Abstract
Objective
To investigate the clinical significance of the creatine kinase (CK)-MB/total CK ratio, neutrophil/lymphocyte ratio (NLR) and red blood cell distribution width in acute myocardial infarction (AMI).
Methods
A retrospective analysis was conducted of 196 AMI cases from our hospital’s cardiology department; healthy people were selected over the same period as the control. The two groups’ test indexes were compared through multivariate logistic regression analysis to screen for AMI risk factors; the receiver operating characteristic (ROC) curve was used to evaluate their AMI predictive values.
Results
The serum CK, CK-MB, CK index, neutrophils and NLR values in the AMI group were significantly higher compared with those in the control group (p < 0.05); however, the levels of serum lymphocytes were significantly lower compared with those in the control group (p < 0.05). Multivariate logistic regression analysis showed that elevated CK-MB and NLR levels were risk factors for AMI (p < 0.05). The ROC curve showed that the area under the curve of the NLR and CK levels were 0.917 and 0.594, respectively.
Conclusion
The CK index and NLR have a clinical predicting value for AMI and could be used as a clinical auxiliary diagnostic index for the assessment of patients with AMI.
Similar content being viewed by others
Introduction
Acute myocardial infarction (AMI) is a severe type of ischemic heart disease. Globally, approximately 9 and 182 million deaths and disabilities, respectively, were caused by AMI in 2019 [1,2,3]. Creatine kinase-MB (CK-MB) is a clinically recognised biomarker for detecting myocardial injury. It is mainly present in myocardial tissue; when myocardial cells experience ischemia or necrosis, CK-MB is released into the blood, resulting in an elevated CK-MB index in the serum. Inflammation plays an important role in the occurrence and progression of AMI and the neutrophil (NEUT)/lymphocyte (LYM) ratio (NLR) is a marker of the body’s inflammatory state. The NLR is a simple and low-cost measure that is associated with the development and prognosis of various diseases [4,5,6]. Therefore, this study aimed to explore the diagnostic value of the CK index and NLR in patients with AMI and further investigate their predictive values for disease progression.
Materials and methods
Study participants
The calculated sample size was at least 190 cases based on the following sample size calculation formula for case-control studies:
where Z is the confidence interval, N is the sample size, d is the sampling error range and σ is the standard deviation (usually taken as 0.5). Therefore, a total of 196 patients with AMI (110 men and 86 women, aged 33–91, average = 75.2 ± 12.4 years) diagnosed in our hospital between December 2019 and July 2022 were selected via random sampling as the AMI group. All selected patients met the diagnostic criteria for AMI released by the Chinese Society of Cardiology. Additionally, 144 healthy individuals (83 men and 61 women, aged 35–89, average = 69.3 ± 11.9 years) who underwent physical examinations during the same period were selected as the control group.
The exclusion criteria were as follows: patients with (1) severe cardiovascular and cerebrovascular diseases of other types; (2) severe liver and kidney dysfunction or undergoing haemodialysis; (3) recent major surgery or serious traumatic history; and (4) severe immune system diseases or recent use of immunosuppressants, malignant tumours or undergoing radiotherapy or chemotherapy, among others.
Outliers in the data were identified and removed using the interquartile range (IQR) method. The IQR is the difference between the 75th and 25th percentiles of the data. Any value that is more than 1.5 times the IQR above the 75th percentile or below the 25th percentile is considered an outlier. This resulted in the exclusion of 12 cases from the original sample of 196 cases.
Methods
General clinical data of the patients were collected; the primary output variables were CK-MB/CK ratio and NLR. Peripheral fasting venous blood samples were collected using vacuum tubes containing dipotassium-ethylene diamine tetra-acetic acid and heparin as anticoagulants. After blood collection, the anticoagulant tubes were gently mixed to prevent clot formation and bubble generation. The CK and CK-MB levels were measured using a Hitachi 7600 fully automatic biochemical analyser, and the CK index (CK index = CK-MB/CK) was calculated [7]. The SYSMEX IE2100 fully automatic blood cell analyser was used to measure the white blood cells, NEUT, LYM counts, etc., and the NLR was calculated (NLR = NEUT/LYM). Original matching reagents were used, with internal quality evaluations performed using these before blood sample testing was conducted.
The diagnosis of acute myocardial infarction
Identifying patients with AMI involves a combination of clinical assessment, diagnostic tests and medical history. Patients with AMI often present with typical symptoms, such as chest pain or discomfort, which may radiate to the arm, neck, jaw, shoulder or back. Other symptoms can include shortness of breath, nausea, light-headedness and sweating. In addition, electrocardiography is a crucial diagnostic tool for identifying AMI in patients; it can show characteristic changes, such as ST-segment elevation or ST-segment depression. Furthermore, coronary angiography can be performed in cases where revascularisation procedures, such as percutaneous coronary intervention or coronary artery bypass grafting, are considered, as it provides direct visualisation of coronary artery blockages.
Data analysis
Data analyses were performed using SPSS v.22.0 (IBM Statistical Software™, IBM Corp., Armonk, NY, USA). The hypothesis testing was as follows:
-
Null hypothesis (H0): There is no significant association between CK-MB/CK, NLR and red blood cell distribution width and the occurrence of AMI in the studied population.
-
Alternative hypothesis (H1): There is a significant association between CK-MB/CK, NLR and red blood cell distribution width and the occurrence of AMI in the studied population.
Data pre-processing mainly included identifying and handling missing data by mean/median imputation, either removing the corresponding records or filling in the missing values. In addition, outliers that may have distorted the analysis were identified. Inconsistencies or errors in the data were corrected and the numerical features were standardised or normalised to ensure they had a similar scale. Statistical methods, such as the interquartile range or z-score, were employed to identify values that fell significantly outside the expected range.
Statistical analysis
Statistical analyses were performed using SPSS v.22.0 (SPSS, Inc., Chicago, IL, USA). All measurement data were tested for normality using the Kolmogorov–Smirnov test and presented as the mean ± standard deviation (x̅ ± s). Independent sample t-tests were used for comparing data between groups. Multivariate logistic regression analysis was used to identify risk factors for AMI occurrence based on the differences between the groups using model relationships between variables. Receiver operating characteristic (ROC) curve analysis was employed to evaluate the predictive performance. A significance level of p < 0.05 denoted statistical significance.
Results
Comparison of the serum level results between the groups
As Table 1 shows, the serum levels of CK, CK-MB, CK index, NEUT and NLR in the AMI group were significantly higher compared with those in the control group (p < 0.05). However, the LYM serum levels were significantly lower in patients with AMI compared with the levels in the control group (p < 0.05).
Multivariable logistic regression analysis of the factors influencing the occurrence of acute myocardial infarction
The multivariate logistic regression analysis of CK, CK-MB, CK index, LYM, NEUT and NLR revealed that elevated CK-MB and NLR were independent risk factors for AMI occurrence (Table 2).
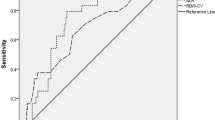
The receiver operating characteristic curve analysis of the CK index and NLR for predicting acute myocardial infarction
The ROC curve analysis showed that NLR’s area under the curve (AUC) for predicting AMI was 0.917 (95% CI: 0.888–0.947, p < 0.001), with a sensitivity of 83.7% and specificity of 81.2%. The AUC for the CK index was 0.594 (95% CI: 0.534–0.654, p = 0.003), with a sensitivity of 60.2% and specificity of 54.9% (Fig. 1).
Discussion
Acute myocardial infarction is a common cardiovascular emergency disease caused by acute obstruction of the coronary artery leading to local myocardial ischemic necrosis. Inflammation and oxidative stress are related to its pathogenesis, with atherosclerosis being the pathological basis for the development of the disease. Therefore, the role of inflammatory biomarkers in the occurrence of AMI has received extensive attention from local and international scholars [8,9,10]. The NLR is an inflammatory marker that combines two subtypes of white blood cells, the NEUTs and LYMs, and has been demonstrated to be associated with the occurrence and prognosis of cardiovascular and cerebrovascular diseases [11,12,13].
Neutrophils can aggravate endothelial cell injury and the damaged endothelial cells can induce NEUT adhesion and aggregation through the expression of selectins and chemokines. The interaction between the NEUTs and the basement membrane increases the permeability of the endothelium [14], facilitating the aggregation of monocytes/macrophages, promoting the transformation of macrophages into foam cells, and forming plaques [15]. When atherosclerosis affects the smooth muscle cell layer of the media, activated smooth muscle cells attract the NEUTs to promote plaque rupture and thrombus formation [16].
Lymphocytes are important cells involved in specific immunity and have a regulatory role in inflammatory responses, protecting arterial vessels by inhibiting inflammatory responses during the occurrence and development of atherosclerosis [17]. In this study, the NLR in patients with AMI was significantly higher compared with the control group (p < 0.05). In addition, multivariate logistic regression analysis showed that NLR elevation was a factor influencing the occurrence of AMI in patients (p < 0.05). The ROC curve analysis revealed an AUC of 0.917 for the NLR predicting AMI, with a sensitivity and specificity of 83.7% and 81.2%, respectively. These findings suggest that NLR elevation is associated with the occurrence of AMI.
Creatine kinase mainly exists in the myocardium and skeletal muscles of the human body, including three types of isoenzymes: muscle-type (CK-MM), brain-type (CK-BB) and heart-type (CK-MB), which mainly exists in the myocardium and is a sensitive indicator for early detection of myocardial injury in clinical practice. In addition, the CK-MB level is often used in conjunction with electrocardiography for the clinical diagnosis of patients with chest pain [18]. However, as the understanding of different systemic diseases deepens, it has been found that malignancies, severe liver diseases, skeletal muscle loss, severe trauma, and other conditions may cause a false elevation of CK-MB. In clinical practice, a CK-MB value exceeding twice the upper limit of normal is often indicative of a higher possibility of acute myocardial injury, but this empirical criterion may lead to clinical misdiagnosis. Subsequently, some scholars have proposed that using CK-MB/CK as an index for the diagnosis and differential diagnosis of myocardial injury has advantages over CK-MB alone [19, 20]. In this study, the CK index in patients with AMI was significantly higher compared with the control group (p < 0.05). The ROC curve analysis revealed an AUC of 0.594 for the CK index, with a sensitivity of 60.2% and a specificity of 54.9%; this suggests that CK-MB/CK has a moderate diagnostic efficacy.
In conclusion, the CK index and NLR have a predictive value for the diagnosis of AMI, with the NLR being superior to the CK index. However, due to the small sample size of this study, the results may be biased, limiting its clinical application. Therefore, further validation is needed through larger-scale clinical studies.
Data availability
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Abbreviations
- WBC:
-
White blood cells
- NEUT:
-
Neutrophils
- LYU:
-
Lymphocyte
- AMI:
-
Acute myocardial infarction
- CK-MB:
-
Creatine kinase-MB
- NLR:
-
Neutrophils to lymphocytes ratio
- ROC:
-
Receiver operating characteristic curve
References
Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021.
Song Y, Jing Ling. Research progress on predicting factors for heart failure after acute myocardial infarction. Chin J Evidence-Based Cardiovasc Med. 2021;13(10):1270–2.
Leithead JA, Rajoriya N, Gunson BK, et al. Neutrophil-to-lymphocyte ratio predicts mortality in patients listed for liver transplantation. Liver Int. 2015;35(2):502–9.
Atum M, Alagöz G. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with retinal artery occlusion. J Ophthalmic Vis Res. 2020;15(2):195–200.
Li L, Zhang H, Feng GL. Neutrophil-to-lymphocyte ratio predicts in-hospital mortality in Intracerebral Hemorrhage. J Stroke Cerebrovasc Dis. 2022;31(8):106611.
Xie Yuying M, Xuesong L, Xingtong, et al. Influence of creatine kinase index on the risk of recurrence in patients with acute ischemic stroke. Chin J Crit Care Med. 2021;41(08):714–7.
Di Lorenzo B, Pau MC, Zinellu E, et al. Association between Red Blood cell distribution width and obstructive sleep apnea syndrome: a systematic review and Meta-analysis. J Clin Med. 2023;12(9):3302.
Kose N, Akin F, Yildirim T, et al. The association between the lymphocyte-to-monocyte ratio and coronary artery disease severity in patients with stable coronary artery disease. Eur Rev Med Pharmacol Sci. 2019;23(6):2570–5.
Xu Na T, Xiaofang X, Jingjing, et al. Predictive value of neutrophil-to-lymphocyte ratio on long-term prognosis in patients with acute myocardial infarction and multi-vessel disease. Chin J Cardiol. 2019;47(1):42–8.
Wang Y. Predictive value of neutrophil-to-lymphocyte for first acute myocardial infarction in patients with type 2 diabetes mellitus. J Nanchang Univ (Medical Edition). 2021;62(5):45–50.
Bo Y, Shengmin T, Jialin N, et al. Evaluation of neutrophil-to-lymphocyte ratio for coronary artery disease severity and prognosis in elderly patients with acute ST-segment elevation myocardial infarction. Chin J Geriatric Heart Brain Vessel Dis. 2022;24(4):385–8.
Chen Y, Chen S, Han Y, et al. A combined index constructed based on NLR and PLR is associated with in-hospital mortality risk in patients with acute myocardial infarction. Am J Transl Res. 2023;15(6):4118–28.
Khire TS, Salminen AT, Swamy H, et al. Microvascular mimetics for the study of leukocyte-endothelial interactions. Cell Mol Bioeng. 2020;13(2):125–39.
Shibata K, Sato K, Shirai R, et al. Lipocalin-2 exerts pro-atherosclerotic effects as evidenced by in vitro and in vivo experiments. Heart Vessels. 2020;35(7):1012–24.
Silvestre-Roig C, Braster Q, Wichapong K, et al. Externalized histone H4 orchestrates chronic inflammation by inducing lytic cell death. Nature. 2019;569(7755):236–20.
Chen Z, Yan W, Mao Y, et al. Effect ofAerobic Exercise on Treg and Th17 of rats with ischemic cardiomyopathy. J Cardiovasc Transl Res. 2018;11(3):230–5.
Fan J, Ma J, Xia N, et al. Clinical value of combined detection of CK-MB, MYO, cTnI and plasma NT-proBNP in diagnosis of Acute myocardial infarction. Clin Lab. 2017;63(3):427–33.
Wei Zhonghai. Discussion on the clinical application value of the ratio of phosphocreatine kinase and its isoenzyme in the differential diagnosis of myocardial injury. Zhejiang: Zhejiang University; 2008.
Rigueira J, Aguiar-Ricardo I, Carrilho-Ferreira P, et al. Predictors of coronary artery disease in cardiac arrest survivors: coronary angiography for everyone? A single-center retrospective analysis. Rev Bras Ter Intensiva. 2021;33(2):251–60.
Acknowledgements
None.
Funding
This study did not receive any funding in any form.
Author information
Authors and Affiliations
Contributions
Liu Y and Tang XL conceived of the study, and Ni Y, Duan LZ and Jing FJ participated in its design and data analysis and statistics and Liu Y helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of The Second Affiliated Hospital of Wannan Medical College.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Tang, XL., Ni, Y. et al. Diagnostic value of the creatine kinase-MB/creatine kinase and neutrophil/lymphocyte ratios in acute myocardial infarction. J Cardiothorac Surg 19, 227 (2024). https://doi.org/10.1186/s13019-024-02740-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02740-9