Abstract
Background
Aortic intramural hematoma (IMH) is one of the typical entities of acute aortic syndrome and probably accounts for 5–25% of all cases. The ulcer-like projections (ULP), which are described as a focal, blood-filled pouch protruding into the hematoma of the aortic wall, are regarded as one of the high-risk imaging features of IMH and may cause initial medical treatment failure and death.
Case presentation
We present a case report of an acute type B IMH patient with impaired renal function and newly developed ULP in the acute phase. The 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging (18F-FDG PET/MR) was performed to evaluate the condition of aortic hematoma. The 18F-FDG focal uptake along the aortic wall of the hematoma was normal compared to the background (SUVmax 2.17; SUVSVC 1.6; TBR 1.35). We considered the IMH stable in such cases and opted for medical treatment and watchful observation. Six months after discharge, the patient’s recovery was satisfactory, and aortic remodeling was ideal.
Conclusions
The 18F-FDG PET/MR is a novel tool to evaluate the risk of IMH patients and thus provides information for therapy selection.
Similar content being viewed by others
Background
Acute type B aortic intramural hematoma (IMH) is characterized by dramatic evolution and may evolve into aortic dissection and even rupture, which frequently cause initial medical treatment failure and death [1]. Here, we present a case in which we utilized 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging (18F-FDG PET/MR) to evaluate the risk of type B IMH.
Case presentation
A 58-year-old man presented with severe chest pain and elevated blood pressure (188/79 mm Hg). Heart rate was 120 beats/min and respiratory rate was 22 breaths/min. Oxygen saturation was sufficient on room air. Urgent laboratory testing showed increased creatinine level (185 μmol/L, 2.09 mg/dl) without metabolic acidosis. Urgent contrast-enhanced computed tomography (CT) was performed and an acute type B aortic IMH extending from the distal aortic arch to the iliac artery bifurcation was noted (Fig. 1). The maximal aortic diameter was 39 mm and the maximal hematoma thickness was 10 mm. Initial CT detected no ulcer-like projections (ULP).
The urgent contrast-enhanced computed tomography image on admission shows intramural hematoma of the descending aorta. A The section of the maximal aortic diameter (line). B The section of maximal hematoma thickness (line). C Sagittal contrast-enhanced computed tomography shows intramural hematoma of the descending aorta (star)
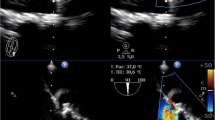
To better evaluate the condition of the aortic hematoma, 18F-FDG PET/MR (PET and MRI acquisition parameters can be requested from the authors) was performed three days after admission, and a newly developed ULP located in the distal aortic arch was observed (Fig. 2). The maximum standardized uptake value of the aortic wall (SUVmax), the maximum standardized uptake value of superior vena cava (SUVSVC), and the target-to-blood ratio (TBR, SUVmax divided by SUVSVC) were calculated through PET. Interestingly, the 18F-FDG focal uptake along the aortic wall of the hematoma was normal compared to the background (SUVmax 2.17; SUVSVC 1.6; TBR 1.35). The maximal aortic diameter was 36 mm and the maximal hematoma thickness was 9 mm. In such cases, we considered the IMH stable even though it appeared newly developed ULP in the proximal descending aorta. Therefore, we opted for watchful observation and the patient was discharged one week later. Six months after discharge, the patient’s recovery was satisfactory, and aortic remodeling was ideal.
18F-fluorodeoxyglucose positron emission tomography/ magnetic resonance imaging. A Magnetic resonance imaging shows intramural hematoma with newly developed ULP on the arch (arrow). B The metabolism of the aortic wall was assessed by 18F-fluorodeoxyglucose positron emission tomography. C Fusion image of intramural hematoma
The patient’s recovery was satisfactory after six months. He had not experienced chest pain since discharged and the blood pressure (128/75 mm Hg) and heart rate (65–70 bpm) were well controlled. The contrast-enhanced CT showed that, compared with the previous CT result, no matter whether the maximal aortic diameter or the maximal hematoma thickness was reduced (Fig. 3). Owing to the ideal aortic remodeling, the patient received medical treatment continually and was under close follow-up.
The contrast-enhanced computed tomography image shows the hematoma was significantly resolved and the ULP on the aortic arch disappeared after three months. A The transverse section of the aortic arch. B The section of the maximal aortic diameter (line). C Sagittal contrast-enhanced computed tomography shows resolved intramural hematoma of the descending aorta
Discussion and conclusions
According to the latest guideline, the ULP involving the descending thoracic aorta if it develops in the acute phase is regarded as one of the high-risk imaging features of IMH [2]. However, in our previous experience, not all forms of acute newly developed ULP are associated with poor outcomes. The 18F-FDG PET/CT provided a valuable approach for predicting risk in patients with type B IMH. As for this patient, we performed 18F-FDG PET/MR to further assess the IMH condition. It’s known that MR can provide coverage of the entire aorta and branch vessels, which can characterize aortic wall changes in the setting of inflammation and AAS [3]. As mentioned above, the 18F-FDG focal uptake along the aortic wall of the hematoma of this patient was normal compared to the background (SUVmax 2.17; SUVSVC 1.6; TBR 1.35). Based on our previous findings, the TBR of 1.5 had an acceptable predictive value for differentiating high-risk from low-risk patients. Regarding pathophysiology, acute inflammation could result in the accumulation of hypermetabolic cells such as macrophages and enhanced 18F-FDG uptake [4]. In addition, 18F-FDG PET/MR does not require contrast media, which can cause acute kidney injury. Therefore, 18F-FDG PET/MR not only evaluated the risk of IMH but also avoided the impairment of this patient's renal function.
This is one of the first case reports of a patient using 18F-FDG PET/MR as a complementary diagnostic tool for the anatomic-functional evaluation for patients with high-risk imaging features. Further analysis involving larger samples are suggested to validate the efficacy of 18F-FDG PET/MR in IMH patients.
Availability of data and materials
Data available on request.
Abbreviations
- IMH:
-
Intramural hematoma
- AAS:
-
Acute aortic syndrome
- ULP:
-
Ulcer-like projections
- 18F-FDG PET/MR:
-
18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging
References
Bossone E, LaBounty TM, Eagle KA. Acute aortic syndromes: diagnosis and management, an update. Eur Heart J. 2018;39(9):739–749d.
Isselbacher EM, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022;146(24):e334–482.
Barra L, et al. Imaging modalities for the diagnosis and disease activity assessment of Takayasu’s arteritis: a systematic review and meta-analysis. Autoimmun Rev. 2018;17(2):175–87.
Yang F, et al. Predictive value of (18)F-FDG PET/CT in patients with acute type B aortic intramural hematoma. J Nucl Cardiol. 2019;26(2):633–41.
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
FY contributed to the study conception and design, analysis and interpretation of data, drafting of the manuscript, and critical revision of the manuscript; YC contributed to acquisition of data and critical revision of the manuscript; YZ and DS made a contribution to image data analyses and revision of the manuscript; JL served as primary consultant in the management of the patient, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Guangdong Provincial People’s Hospital Ethics Committee (KY-Z-2020-080-02). Written informed consent was waived.
Consent for publication
Written informed consent for publication of their clinical details and clinical images was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, F., Chen, Y., Zhou, Y. et al. Evaluation of intramural hematoma: a novel use of 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging. J Cardiothorac Surg 19, 133 (2024). https://doi.org/10.1186/s13019-024-02598-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02598-x