Abstract
Background
Open repair of thoracoabdominal aortic aneurysm (TAAA) was characterized by significant risk of postoperative mortality and morbidity. The aim of this study was to determine the perioperative predictors of early and long-term mortality in patients undergoing open repair of TAAA. Besides, the postoperative outcomes in patients with open repair of TAAA were described.
Methods
This is a single-center retrospective study, and 146 patients with open repair of TAAA from January 4, 2011, to November 22, 2018 was involved. Categorical variables were analyzed by the Chi-square test or Fisher’s exact test, and continuous variables were analyzed by the independent sample t-test and the WilCoxon rank-sum test. Multivariate Logistic regression and Cox regression were applied to identify the predictors of 30-day and long-term mortality, respectively. The Kaplan Meier curves were used to illustrate survival with the Log-rank test.
Results
The 30-day mortality was 9.59% (n = 14). Older than 50 years, the intraoperative volume of red blood cell (RBC) and epinephrine use were independently associated with postoperative 30-day mortality in open repair of TAAA. Long-term mortality was 17.12% (n = 25) (median of 3.5 years (IQR = 2–5 years) of follow-up). Prior open thoracoabdominal aortic aneurysm (TAAA) repair, aortic cross-clamping (ACC) time, intraoperative volume of RBC and use of epinephrine were independently correlated with long-term mortality.
Conclusions
Identifying perioperative risk factors of early and long-term mortaliy is crucial for surgeons. Intraoperative volume of RBC and use of epinephrine were predictors of both early and long-term mortality. In addition, patients of advanced age, prior open repair of TAAA and prolonged ACC time should be paid more attention.
Similar content being viewed by others
Background
The natural progression of thoracoabdominal aortic aneurysm (TAAA) can lead to the aneurysm growing, and finally the aneurysm is prone to rupture without surgery. The prognosis of such patients with TAAA is poor [1, 2]. It is reported that the 5-year survival rate of such patients without surgery is from 7% to19.2% [3]. Currently, the main surgery of TAAA is open repair of thoracoabdominal aortic aneurysm (TAAAR), which can effectively prevent aneurysm rupture. Recently, a systematic review illustrated that the perioperative mortality of 47 studies related to open TAAAR is 8.9% [4]. However, many studies reported that the incidence of mortality and severe complications including permanent spinal cord injury (SCI), renal failure, stroke, myocardial infarction after the TAAAR cannot be ignored [5,6,7], especially in extent II and III [8]. This research mainly analyses perioperative risk factors of 30-day and long-term mortality in open repair of thoracoabdominal aortic aneurysm (TAAA, extent II/III).
Methods
This is a single-center retrospective study including 146 consecutive patients who underwent open repair of TAAA from January 4, 2011, to November 22, 2018. Ethical consent was approved by the Ethics Committee of Fuwai Hospital (Approval NO. 2019 − 1308). The study protocol was compliant with the Declaration of Helsinki. Patient consent was waived.
Data resource
Patients’ data was collected from electronic medical record system. Clinical data included preoperative basic characteristics, intraoperative variables, postoperative 30-day mortality and adverse complications. In addition to collecting furthermore data, the occurrence and time of mortality and adverse outcomes were followed by our research staff by telephoning patients and patients’ family members in 2020.
Surgical methods
Under general anesthesia and normothermic conditions with a nasal temperature > 35 °C, a left lateral thoracoabdominal incision was made, involving rib dissection, extending through the left rectus abdominis to the level of the umbilicus. During the procedure, moderate doses of heparin (200 U/kg) was used. The thoracic and abdominal aorta were exposed, and the proximal thoracic aorta was mobilized. A quadrifurcated graft was used to replace the descending aortic aneurysm. One branch of the graft was anastomosed to the severed end of the left external iliac artery, while another branch was connected to a vein for blood return using a blood pump technique. Temporary cross-clamping was applied to thoracic aorta, and proximal end of the synthetic graft was was anastomosed to the severed end of the thoracic aorta and reconstruction of intercostal arteries was performed. The celiac trunk, superior mesenteric artery, and right renal artery were modified into an island configuration, anastomosed to the distant proximal end of the synthetic graft. The left renal artery and bilateral common iliac arteries were anastomosed to branch synthetic grafts. Finally, protamine sulfate was utilized to neutralize heparin. For cases where occlusion of the proximal end of the thoracic aorta was not feasible, surgery was performed under deep hypothermic circulatory arrest (DHCA).
TAAA repair with DHCA involved the administration of heparin (400 U/kg). Initiation of hypothermic circulatory arrest was followed by establishing vena cava drainage through cannulation of the left external iliac vein. Insertion of an arterial cannula into the left external iliac artery facilitated drainage from the left heart, achieved by inserting a tube either into the apical incision or the main pulmonary artery to establish cardiopulmonary bypass. Nasal and rectal temperatures were gradually reduced to 20 °C.
Definitions
Regarding postoperative complications, hypohepatia was identified as alanine aminotransferase (ALT) > 200 u/L or total bilirubin (TBil) > 50 umol/L or lactic dehydrogenase (LDH) > 500 u/L. Postoperative renal failure was defined as the need for dialysis or hemofiltration as well as renal insufficiency was defined as the serum creatinine level two times than the preoperative baseline value [9]. Postoperative respiratory complications were defined as one or more episodes of postoperative pneumonia, respiratory failure, acute respiratory distress syndrome (ARDS), or pulmonary embolism. SCI was classified, according to its severity, into paraplegia (muscle strength 0 ∼ 2 grade) and paraparesis (muscle strength 3 ∼ 4 grade). In order to provide more guidance for clinical practice, the age was divided into two categories by interquartile range (IQR): 50 (17–70) years. The cut-off point of body mass index (BMI) was 30 kg/m2 on account of the World Health Organization’s BMI diagnosis of obesity [10].
Outcomes of interest
The primary endpoint was 30-day and long-term mortality. Secondary endpoint was a composite endpoint which included 30-day and long-term adverse outcomes.
Statistical analysis
Data were analyzed with IBM SPSS Statistics 26.0. Discrete variables and continuous variables were presented as n (%) and mean ± standard deviation, respectively. We tried to find out influencing factors for the mortality in the short term after surgery. Categorical variables were analyzed by using the Chi-square test or Fisher’s exact test. The independent sample t-test and the WilCoxon rank-sum test were used for normally and non-normally distributed continuous variables, respectively. Univariate Logistic regression was performed between groups with and without death within 30 days to select risk factors from all relevant preoperative and intraoperative variables, and each variables showing P < 0.05 were entered into multivariate Logistic regression models (method: LR forward) to identify independent risk factors.
Simultaneously, the multivariate Cox regression (method: LR forward) was performed to identify independent risk factors of long-term mortality. For the independent risk factors identifified by Cox regression, the actuarial survival was shown by the Kaplan Meier analysis and differences between the two groups was determined by the Log-rank test. Discrete variables were transformed into categorical variables according to their quartiles as a cut point. P value less than 0.05 was considered significant.
Results
Of 146 patients undergoing open repair of TAAA, 101 cases were Crawford extent II and 45 cases were Crawford extent III. The average age of study participants was 41.27 ± 11.61 years. The proportion of males (76.03%) was greater. The mean ACC time was 22.29 ± 24.04 min. Preoperative and intraoperative patients characteristics were listed in Table 1.
Mortality
Short-term mortality
The 30-day mortality was 9.59% (n = 14). Aged ≥ 50 years had a 14.732 (95%CI: 2.218–97.836) odds ratio of mortality as compared with < 50 years. The intraoperative volume of RBC was an independent risk factor for mortality, with odds ratio 1.262 (95%CI: 1.130–1.410). Intraoperative use of epinephrine had a 11.148 (95%CI: 1.738–71.525) odds of 30-day mortality as compared to without epinephrine (Table 2).
Long-term mortality
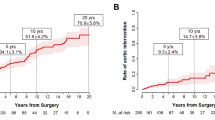
The rate of follow-up was 85.62% (n = 125) and 14.38% (n = 21) was loss to follow-up due to changing contact information. Overall mortality was 17.12% (n = 25) at a median follow-up duration of 3.5 years (IQR = 2–5 years). Variables were further divided according to mortality status within 9 years between the two groups (Table 1). Patients with prior open TAAA repair had a 12.930 (95%CI: 2.722–61.427) hazard ratio of mortality as compared with those without (Table 3). Besides, the ACC time and intraoperative volume of RBC were independent risk factors for long-term mortality, with hazard ratio 1.016 (95%CI: 1.003–1.028) and 1.097 (95%CI: 1.004–1.152), respectively. Simultaneously, intraoperative use of epinephrine mortality had approximately four times hazard of mortality compared to without use of epinephrine. The Kaplan–Meier curves of the four independent risk factors evaluated by the Log-rank test are shown in Fig. 1. The cut points of ACC time is 23 min (IQR = 10–23 min, median = 17 min) and of intraoperative volume of RBC is 6 units (IQR = 0–6 units, median = 2 units).
Adverse outcomes
Short-term outcomes
The postoperative 30-day outcomes were presented in Table 4. Regarding to adverse complication, patients with stroke were 2.05% (n = 3), 13.70% (n = 20) patients suffered spinal cord injury, and patients suffering from respiratory complications, renal insufficiency and renal failure were 17.12% (n = 25), 18.49% (n = 27) and 19.18% (n = 28), respectively. In addition, intensive care unit (ICU) length of stay was 7.014 ± 8.674 days.
Long-term outcomes
The postoperative long-term outcomes were listed in Table 5. At a 9-year follow-up, the overall incidence of stroke, permanent spinal cord injury, myocardial infarction (MI), renal failure, sexual dysfunction and permanent hoarseness was 5.48% (n = 8), 13.01% (n = 19), 3.42% (n = 5), 21.23% (n = 31), 2.74% (n = 4) and 1.37% (n = 2), respectively.
Discussion
This study identified independent perioperative risk factors for both early and long term mortality after TAAA.
The 30-day mortality of 9.59% was higher than other research, as compared to 7–9% [4, 11,12,13]. However, this study only included extent II and extent III, and previous studies have shown that patients in extent II and III had increased rates of mortality (9.1–9.5% and 8.8%-12.7% respectively) and adverse outcomes [5, 9]. Three independent risk factors (aged ≥ 50 yeas, intraoperative volume of RBC, and intraoperative use of epinephrine) were associated with an increased risk for 30-day mortality. The incidence of mortality was increased obviously in the advanced aged population, which was also supported by previous studies from Anand Dayama et al. [14] and Joseph S. Coselli et al. [5] In this study we found that the intraoperative volume of RBC transfusion for patients with and without 30-day mortality are 14.79 ± 9.58 and 3.26 ± 4.40 units respectively. Increased intraoperative volume of RBC was an independent risk factor of 30-day mortality. Recent evaluations suggest that in the majority of clinical settings, restrictive RBC transfusion strategies are safe compared with liberal strategies which might potentially lead to adverse outcomes [15,16,17]. In 2009, M D Kertai et al. found that 30-day mortality of TAAA surgery was increased in patients receiving intraoperative RBC compared to those without (1 or 2 units of RBCs) [13]. Intraoperative use of RBC in patients with open repair of aortic aneurysm was independently related with perioperative mortality [13], which was also consistent with our study. According to the results presented above, it is advisable to consider more restrictive strategies concerning RBC transfusions for patients undergoing elective TAAA repair. Administering RBC transfusions at a conservative hemoglobin level of 7–8 g/dL might be considered viable without concerning about potential adverse effects [16]. Epinephrine is crucial for increasing cerebral and coronary perfusion pressure during circulatory instability [18]. In our research, out of 10 patients (6.85%) were applied 7258 ± 14,515 µg epinephrine, 6 (4.11%) of them who were received 11,408 ± 18,091 µg epinephrine experienced mortality within 30 days. The mortality and severe complications after TAAA repair are associated with hypoperfusion [19, 20].
Long-term survival rate was 82.88% (median of 3.5 years of follow-up). Multivariate Cox regression analysis showed four independent risk factors (prior open repair of aortic aneurysm, ACC time, increased intraoperative volume of RBC, intraoperative use of epinephrine) associated with an increased risk for long-term mortality. In this study we knew that the intraoperative volume of RBC transfusion for patients with and without Long-term death are 9.16 ± 9.69 and 3.37 ± 4.53 units respectively. Increased intraoperative volume of RBC and intraoperative use of epinephrine were independent risk factors for both early and long term mortality. In previous study, The transfusion of 4 or more units of RBC correlated with heightened mortality, and this elevated risk was maintained during the 15-year follow-up period [15]. In this research, 7 (4.79%) patients who were received 9850 ± 17,021 µg epinephrine experienced long-term mortality. Christopher J. R et al. research showed that epinephrine may lead to worse microcirculatory flow, and was associated with worse long-term outcomes [18]. Joseph V et al. presented that there was no significant association between prior TAAA repair and mortality of reoperative TAAA surgery [21]. However, we found that prior open TAAA repair was an independent risk factor for long-term mortality. In this study, the number of patients with prior TAAA repair (2.05%, n = 3) are fewer, compared with 7% (n = 20) [21], and the result may require a larger sample size to support. Furthermore, several previous studies [9, 12, 22], illustrated that increased ACC time was a risk factor for long-term mortality and adverse events. In our research, the intraoperative ACC time for patients with and without Long-term death are 34.88 ± 32.75 min and 19.69 ± 21.07 min respectively. An extensive ACC duration is characterized as significant when exceeding 30 min for TAAA surgery [22].
SCI is one of the serious complications after TAAAR, which can result in paraplegia and paraparesis [5, 9]. In this study, the incidence of immediate postoperative SCI is 13.70% (n = 20), with 8.90% of paraplegia and 4.79% of paraparesis. Seven cases were cured before discharge under active treatments. 6 cases were delayed SCI (SCI occurred after discharge from the hospital). The incidence of permanent SCI is 13.01% (n = 19). Surprisingly, in the process of follow-up, we found that four cases occurred sexual dysfunction after the surgery. In male, sexual dysfunction can result from erectile dysfunction (ED), which is caused by the inability to achieve or maintain an erection or ejaculation disorders [23, 24]. Previous clinical study showed that abdominal aortic aneurysm (AAA) surgical repair has an impact on sexual function which is caused by the involvement of the common iliac artery by AAA repair [23]. However, up to now, studies of sexual dysfunction after TAAAR are rare. TAAAR also involves the common iliac artery, so the occurrence of sexual function after such procedure requires more attention. Two patients happened permanent hoarseness after the surgery, and this outcome was generally associated with prolonged tracheal intubation [25,26,27].
Several approaches have been devised and are applied in surgery to minimize spinal cord injury, enhance spinal cord metabolism, and reduce ischemia in distal organs. These encompass profound hypothermic circulation arrest, intraoperative distal aortic perfusion, left heart bypass, monitoring spinal motor neurons through motor evoked potentials, cerebrospinal fluid drainage, and facilitating intraoperative spinal cord perfusion to reduce ischemia-reperfusion damage.
The primary limitation of current study is that the number of cases involved is small due to the difficulty of therapy and expensive cost. Moreover, this is a single-center study which is appropriate for Asian populations and the applicability in other populations require further researches to verify.
Conclusion
Our study identified perioperative predictors for early and long term mortality after TAAA. This result could be instructive for perioperative patient management. In addition, the early and long term postoperative outcomes were presented. Although open repair of thoracoabdominal aortic aneurysm was the primary treatment method for patient at risk for lethal aneurysm rupture, the challenging mortality and adverse outcomes cannot be ignored.
Data availability
Data supporting the results reported in the article can be accessed by connecting wangyuefu@hotmail.com.
Abbreviations
- TAAA:
-
Thoracoabdominal aortic aneurysm
- RBC:
-
Red blood cell
- ACC:
-
aortic cross-clamping
- TAAAR:
-
Repair of thoracoabdominal aortic aneurysm
- SCI:
-
spinal cord injury
- DHCA:
-
deep hypothermic circulatory arrest
- ALT:
-
Alanine aminotransferase
- TBil:
-
Total bilirubin
- LDH:
-
Lactic dehydrogenase
- ARDS:
-
Acute respiratory distress syndrome
- IQR:
-
Interquartile range
- BMI:
-
Body mass index
- ICU:
-
Intensive care unit
- MI:
-
Myocardial infarction
- ED:
-
Erectile dysfunction
- AAA:
-
Abdominal aortic aneurysm
References
Crawford ES, DeNatale RW. Thoracoabdominal aortic aneurysm: observations regarding the natural course of the disease. J Vasc Surg. 1986;3(4):578–82.
Matsushita A, Fukui T, Tabata M, et al. Preoperative characteristics and surgical outcomes of acute intramural hematoma involving the ascending aorta: a propensity score-matched analysis. J Thorac Cardiovasc Surg. 2016;151(2):351–8.
Bickerstaff LK, Pairolero PC, Hollier LH, et al. Thoracic aortic aneurysms: a population-based study. Surgery. 1982;92(6):1103–8.
Rocha RV, Lindsay TF, Friedrich JO, et al. Systematic review of contemporary outcomes of endovascular and open thoracoabdominal aortic aneurysm repair. J Vasc Surg. 2020;71(4):1396–412.
Coselli JS, LeMaire SA, Preventza O, et al. Outcomes of 3309 thoracoabdominal aortic aneurysm repairs. J Thorac Cardiovasc Surg. 2016;151(5):1323–38.
Parotto M, Ouzounian M, Djaiani G. Spinal cord Protection in Elective Thoracoabdominal aortic procedures. J Cardiothorac Vasc Anesth. 2019;33(1):200–8.
Schepens MA, Heijmen RH, Ranschaert W, et al. Thoracoabdominal aortic aneurysm repair: results of Conventional Open surgery. Eur J Vasc Endovasc Surg. 2009;37(6):640–5.
Arnaoutakis DJ, Scali ST, Beck AW, et al. Comparative outcomes of open, hybrid, and fenestrated branched endovascular repair of extent II and III thoracoabdominal aortic aneurysms. J Vasc Surg. 2020;71(5):1503–14.
LeMaire SA, Price MD, Green SY, et al. Results of open thoracoabdominal aortic aneurysm repair. Ann Cardiothorac Surg. 2012;1(3):286–92.
Barba C, Cavalli-Sforza T, Cutter J, et al. WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Conrad MF, Crawford RS, Davison JK, et al. Thoracoabdominal aneurysm repair: a 20-Year perspective. Ann Thorac Surg. 2007;83(2):S856–861.
Wong DR, Parenti JL, Green SY, et al. Open repair of Thoracoabdominal aortic aneurysm in the Modern Surgical Era: contemporary outcomes in 509 patients. J Am Coll Surg. 2011;212(4):569–79.
Kertai MD, Tiszai-Szûcs T, Varga KS, et al. Intraoperative use of packed red blood cell transfusion and mortality in patients undergoing abdominal or thoracoabdominal aortic aneurysm surgery. J Cardiovasc Surg (Torino). 2009;50(4):501–8.
Dayama A, Sugano D, Reeves JG, et al. Early outcomes and perioperative risk assessment in elective open thoracoabdominal aortic aneurysm repair: an analysis of national data over a five-year period. Vascular. 2016;24(1):3–8.
Wedel C, Møller CM, Budtz-Lilly J, et al. Red blood cell transfusion associated with increased morbidity and mortality in patients undergoing elective open abdominal aortic aneurysm repair. PLoS ONE. 2019;14(7):e0219263.
Carson JL, Stanworth SJ, Roubinian N, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2016;10(10):CD002042.
Holst LB, Petersen MW, Haase N, Perner A, Wetterslev J. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ. 2015;350:h1354.
Gough CJR, Nolan JP. The role of adrenaline in cardiopulmonary resuscitation. Crit Care. 2018;22(1):139.
Coselli JS, de la Cruz KI, Preventza O, et al. Extent II Thoracoabdominal aortic aneurysm repair: how I do it. Semin Thorac Cardiovasc Surg. 2016;28(2):221–37.
Smit M, Coetzee AR, Lochner A. The pathophysiology of myocardial ischemia and perioperative myocardial infarction. J Cardiothorac Vasc Anesth. 2020;34(9):2501–12.
Lombardi JV, Carpenter JP, Pochettino A, et al. Thoracoabdominal aortic aneurysm repair after prior aortic surgery. J Vasc Surg. 2003;38(6):1185–90.
Safi HJ, Winnerkvist A, Miller CC 3rd, et al. Effect of extended Cross-clamp Time during Thoracoabdominal aortic aneurysm repair. Ann Thorac Surg. 1998;66(4):1204–9.
Regnier P, Lareyre F, Hassen-Khodja R, et al. Sexual dysfunction after abdominal aortic aneurysm Surgical Repair: current knowledge and future directions. Eur J Vasc Endovasc Surg. 2018;55(2):267–80.
Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381(9861):153–65.
Santos PM, Afrassiabi A, Weymuller EA Jr. Risk factors associated with prolonged intubation and laryngeal injury. Otolaryngol Head Neck Surg. 1994;111(4):453–9.
Jack Sariego. Vocal Fold hypomobility secondary to elective endotracheal intubation: a general surgeon’s perspective. J Voice. 2010;24(1):110–2.
Sue RD, Susanto I. Long-term complications of artificial airways. Clin Chest Med. 2003;24(3):457–71.
Acknowledgements
Special thanks are given to Dr. Y. F. Wang, who helped with the manuscript from initial conception until its publication.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SW wrote the manuscript and finished all the study protocol. SW, CW and YG completed the statistics. YT and JL finished the data reconciliation. YW was responsible for the design of this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical consent was approved by the Ethics Committee of Fuwai Hospital (Approval NO. 2019 − 1308). Patient consent was waived.
Consent for publication
All the co-authors approved to publish this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, S., Wang, C., Gao, Y. et al. Risk factors of 30-day and long-term mortality and outcomes in open repair of thoracoabdominal aortic aneurysm. J Cardiothorac Surg 19, 170 (2024). https://doi.org/10.1186/s13019-024-02666-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02666-2