Abstract
In this case report, we present the unique and intriguing case of a 57-year-old man who experienced exertional palpitations and shortness of breath for 5 years. He was diagnosed with idiopathic heart failure three years ago, leading to diuretic treatment. Physical examination revealed notable left lower extremity swelling, severe varicose veins, and cardiac murmurs. Echocardiography showed significant cardiac enlargement and severe functional mitral and tricuspid valve regurgitation. Computed tomography (CT) imaging uncovered a 10 mm left common iliac arteriovenous fistula, causing abnormal early filling of the inferior vena cava (IVC) and marked IVC dilation. Open surgical repair of the arteriovenous fistula resulted in symptom relief and improved cardiac function. This case underscores the importance of considering unusual causes in heart failure patients and highlights the value of early diagnosis and intervention in complex cardiac-vascular interactions.
Similar content being viewed by others
Background
Cardiac insufficiency, characterized by structural or functional alterations in the heart, results in compromised ventricular pumping efficiency and impaired filling capacity. This condition primarily stems from various etiological factors, such as myocardial damage, cardiac overload, or insufficient ventricular preload, which can lead to decreased cardiac output [1].
In this case report, we present a unique clinical scenario where cardiac insufficiency arises as a consequence of an abnormal arteriovenous shunt. The significance of this case lies in its rarity and atypical presentation, highlighting the need for a comprehensive understanding of the diverse mechanisms contributing to cardiac insufficiency. By examining this case in detail, we aim to shed light on the intricate relationship between cardiac physiology and unexpected vascular anomalies.
In the following sections, we will provide a comprehensive overview of the patient’s clinical history, diagnostic assessment, management, and outcome, offering insights into the pathophysiological mechanisms underlying cardiac insufficiency in the context of an abnormal arteriovenous shunt.
Case Presentation
A 57-year-old man presented with a 5-year history of exertional palpitations and shortness of breath. Three years ago, he was diagnosed with Idiopathic heart failure at a clinic and has been receiving diuretic treatment since then. Additionally, he had a surgical history of lumbar disk protrusion surgery performed 21 years ago.
Upon physical examination, the patient exhibited significant swelling in his left lower extremity, along with visible hyperpigmentation and severe varicose veins. In the precordial area, a Grade 2 early systolic murmur was detected. An unusual continuous murmur with an associated thrill was noted over the left lower abdomen.
Echocardiography revealed marked enlargement of the entire heart, with an end-diastolic diameter of 65 mm for the left ventricle and 53 mm for the right ventricle. Severe functional regurgitation was observed in both the mitral and tricuspid valve.
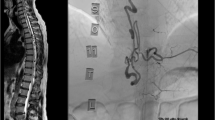
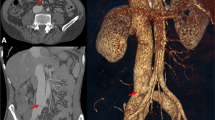
Further evaluation via computed tomography (CT) scan revealed a 10 mm left common iliac arteriovenous fistula. 3D volume-rendering CT angiography showed abnormal early filling of the inferior vena cava (IVC), left iliac vein, and right upper common iliac vein (Fig. 1). The IVC appeared significantly dilated, measuring approximately twice the diameter of the descending aorta on the same plane (Fig. 2).
Due to the small size of the patient’s left femoral artery, large size of fistula, which were contraindications for stent repair [2, 3], an open surgical procedure was performed through a transabdominal incision. Fistula was found between the posterior wall of the left iliac artery and iliac vein. The size was about 10 mm and the iliac vein was extremely dilated. The fistula was repaired directly with intermittent 4 − 0 prolene suture (Fig. 3). The incision of the iliac artery was closed followed by the closure of abdominal layers and the abdominal incision. The iliac vessel mumur disappeared after the surery.
The patient’s post-operative recovery was favorable, with a notable improvement in symptoms and satisfaction. A follow-up echocardiography examination conducted one week after the operation demonstrated significantly reduced functional mitral and tricuspid valve regurgitation (Fig. 4). Additionally, the diameter of the inferior vena cava had returned to almost normal, measuring 23 mm in the CT scan (Fig. 2).
Discussion
Clinically, unexplained cardiac enlargement and cardiac insufficiency present diagnostic challenges. In this case, the patient exhibited generalized cardiac enlargement and concurrent multiple valve insufficiencies, which could easily be misdiagnosed as primary cardiomyopathy. Additionally, the marked dilation of the inferior vena cava, often viewed as a secondary change in response to cardiac failure, further complicated the clinical picture.
What sets this case apart is the extreme extent of inferior vena cava dilation, far surpassing what is typically observed in cases of heart failure alone. Coupled with the patient’s history of lumbar spine disc surgery, the discovery of an iliac arteriovenous fistula emerged as a significant revelation. Such fistulas are exceedingly rare complications of spinal disc surgery [4]. This may be caused by the use of instruments such as the pituitary rongeur or forceps to perforate the anterior spinal ligament, which is anatomically very close to the vessels. Or it could be retroperitoneal inflammatory processes leading to adhesion of the vessel and the disc [5]. The massive iliac arteriovenous shunt imposed a substantial volume load on the heart, resulting in cardiac enlargement and insufficiency. Notably, congestive heart failure typically develops rapidly in such cases. However, this patient’s prolonged history of symptoms was exceptional.
Early detection and intervention to correct the fistula proved instrumental in halting the progression of heart enlargement and cardiac insufficiency. This case serves as a poignant reminder of the critical importance of considering uncommon etiologies in patients with cardiac insufficiency and highlights the value of swift diagnosis and treatment.
Conclusion
In summary, this case report illuminates the complexities of diagnosing cardiac enlargement and insufficiency, emphasizing the need to explore beyond conventional explanations, especially when faced with protracted and enigmatic clinical presentations. The identification of an iliac arteriovenous fistula related to lumbar spine disc surgery offers a valuable lesson in recognizing rare complications. Prompt intervention in cases such as these can halt the progression of heart enlargement and cardiac insufficiency, underscoring the importance of early detection and management to optimize patient outcomes.
Data availability
All data generated or analysed during this study are included in this published article.
References
Tsutsui H. Recent advances in the pharmacological therapy of chronic heart failure: evidence and guidelines. Pharmacol Ther. 2022;238:108185.
Cuypers PW, Laheij RJ, Buth J. Which factors increase the risk of conversion to open surgery following endovascular abdominal aortic aneurysm repair? The EUROSTAR collaborators. Eur J Vasc Endovasc Surg. 2000;20(2):183–9.
Patel S, et al. Successful open surgical repair of large ilio-caval fistula presenting with congestive heart failure. Indian J Thorac Cardiovasc Surg. 2022;38(1):96–8.
Papadoulas S, et al. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002;24(3):189–95.
Bojarski P, Sobstyl M. Vascular iatrogenic injury during lumbar disc surgery: a literature review. Pol Merkur Lekarski. 2021;49(291):231–4.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Zheng-Ji Chen, Nouman Ahmad, and Ling-Jin Huang. The first draft of the manuscript was written by Zheng-Ji Chen and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The authors affirm that human research participants provided informed consent for the publication of the images in Fig. 1a and b, and 1c.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, ZJ., Ahmad, N. & Huang, LJ. Unusual origins of cardiac insufficiency: a case of iliac arteriovenous fistula post-spinal disc surgery. J Cardiothorac Surg 19, 193 (2024). https://doi.org/10.1186/s13019-024-02664-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02664-4