Abstract
Background
This study evaluated the prevalence and quantity of lymph nodes at particular stations of the mediastinum in patients with lung cancer. These data are important to radiologists, pathologists, and thoracic surgeons because they can serve as a benchmark when assessing the completeness of lymph node dissection. However, relevant data in the literature are scarce.
Methods
Data regarding the number of lymph nodes derived from two randomised trials of bilateral mediastinal lymph node dissection, the BML-1 and BML-2 study, were included in this analysis. Detectable nodes at particular stations of the mediastinum and the number of nodes at these stations were analysed.
Results
The mean number of removed nodes was 28.67 (range, 4–88). Detectable lymph nodes were present at stations 2R, 4R, and 7 in 93%, 98%, and 99% of patients, respectively. Nodes were rarely present at stations 9 L (33%), and 3 (35%). The largest number of nodes was observed at stations 7 and 4R (mean, 5 nodes).
Conclusion
The number of mediastinal lymph nodes in patients with lung cancer may be greater than that in healthy individuals. Lymph nodes were observed at stations 2R, 4R, and 7 in more than 90% of patients with lung cancer. The largest number of nodes was observed at stations 4R and 7. Detectable nodes were rarely observed at stations 3 and 9 L.
Trial registration
ISRCTN 86,637,908.
Similar content being viewed by others
Background
The prevalence and number of detectable nodes at particular stations of the mediastinum are important to radiologists, pathologists, and surgeons who perform mediastinal lymphadenectomy and mediastinoscopy. Unfortunately, the number of lymph nodes in patients with non-small cell lung cancer (NSCLC) has not been specifically studied, and relevant data are scarce. Most studies of the anatomy of mediastinal lymphatics have been based on investigations of groups without cancer and analysed radiological or autopsy findings rather than surgical specimens [1,2,3,4]. Bilateral mediastinal lymphadenectomy (BML) is not routinely performed for patients with lung cancer; however, it provides an opportunity to study the anatomy of mediastinal nodal compartments in surgical practice.
Materials and methods
This observational study aimed to determine the prevalence (defined as the percentage of patients with any detectable lymph nodes present in particular mediastinal stations) and quantity of lymph nodes at mediastinal stations in patients with lung cancer by evaluating data retrieved from two prospective, randomised trials, the BML-1 study [5] and the BML-2 study (ISRCTN 86,637,908), that assessed the value of BML for the surgical treatment of NSCLC. The protocols of the BML-1 and BML-2 study have been approved by the Bioethical Committee of the Jagiellonian University (K/ZDS/002337 and 1072.6120.91.2017), where the full protocol of the study is available. Both, BML-1 and BML-2 studies have been performed in accordance with the Declaration of Helsinki.
The sample size was not determined before this study was performed because of its design. The anatomy of the mediastinal lymphatics of a group of patients who underwent surgery at the Department of Thoracic Surgery, Jagiellonian University Medical College, John Paul II Hospital, Cracow, Poland, the Department of Thoracic Surgery, Sun Yat-Sen University, Guangzhou, China, and the Department of Thoracic Surgery, Cerrahpasa Medical School, Istanbul University-Cerrahpasa, Istanbul, Turkey, were evaluated. The inclusion criteria for the BML-1 study and BML-2 study were as follows: adult patients with confirmed or suspected NSCLC stages I to IIIB; preoperative staging was routinely performed using chest radiography, computed tomography, positron emission tomography-computed tomography, abdominal ultrasonography, bronchoscopy, endobronchial ultrasonography and endoscopic ultrasonography; and patients were suitable candidates for lung resection. The exclusion criteria were as follows: history of malignancies other than non-melanoma skin cancer; use of chemotherapy or chemoradiotherapy; pathological confirmation of tumours other than NSCLC; ground-glass opacity lesions; and lack of informed consent. In both studies patients were randomized in a 1:1 ratio to the group in which systematic (unilateral) lymph node dissection or BML was performed. The technique of BML is summarized below.
Bilateral mediastinal lymph node dissection was performed using both a cervical incision and thoracotomy or video-assisted thoracoscopic surgery (VATS) during one procedure. For right-sided surgery, the procedure began in a supine position with a cervical incision and exploration of stations 2 L, 4 L, and 7. Subsequently, patients were repositioned to the lateral decubitus position and – using the open or VATS approach – appropriate lung resection was performed and lymph node stations 2R, 3, 4R, 7, 8, and 9R were dissected. For left-sided surgery, the procedure began with a cervical incision and exploration of stations 2R, 2 L, 4R, 4 L, and 7. Subsequently, using the open or VATS approach, appropriate lung resection was performed and lymph node stations 5, 6, 7, 8, and 9 L were dissected. The dissection technique has been described in detail elsewhere [5]. During the procedure, the nodes from each station were labelled separately and counted by the operating surgeon to avoid their overestimation. Overestimations could occur if the number is assessed based on the pathology report because some nodes are inevitably removed in pieces. Lymph nodes were classified according to the 8th edition of the TNM staging system for lung cancer [6]. Data regarding the mediastinal lymph nodes of all patients who underwent BML during both studies were pooled for the final analysis. The prevalence of detectable lymph nodes at each mediastinal station was determined, and the node quantities are presented as the mean and range.
Results
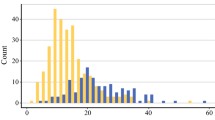
The study group comprised 181 patients who underwent bilateral mediastinal dissection. The characteristics of this group are presented in Table 1. The mean number of removed nodes was 28.67 (range, 4–88). At stations 2R, 4R, and 7, detectable lymph nodes were present in 93%, 98%, and 99% of patients, respectively. Nodes were rarely present at stations 9 L (33%), and 3 (35%). The largest number of nodes was encountered at stations 7 and 4R (mean, 5 nodes). The prevalence and number of mediastinal lymph nodes at each station are listed in Table 2 and presented in Figs. 1 and 2.
Discussion
To the best of our knowledge, this is the first study to evaluate the surgical anatomy of the mediastinal lymph nodes based on the results of bilateral mediastinal dissection performed during lung cancer surgery. These data are important to radiologists, pathologists, and thoracic surgeons because they can serve as a benchmark when assessing the completeness of lymph node dissection. Previous studies involved cadaveric and radiological studies or diagnostic explorations of the mediastinum. Beck and Beattie were the first to report data regarding the number of mediastinal lymph nodes [1]. According to their study involving five cadavers, the average number of lymph nodes was 53; however, the number of autopsies performed was limited, and the authors distinguished only four groups of mediastinal nodes (anterior mediastinum, peribronchial, subcarinal, and paratracheal nodes). Genereux and Howie reported the number of mediastinal lymph nodes without any nodal pathology observed in 39 patients using computed tomography (CT) and during dissection at the time of autopsy in 12 cadavers [2]. These authors divided the nodes into four zones: related to the innominate vein, pretracheal space, pericarinal/subcarinal space, and aortopulmonary window, and concentrated on the node size rather than on the number of nodes. Although they reported some data regarding the number of nodes found using CT (mean, 5.7 lymph nodes), they did not report any data regarding the number of nodes found during autopsy.
Two studies have reported the number of mediastinal lymph nodes classified according to the American Thoracic Society [7]. Glazer et al. reported the CT data of 56 patients and Kiyono et al. reported the data of 40 cadavers obtained during dissection at the time of autopsy [3, 4]. Individuals with any malignancy or chest inflammation were excluded from these studies. Summarised data from these two studies are presented in Table 3.
Two other studies have provided data regarding the number of lymph nodes removed during right or left thoracotomy for patients with lung cancer. Although the authors did not distinguish the nodes according to the American Thoracic Society or Mountain-Dresler classifications and used a simplified classification (superior mediastinal, inferior mediastinal, and para-aortic nodes), they reported the number of removed mediastinal lymph nodes. The numbers of nodes on the right and left sides were determined separately (21 ± 13 and 17 ± 10, respectively) [8, 9]. However, their sum should not be directly compared with the results of other authors because station 7 nodes were removed during thoracotomy on each side, and those at station 1 and station 2 L were not removed regardless of the side of the thoracotomy.
According to a retrospective study that assessed the value of transcervical extended mediastinal lymphadenectomy in lung cancer staging, 15 to 85 (mean, 38.9) lymph nodes were removed; however, station 9 was not dissected, and the number of nodes removed from particular mediastinal stations was not reported [10].
Based on these results, three issues should be addressed. First, the sensitivity of the CT-based assessments performed by Genereux and Howie and Glazer et al. [2, 3] was dependent on the CT scanner generation used in 1980s and slice thickness; the risk of missing small nodes is substantial with thick slices. Second, the numbers of detectable mediastinal nodes in individuals without chest inflammation or malignancy may differ from those of patients with NSCLC. The aforementioned studies included populations without malignancy or chest inflammation [3, 4]; it should be emphasized that the numbers of lymph nodes reported by those studies were approximately two-fold less than those reported by other studies involving patients with lung cancer and our team [8, 9]. Third, the simplified classifications used in these studies do not correspond to the present 8th edition of the TNM system.
Additionally, the distribution of nodes differed. For individuals without chest pathology, the largest number of nodes was encountered in both the left paratracheal (stations 2 L and 4 L) and preaortic regions (station 6), and relatively fewer nodes were encountered in the subcarinal region (station 7), suggesting that changes in the mediastinal lymphatic system of patients with lung cancer may lead to inadequate results of anatomical studies in clinical settings. However, the nodal stations with the largest and smallest prevalence of lymph nodes did not differ between patients with lung cancer and healthy individuals.
The strengths of our study include its multicentre design, large number of analysed patients and use of data from real-world surgical practice. Therefore, the applicability of these results to clinical practice may be better than that of the results of purely anatomical studies. Data we present may be used as a reference point for assessment of completeness of lymph node dissection during lung cancer surgery. Also, we used the current TNM classification, instead the simplified divisions used in previously published papers [1, 2, 4, 8]. Stations 5 and 6 were not dissected during right-sided surgery, which was the main limitation of this study. However, because metastases from right lung tumours to these two stations are very rare, the clinical importance of this limitation seems negligible.
Conclusions
Patients with lung cancer may have more detectable mediastinal lymph nodes than healthy individuals. Lymph nodes were most often observed at stations 2R, 4R, and 7 in patients with lung cancer. The largest number of nodes was observed at stations 4R and 7, while detectable nodes were least often observed at stations 3 and 9 L.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Beck E, Beattie EJ. The lymph nodes in the mediastinum. J Int Coll Surg. 1958;29:247–51.
Genereux GP, Howie JL. Normal mediastinal lymph node size and number: CT and anatomic study. AJR Am J Roentgenol. 1984;142:1095–100.
Glazer GM, Gross BH, Quint LE, Francis IR, Bookstein FL, Orringer MB. Normal mediastinal lymph nodes: number and size according to American thoracic society mapping. AJR Am J Roentgenol. 1985;144:261–5.
Kiyono K, Sone S, Sakai F, et al. The number and size of normal mediastinal lymph nodes: a postmortem study. AJR Am J Roentgenol. 1988;150:771–6.
Kużdżał J, Trybalski Ł, Hauer Ł, et al. Influence of bilateral mediastinal lymph node dissection on survival in non-small cell lung cancer patients – randomized study. Lung Cancer. 2021;156:140–6.
Asamura H, Chansky K, Crowley J et al. International Association for the Study of Lung Cancer staging and prognostic factors committee, advisory board members, and participating institutions. The International Association for the Study of Lung Cancer lung cancer staging project: proposals for the revision of the N descriptors in the forthcoming, 8th edn. of the TNM Classification for Lung Cancer. J Thorac Oncol. 2015;10:1675-84.
The American Thoracic Society. Medical section of the American Lung Association. Clinical staging of primary lung cancer. Am Rev Respir Dis. 1983;127:659–64.
Sagawa M, Sato M, Sakurada A, Matsumura Y, Endo C, Handa M, Kondo T. A prospective trial of systematic nodal dissection for lung cancer by video-assisted thoracic surgery: can it be perfect? Ann Thorac Surg. 2002;73:900–4.
Watanabe A, Koyanagi T, Obama T, Ohsawa H, Mawatari T, Takahashi N, Ichimiya Y, Abe T. Assessment of node dissection for clinical stage I primary lung cancer by VATS. Eur J Cardiothorac Surg. 2005;27:745–52.
Zieliński M. Transcervical extended mediastinal lymphadenectomy: results of staging in two hundred fifty-six patients with non-small cell lung cancer. J Thorac Oncol. 2007;2:370–2.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
Ł Trybalski: project development, data collection, data analysis, manuscript writing; J Szadurski: project development, data collection, data analysis, manuscript editing; L Zhang: data collection, manuscript editing; J Kużdżał: project development, data analysis, manuscript writing; A Turna: data collection, manuscript editing; W Wang: data collection, manuscript editing; J Warmus: data collection, manuscript editing; G Ozcibik Isık: data collection, manuscript editing; K Żanowska: data collection, manuscript editing; P Kocoń: project development, data analysis, manuscript writing.
Corresponding author
Ethics declarations
Ethical approval
The protocols of the BML-1 and BML-2 study have been approved by the Bioethical Committee of the Jagiellonian University (K/ZDS/002337 and 1072.6120.91.2017), where the full protocol of the study is available. Both, BML-1 and BML-2 studies have been performed in accordance with the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all patients in the BML-1 and BML-2 study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Trybalski, Ł., Szadurski, J., Zhang, L. et al. Prevalence and quantity of lymph nodes at mediastinal stations in patients with lung cancer: lessons from 181 bilateral mediastinal lymphadenectomies. J Cardiothorac Surg 19, 412 (2024). https://doi.org/10.1186/s13019-024-02928-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02928-z