety analysis of TNWB. The decision to use temporary pacing before discontinuing cardiopulmonary bypass depended on the patient’s condition, ensuring optimal cardiac function during the transition, particularly in bradyarrhythmias and atrioventricular block. The decision to use defibrillation was considered in the event of ventricular fibrillation or ventricular tachycardia. CK-MB and troponin T levels were evaluated at two time points: prior to aortic cross-clamp and 6 h post-operation upon arrival in the ICU.
Statistics
STATA 16.0 was utilized for data analysis. Normal distributed continuous data were expressed as the mean ± SD, and Student’s t-test was used to compare the two groups. Non-normal distributed continuous data were expressed as a median with the interquartile range (25th to 75th percentiles), and the Mann-Whitney test was used to compared the two groups. Nominal data were expressed as number and percentage, and the two-tailed Fisher’s test was used for analyses. The normality of the data was assessed using both the Shapiro-Wilk test and histograms. Statistical significance was considered at a p < 0.05.
Results
The patient characteristics data showed no significant differences between the two groups, as summarized in Table 1.
Intraoperative data is shown in Table 2. There were no significant differences among the two groups in terms of cardiopulmonary bypass time, aortic clamping time, number of vessels grafted. The time interval from coronary perfusion to the first heartbeat was shorter in the TNWB group compared to the control group (TNWB: 34 s (4-100) vs. control: 90 s (15–340), p < 0.001). Similarly, the time interval from coronary perfusion to sinus beat was also shorter in the TNWB group compared to the control group (TNWB: 100 s (28–290) vs. control: 132 s (45–350), p = 0.023). The incidence of intraoperative arrhythmia was lower in the TNWB group compared to the control group (15% vs. 50%, p = 0.018). Additionally, the defibrillation rate was 5% in the TNWB group and 15% in the control group (p = 0.037). Spontaneous heartbeat recovery was more evident in the TNWB group than in the control group (85% vs. 65%, p = 0.144), although the difference did not reach statistical significance. There were no differences in the need for temporary pacing, or mechanical support between both groups.
The postoperative course, as shown in Table 2, revealed no significant differences in time to extubation, occurrence of atrial fibrillation, need for reoperation, and length of ICU stay between the groups.
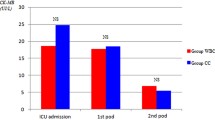
The concentrations of perioperative cardiac markers are displayed in Figs. 1 and 2. Initial measurements of both CK-MB and troponin T before aortic clamping showed no significant differences between the TNWB and control groups. Importantly, CK-MB at 6 h postoperatively was significantly lower in the TNWB group compared to the control group (TNWB: 14.10 ng/mL (9.78–19.26) vs. control: 18.31 ng/mL (13.98–23.80), p = 0.045). However, serum cardiac troponin T levels at 6 h postoperatively did not differ significantly between the two groups.
Serum concentration of CK-MB (ng/mL) before aortic cross-clamp, and 6 h post-op. Data are presented as median (IQR). The upper and lower borders of the box represent the upper and lower quartiles. The middle horizontal line represents the median. The upper and lower whiskers represent the maximum and minimum values of nonoutliers
Serum concentration of Trop T (ng/mL) before aortic cross-clamp, and 6 h post-op. Data are presented as median (IQR). The upper and lower borders of the box represent the upper and lower quartiles. The middle horizontal line represents the median. The upper and lower whiskers represent the maximum and minimum values of nonoutliers
Discussion
The primary finding of our experiment is that the TNWB group demonstrated a shorter time to the first heartbeat and initial sinus rhythm after coronary perfusion, indicating improved myocardial recovery. This is a significant indicator of effective myocardial protection, as the recovery of the heartbeat is regarded as a key metric [12].
Furthermore, no significant differences were observed between the TNWB and control groups in the early postoperative course regarding time to extubation, arrhythmia, reoperation, or length of ICU stay, indicating that TNWB is safe and does not adversely affect these outcomes.
These results highlight the potential benefits of TNWB in enhancing myocardial recovery without compromising patient safety in the early postoperative period. Future studies should continue to explore the long-term outcomes and mechanisms underlying these benefits to further validate the efficacy and safety of TNWB in coronary artery bypass surgery.
Rationale behind TNWB
The rationale for using TNWB in our study is grounded on scientific principles including: (1) the single clamp technique in CABG already achieves a gradual revascularization of the ischemic myocardium for each grafted coronary vessel, (2) by administering cardioplegia through blood mixtures and repeating it after each set of coronary grafting, a gradual reperfusion of the ischemic myocardium seemed to occur, (3) once all the anastomoses were completed, the opportunity to regulate and ensure sufficient coronary blood flow occurs solely before the aortic unclamping, and (4) a non-cardioplegic warm blood may be a more optimal choice than using a high-potassium solution, which has potential adverse effects, to enhance the energy charge for heartbeat recovery and washout of the waste products in the brief period before aortic unclamp.
The ‘single-clamp technique’ in coronary artery bypass surgery involves creating both distal and proximal anastomoses during a single period of aortic cross-clamping. This method allows for gradual coronary reperfusion with each grafted vessel and enhances myocardial protection through the administration and repetition of blood cardioplegia after each proximal anastomosis [5]. At our institute, intermittent antegrade whole blood cardioplegia, which reduces the use of crystalloid solutions, has been routinely used in coronary bypass procedures for the past decade. Literature supports its benefits, maintaining myocardial protection, mortality, and morbidity without compromise [6, 7]. We observe similar advantages at our institution.
Following aortic unclamping, the flow and pressure decreased, heart distended, presence of vasoconstrictors or vasodilators influence the range of coronary autoregulation uncontrolled. In the single-clamp technique coronary artery bypass, once all the anastomoses are completed, the opportunity to regulate and ensure sufficient coronary blood flow occurs solely before the aortic unclamping. TNWB technique, the infusion is carried out at a flow rate of 250 ml/min, mimicking normal resting coronary blood flow. The perfusion is maintained at a pressure of 100–150 mmHg, and the perfusion time is set at 3 min, mirroring the conditions of the initial antegrade cardioplegic perfusion.
Elevated potassium level associated with potential adverse effects [8], which further enhances myocardial damage, by limiting myocardial perfusion [9]. Another significant aspect of high K+ levels is the differential sensitivity of the atria and ventricles to high potassium. This discrepancy can contribute to an arrhythmogenic substrate between the chambers during reanimation after cold-diastolic arrest [10]. Considering that blood possesses inherent properties as a potent buffering effect of oxygen-derived free radicals, which may be released during reperfusion, opting for a non-cardioplegic warm blood could be considered a more optimal choice compared to using a high-potassium solution in the brief period before aortic unclamp.
Although there have been several randomized controlled trials exploring the benefits of warm blood hyperkalemic perfusion (Hot shot) in various settings, often administered retrogradely, studies focusing on antegrade non-cardioplegic warm blood perfusion before aortic unclamping are rare [11,12,13]. Further validation of this strategy is necessary.
Cardiac markers
Elevated levels of CK-MB and troponin T in the blood are indicators of myocardial damage, often correlating with the extent of injury. The release of CK-MB into the bloodstream typically occurs within 4–6 h after the onset of myocardial injury, peaking around 18–24 h, and returning to normal levels within 48–72 h. Troponin T levels rise within 3–4 h after the onset of myocardial injury, peak at around 12–48 h, and can remain elevated for several days [14, 15]. Our data show a significant difference in CK-MB levels at 6 h postoperatively between the groups, while troponin T levels did not differ significantly. This discrepancy may be attributed to the limited 6-hour window for collecting enzyme levels. However, these cardiac markers were secondary endpoints for assessing the safety of TNWB. Extending the sample collection time to 12–48 h would provide a clearer conclusion on this matter.
Conclusion
Administering TNWB into the aortic root before aortic unclamping is a simple and efficient procedure that can be performed at the operating table. Our study suggests that incorporating TNWB before aortic unclamping in single-clamp technique coronary artery bypass surgery can enhance myocardial protection. This method has the potential to improve heartbeat recovery, as shown by the shortened time to the initial heartbeat and the establishment of sinus rhythm following coronary perfusion. While TNWB may not significantly impact clinical outcomes, it could serve as an adjunct in a multimodal myocardial protection strategy for single-clamp technique coronary artery bypass surgery.
Limitations
This was a small randomized controlled trial (RCT) focusing on the single-clamp technique for coronary artery bypass grafting (CABG). The findings of this study should be considered applicable to a similar set of myocardial protection protocols.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- TNWB:
-
terminal non-cardioplegic warm blood
- CABG:
-
coronary artery bypass graft
- CPB:
-
cardiopulmonary bypass
- LAD:
-
left anterior ascending artery
- LIMA:
-
left internal mammary artery
- LVEF:
-
left ventricular ejection fraction
- LM:
-
left main coronary artery
- COPD:
-
chronic obstructive pulmonary disease
References
Hausenloy DJ, Boston-Griffiths E, Yellon DM. Cardioprotection during cardiac surgery. Cardiovasc Res. 2012;94(2):253–65.
Buckberg GD. Update on current techniques of myocardial protection. Ann Thorac Surg. 1995;60(3):805–14.
Teoh KH, Christakis GT, Weisel RD, Fremes SE, Mickle DA, Romaschin AD, Harding RS, Ivanov J, Madonik MM, Ross IM, et al. Accelerated myocardial metabolic recovery with terminal warm blood cardioplegia. J Thorac Cardiovasc Surg. 1986;91(6):888–95.
Salerno TA. Single aortic cross-clamping for distal and proximal anastomoses in coronary surgery: an alternative to conventional techniques. Ann Thorac Surg. 1982;33(5):518–20.
Weisel RD, Hoy FB, Baird RJ, Burns RJ, Mickle DA, Ivanov J, Madonik MM, McLaughlin PR. Improved myocardial protection during a prolonged cross-clamp period. Ann Thorac Surg. 1983;36(6):664–74.
Vinten-Johansen J. Whole blood Cardioplegia: do we still need to dilute? J Extra Corpor Technol. 2016;48(2):9–14.
Borden RA 2nd, Ball C, Grady PM, Toth AJ, Lober C, Bakaeen FG, Tong MZ, Soltesz EG, Blackstone EH, Roselli EE. Microplegia vs 4:1 blood Cardioplegia: effectiveness and cost savings in Complex Cardiac operations. Ann Thorac Surg. 2020;110(4):1216–24.
Sellke FW, Boyle EM Jr, Verrier ED. Endothelial cell injury in cardiovascular surgery: the pathophysiology of vasomotor dysfunction. Ann Thorac Surg. 1996;62(4):1222–8.
He GW. Endothelial function related to vascular tone in cardiac surgery. Heart Lung Circ. 2005;14(1):13–8.
Dobson GP, Faggian G, Onorati F, Vinten-Johansen J. Hyperkalemic cardioplegia for adult and pediatric surgery: end of an era? Front Physiol. 2013;4:228.
Caputo M, Dihmis WC, Bryan AJ, Suleiman MS, Angelini GD. Warm blood hyperkalaemic reperfusion (‘hot shot’) prevents myocardial substrate derangement in patients undergoing coronary artery bypass surgery. Eur J Cardiothorac Surg. 1998;13(5):559–64.
Susumu I, Kiyotaka I, Shinichi S, Keiji U, Naoki H, Hiromasa Y, Yoshinori T. Benefits of terminal noncardioplegic warm blood retrograde perfusion after terminal warm blood cardioplegia perfusion prior to aortic unclamping in open heart surgery. J Cardiovasc Surg (Torino). 2006;47(6):677–82.
Rergkliang C, Chetpaophan A, Chittithavorn V, Vasinanukorn P, Chowchuvech V. Terminal warm blood cardioplegia in mitral valve replacement: prospective study. Asian Cardiovasc Thorac Ann. 2006;14(2):134–8.
Chin CT, Wang TY, Li S, Wiviott SD, deLemos JA, Kontos MC, Peterson ED, Roe MT. Comparison of the Prognostic Value of Peak Creatine Kinase-MB and troponin levels among patients with Acute myocardial infarction: a report from the Acute Coronary treatment and intervention Outcomes Network Registry–get with the guidelines. Clin Cardiol. 2012;35:424–9.
Newby LK, Goldmann BU, Ohman EM. Troponin: an important prognostic marker and risk-stratification tool in non-ST-segment elevation acute coronary syndromes. J Am Coll Cardiol. 2003;41(4 Suppl S):S31–6.
Acknowledgements
Not applicable.
Funding
This work was not funded.
Author information
Authors and Affiliations
Contributions
O.S. is the main author who responsible for: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing-original draft preparation, Writing-review & editingM.S. performed: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing-original draft preparation.B.H., N.N., C.P., J.K. responsible for: Resources, Investigation.All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by Human Ethics Committee of Thammasat University (MTU-EC-SU-1-051/66).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Satdhabudha, O., Songvasin, M., Homvises, B. et al. Can heartbeat recovery be improved with terminal non-cardioplegic warm blood perfusion prior to aortic unclamping in single-clamp technique coronary artery bypass surgery? A randomized controlled trial. J Cardiothorac Surg 19, 486 (2024). https://doi.org/10.1186/s13019-024-03006-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-03006-0