Abstract
Background
This study aimed to evaluate the short-term and long-term outcomes of dialysis and non-dialysis patients after On-pump beating-heart coronary artery bypass grafting (OPBH-CABG).
Methods
We retrospectively reviewed medical records of 659 patients underwent OPBH-CABG at our hospital from 2009 to 2019, including 549 non-dialysis patients and 110 dialysis patients. Outcomes were in-hospital mortality, length of stay, surgical complications, post-CABG reintervention, and late mortality. The median follow-up was 3.88 years in non-dialysis patients and 2.24 years in dialysis patients. Propensity matching analysis was performed.
Results
After 1:1 matching, dialysis patients had significantly longer length of stay (14 (11–18) vs. 12 (10–15), p = 0.016), higher rates of myocardial infarction (16.85% vs. 6.74%, p = 0.037) and late mortality (25.93% vs. 9.4%, p = 0.005) after CABG compared to non-dialysis patients. No significant differences were observed in in-hospital mortality, complications, or post-CABG reintervention rate between dialysis and non-dialysis groups.
Conclusions
OPBH-CABG could achieve comparable surgical mortality, surgical complication rates, and long-term revascularization in dialysis patients as those in non-dialysis patients. The results show that OPBH-CABG is a safe and effective surgical option for dialysis patients.
Similar content being viewed by others
Background
Patients on dialysis have high risks for coronary artery diseases and displayed poor prognosis after coronary artery bypass grafting (CABG) compared to non-dialysis patients, including higher surgical mortality, postoperative complications, readmission rate, revascularization, and lower survival [1,2,3,4,5]. On-pump heart-beating CABG is a hybrid surgical approach maintaining stable hemodynamics with the support of cardiopulmonary bypass, but without cardioplegic arrest and aortic cross-clamping [6]. This may lead to lower myocardial injury, therefore is an option for patients with high-risk profiles. However, its outcomes in different high-risk groups remain further investigation. The purpose of this study was to evaluate short-term and long-term outcomes in dialysis and non-dialysis patients after on-pump beating-heart CABG.
Methods
Patients
This retrospective study enrolled patients underwent coronary artery on-pump beating-heart bypass surgery in our hospital between 2009 and 2019. Inclusion criteria were: 1) with coronary artery disease; 2) indicated for CABG surgery. No exclusion criteria. All necessary information was reviewed from medical record, including demography, clinical characteristics, and postoperative complications. The study was approved by the institutional review board, and the requirement of informed consent was waived.
Operative procedure of on-pump beating heart CABG and renal management
Our perioperative management of renal replacement therapy were as follows: 1) low-potassium hemodialysis (HD) for consecutive 3 days before operation; 2) only hemofiltration during bypass; 3) start of regular intermittent HD on the first postoperative day, followed by regular intermittent HD three times a week.
CABG was performed with a median sternotomy. A partial cardiopulmonary bypass was used. The left anterior descending (LAD) artery was anastomosed with left or right ITA graft. The non-LAD coronary arteries were grafted with a sequential saphenous vein graft (SVG). The distal end of SVG was anastomosed to ascending aorta using partially side-clamping of aorta. Intra-aortic blood pump (IABP) was used liberally pre- or post-operatively in patients with hemodynamic instability, unstable cardiac rhythms, or poor LV function.
Outcomes
Short-term outcomes were in-hospital mortality, length of stay, surgical complications. Long-term outcomes were adverse cardiac events, percutaneous coronary intervention (PCI) reintervention, and late mortality during follow-up. Adverse cardiac events included recurrent angina and myocardial infarction (MI). Late mortality is defined as death during follow-up.
Statistical analysis
Continuous data with a normal distribution were analyzed by Student’s t-test and are presented as the mean ± standard deviation (SD); continuous data without a normal distribution are presented as the median (interquartile range (IQR)) and were analyzed by the Wilcoxon rank-sum test. Normal distribution of variables was tested by Shapiro–Wilk. Categorical data were analyzed with the chi-square test or Fisher’s exact test and are presented as n (%), as appropriate. Patients were matched as propensity score (PS) with the ratio of dialysis: non-dialysis = 1:1 according to age, male sex, BMI, smoking status, preoperative EF, CCS angina class, diabetes mellitus, hyperlipidemia, cardiac dysfunction, PAOD, liver insufficiency, cerebral deficits, number of grafts, complete revascularization, grafting strategy. Kaplan–Meier plot was performed and used log-rank test to compare late mortality between non-dialysis and dialysis patients. Late mortality was identified as death after discharge, and the follow-up duration was estimated from surgery date to the last visit or death. A two-sided P-value of < 0.05 was regarded as statistically significant. Data management and statistical analyses were conducted with SAS version 9.4 software (SAS Institute, Inc.).
Results
Demographic characteristics
A total of 549 non-dialysis patients and 110 dialysis patients were included in this study (Table 1). Compared to dialysis patients, non-dialysis patients had significantly higher body mass index, higher proportions of male, current smoker, normal preoperative ejection fraction (EF), Canadian cardiovascular society (CCS) classes I and II, hyperlipidemia, complete revascularization, bilateral internal thoracic arteries grafting, and longer follow-up period. Non-dialysis patients also had significantly lower European system for cardiac operative risk evaluation (EuroSCORE), lower proportions of diabetes, cardiac dysfunction, peripheral artery occlusive disease (PAOD), liver insufficiency, and cerebral deficits. After PS matching, 89 non-dialysis patients and 89 dialysis patients were enrolled in the analysis. The characteristics between non-dialysis and dialysis groups were balanced, except EuroSCORE and follow-up period. Non-dialysis patients still had lower additive and logistic score and longer follow-up period.
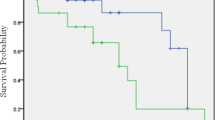
The outcomes after CABG between non-dialysis and dialysis patients after PS matching are presented in Table 2. After CABG, dialysis group had significantly higher longer length of stay (14 (11–18) vs 11 (9–14) days, p = 0.016), post-CABG MI frequency (16.85% vs. 6.74%, p = 0.037), and mortality rate (25.93% vs 9.41%, p = 0.005) than non-dialysis group. No significant differences in in-hospital mortality, surgical complications or post-CABG reintervention were observed between groups. Figure 1 presents the crude survival curves excluded in-hospital death. A significantly lower survival during follow-up was observed in dialysis group compared to the non-dialysis group (p < 0.001 with long rank test).
The outcomes of dialysis patients after CABG are presented in Table 3, including 99 patients with HD and 11 patients with peritoneal dialysis (PD). The in-hospital mortality was 7.07% in HD patients and 18.18% in PD patients (p = 0.222). No significant differences were found between the two groups, except the PD group had more cardiac complications than the HD group (18.18% vs 2.02%, p = 0.049).
Discussions
The results of the present study, dialysis patients had significantly worse outcomes compared to non-dialysis patients after on-pump beating-heart CABG, including longer length of stay, higher rate of post-CABG MI, and lower survival during follow-up. However, no significant differences in in-hospital mortality, surgical complications, or revascularization rate during follow-up were observed between dialysis and non-dialysis groups. Our results show that on-pump beating-heart CABG is a safe and effective option for dialysis patients.
In the present study, no significant differences in in-hospital mortality, surgical complications, or post-CABG reintervention during follow-up was observed between dialysis and non-dialysis patients. Dialysis is known as an independent risk factor for surgical mortality after CABG [1, 3,4,5]. Our results showed on-pump beating-heart CABG could achieve comparable short-term surgical outcomes in dialysis patients as those in non-dialysis patients. Meanwhile, Chen et al. reported a higher risk for revascularization after CABG in dialysis patients than non-dialysis patients [3]. It is well-recognized that on-pump CABG ensures comprehensive revascularization [7, 8]. Our result showed that on-pump beating-heart CABG achieves good long-term revascularization also in dialysis group. These results together show that it is a safe and effective option for dialysis patients.
Our results showed that dialysis patients had a significantly longer length of stay, higher rate of MI, and poorer survival after CABG compared to non-dialysis patients. Dialysis is significantly associated with poor outcomes after cardiac surgery [1,2,3,4,5], and the risk for mortality is elevated as dialysis-dependence duration extends [1, 3]. Studies have reported that dialysis patients show significantly higher 30-day mortality, readmission rate, rates of postoperative MI or revascularization, and lower survival after CABG compared to non-dialysis patients [1,2,3,4,5]. CABG is not associated with short-term mortality but improves life expectancy of dialysis patients [5, 9, 10]. For better prognosis, more attention must be paid on dialysis patients’ postoperative conditions after CABG, including monitoring cardiovascular stability, and education of self-care for patients and caregivers.
In the present study, PD patients showed twofold higher in-hospital mortality compared to HD patients without statistically significant difference (2/12 vs. 7/115, p = 0.222) probably due to the limited sample size. Studies reported that PD patients were prone to higher in-hospital mortality than HD patients after CABG [11, 12]. Further study is needed to clarify the underlying mechanism.
Limitation
The study had some limitations. First, it is a retrospective study with those inherent limitations. Second, the study had small sample size and unequal distribution of patients across the dialysis and non-dialysis groups, which may skew the analysis of outcomes. Therefore, PS matching analysis was employed to account for these variables.
Conclusion
After on-pump beating-heart CABG, dialysis patients have longer length of stay, higher rate of postoperative MI, and poor survival; whereas no significant differences in in-hospital mortality or revascularization rate during follow-up between dialysis and non-dialysis patients. Our findings show that on-pump beating-heart CABG could achieve comparable surgical mortality and good long-term revascularization in dialysis patients as those in non-dialysis patients. It is a safe and effective option for dialysis patients.
Availability of data and materials
The data analyzed available in the published article.
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- HD:
-
Hemodialysis
- ITA:
-
Internal thoracic artery
- IABP:
-
Intra-aortic blood pump
- PCI:
-
Percutaneous coronary intervention
- MI:
-
Myocardial infarction
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- CIs:
-
Confidence intervals
- HR:
-
Hazard ratio
- PAOD:
-
Peripheral artery occlusive disease
- EF:
-
Ejection fraction
- CCS:
-
Canadian cardiovascular society
- BITA:
-
Bilateral internal thoracic arteries
References
Bianco V, Kilic A, Gleason TG, Aranda-Michel E, Navid F, Sultan I. Longitudinal outcomes of dialysis-dependent patients undergoing isolated coronary artery bypass grafting. J Card Surg. 2019;34(3):110–7.
Leontyev S, Davierwala PM, Gaube LM, Röhrig KA, Lehmann S, Holzhey DM, et al. Outcomes of dialysis-dependent patients after cardiac operations in a single-center experience of 483 patients. Ann Thorac Surg. 2017;103(4):1270–6.
Chen SW, Chang CH, Lin YS, Wu VC, Chen DY, Tsai FC, et al. Effect of dialysis dependence and duration on post-coronary artery bypass grafting outcomes in patients with chronic kidney disease: A nationwide cohort study in Asia. Int J Cardiol. 2016;223:65–71.
Sezai A, Nakata K, Hata M, Yoshitake I, Wakui S, Hata H, et al. Long-term results of dialysis patients with chronic kidney disease undergoing coronary artery bypass grafting. Ann Thorac Cardiovasc Surg. 2013;19(6):441–8.
Charytan DM, Kuntz RE. Risks of coronary artery bypass surgery in dialysis-dependent patients–analysis of the 2001 National Inpatient Sample. Nephrol Dial Transplant. 2007;22(6):1665–71.
Perrault LP, Menasche P, Peynet J, Faris B, Bel A, de Chaumaray T, et al. On-pump, beating-heart coronary artery operations in high-risk patients: an acceptable trade-off? Ann Thorac Surg. 1997;64:1368–73.
Jiang Y, Xu L, Liu Y, Deng B, Dong N, Chen S. Beating-heart on-pump coronary artery bypass grafting vs. off-pump coronary artery bypass grafting: a systematic review and meta-analysis. J Thorac Dis. 2021;13(7):4185–94.
Wang C, Jiang Y, Jiang X, Chen S. On-pump beating heart versus conventional on-pump coronary artery bypass grafting on clinical outcomes: a meta-analysis. J Thorac Dis. 2021;13(7):4169–84.
Hemmelgarn BR, Southern D, Culleton BF, Mitchell LB, Knudtson ML, Ghali WA, et al. Survival after coronary revascularization among patients with kidney disease. Circulation. 2004;110(14):1890–5.
Hsu HL, Hsu HP, Yu BF, Lu TM, Huang CY, Shih CC, et al. Long-term results of coronary artery bypass grafting in patients with dialysis-dependent renal failure. J Cardiovasc Surg (Torino). 2015;56(5):809–16.
Li HY, Chang CH, Lee CC, Wu VC, Chen DY, Chu PH, et al. Risk analysis of dialysis-dependent patients who underwent coronary artery bypass grafting: Effects of dialysis modes on outcomes. Medicine (Baltimore). 2017;96(39):e8146.
Wang Z, Gong Y, Fan F, Yang F, Qiu L, Hong T, et al. Coronary artery bypass grafting vs. drug-eluting stent implantation in patients with end-stage renal disease requiring dialysis. Ren Fail. 2020;42(1):107–12.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Guarantor of integrity of the entire study: Chia-Hsun Lin, Ming-Jen Lu. Study concepts: Chia-Hsun Lin, Ming-Jen Lu. Study design: Chia-Hsun Lin, Ming-Jen Lu. Clinical studies: Chia-Hsun Lin, Ming-Jen Lu. Data acquisition: Yen-Yang Chen, Yu-Tong Yen, Patrick Hung-Ju Kao. Data analysis: Chai-Hock Chua, Hung-Hsing Chao. Statistical analysis: Yen-Yang Chen, Yu-Tong Yen, Patrick Hung‐Ju Kao. Manuscript preparation: Chia-Hsun Lin, Yen-Yang Chen, Ming-Jen Lu. Manuscript editing: Chia-Hsun Lin, Yen-Yang Chen, Yu-Tong Yen, Ming-Jen Lu. Manuscript review: Chia-Hsun Lin, Yen-Yang Chen, Yu-Tong Yen, Patrick Hung-Ju Kao, Chai-Hock Chua, Hung-Hsing Chao, Ming-Jen Lu. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of Shin Kong Wu Ho-Su Memorial Hospital (No.20220703R), and informed consent was waived by the institutional review board of Shin Kong Wu Ho-Su Memorial Hospital. All methods were carried out in accordance with relevant guidelines and regulations
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, CH., Chen, Y., Yen, Y. et al. Short-term and long-term outcomes of on-pump beating-heart coronary artery bypass surgery in dialysis and non-dialysis patients: a retrospective study in a single center. J Cardiothorac Surg 19, 268 (2024). https://doi.org/10.1186/s13019-024-02662-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02662-6