Abstract
Background
With the implementation of lung cancer screening programs, an increasing number of pulmonary nodules have been detected.Video-assisted thoracoscopic surgery (VATS) could provide adequate tissue specimens for pathological analysis, and has few postoperative complications.However, locating the nodules intraoperatively by palpation can be difficult for thoracic surgeons. The preoperative pulmonary nodule localization technique is a very effective method.We compared the safety and effectiveness of two methods for the preoperative localization of pulmonary ground glass nodules.
Methods
From October 2020 to April 2021, 133 patients who underwent CT-guided single pulmonary nodule localization were retrospectively reviewed. All patients underwent video-assisted thoracoscopic surgery (VATS) after successful localization. Statistical analysis was used to evaluate the localization accuracy, safety, information related to surgery and postoperative pathology information. The aim of this study was to evaluate the clinical effects of the two localization needles.
Results
The mean maximal transverse nodule diameters in the four-hook needle and hook wire groups were 8.97 ± 3.85 mm and 9.00 ± 3.19 mm, respectively (P = 0.967). The localization times in the four-hook needle and hook wire groups were 20.58 ± 2.65 min and 21.43 ± 3.06 min, respectively (P = 0.09). The dislodgement rate was significantly higher in the hook wire group than in the four-hook needle group (7.46% vs. 0, P = 0.024). The mean patient pain scores based on the visual analog scale in the four-hook needle and hook wire groups were 2.87 ± 0.67 and 6.10 ± 2.39, respectively (P = 0.000). All ground glass nodules (GGNs) were successfully resected by VATS.
Conclusions
Preoperative pulmonary nodule localization with both a four-hook needle and hook wire is safe, convenient and effective.
Similar content being viewed by others
Background
Lung cancer is the leading cause of cancer-related deaths [1]. Although the 5-year survival rate of lung cancer is only 15%, early diagnosis and treatment can increase it to 50% [2]. With the widespread use of low-dose spiral computed tomography (CT), an increasing number of pulmonary nodules can be detected [3]. These pulmonary nodules take on three forms on CT: pure ground glass nodules (GGNs), mixed GGNs, and solid nodules. Studies have shown that the malignant percentage of pure GGNs is 59–73%, whereas that of pure solid nodules is 7–9% [4]. Therefore, nodules that are classified based on the relevant imaging manifestations should be subjected to further pathological evaluation, whether by percutaneous lung biopsy, bronchoscopy or minimally invasive thoracoscopic surgery [5]. Some nodules are smaller in diameter, have fewer solid components, or are located deep in the lungs. Routine aspiration biopsy or needle aspiration biopsy for pathology becomes a challenge. Some scholars report that the accuracy of puncture biopsy for less than 1 cm lung nodules under CT guidance is only 48.5% [6]. When nonsurgical biopsy is not available or if the diagnosis is unclear, thoracic surgical biopsy is needed to further clarify the pathological diagnosis. Compared with conventional thoracotomy, thoracoscopy has advantages because it does not require conventional thoracotomy and causes less trauma [7]. Video-assisted thoracoscopic surgery (VATS) provides adequate tissue specimens for pathological analysis, is more comfortable and has fewer postoperative complications, making it ideal for the treatment of pulmonary nodules. Compared with thoracotomy, VATS not only provides adequate tissue specimens for pathological analysis but is also more comfortable, which makes it an ideal treatment for pulmonary nodules [7, 8]. Due to the small pulmonary nodules, deep location or soft nodule texture, it is difficult to manually reach nodules with just the fingers during VATS, and this can even lead to the need for conventional thoracotomy surgery. It may even lead to a routine thoracotomy. The preoperative pulmonary nodule localization technique is a very effective method to mitigate this challenge. Currently, a variety of auxiliary devices can be used, including hook wire, protein glue localization, methylene blue injection, intraoperative ultrasound localization, intraoperative electromagnetic navigation, and immunofluorescence methods [9–14]. Each method has its own advantages and disadvantages. Among these methods, the hook wire was one of the first applied lung nodule needles and is very popular in positioning, with a success rate of up to 96%. The four-hook needle is a modified localization needle for pulmonary nodules. Currently, few articles have compared the two methods. The purpose of this study was to compare the safety and effectiveness of the two mentals for the preoperative localization of pulmonary nodules.
Methods
Materials
We retrospectively analyzed the clinical data of 180 consecutive patients who underwent preoperative localization in the Department of Thoracic Surgery of our institution from October 2020 to April 2021. All patients underwent routine pulmonary function examination, craniocerebral magnetic resonance imaging or CT, systematic bone scan, abdominal ultrasound or CT to exclude possible metastases, and analysis of related tumor markers. After plain or enhanced CT scans, all images were transferred to an AW4.6 workstation (GE Healthcare, Chicago, IL, USA) for postprocessing. The inclusion criteria for VATS for patients with GGN were as follows: [1] GGN confirmed by high-resolution CT; [2] single GGN; [3] GGN difficult to detect during an operation; [4] GGN suspected of being malignant; and [5] distance from the pleura of 5-40 mm. The exclusion criteria were as follows: multiple lesions and the identification of two or more GGNs simultaneously. There were 133 eligible patients.
CT-guided localization process
All CT-guided localizations of GGNs were performed by the same radiologist who had engaged in CT-guided intervention for 15 years. All CT scans were performed on a 64-row multislice spiral CT (GE Healthcare, USA). A four-hook needle (model: SS510-10 Senscure, China) (Fig. 1a and b) or hook wire (20 g×120 mm; Pajunk, Germany) was used for puncture. The four-hook needle is composed of a 19G coaxial needle, tri-colored suture, 4-hook anchor, pusher, release buckle, and protection tube. Before positioning, the surgeon and the radiologist reviewed the CT images together to determine whether the pulmonary nodules could be located. Then, a path that avoided the vessels, trachea and interleaf pleura was determined by the radiologist. After routine disinfection and drape laying, 2% lidocaine was used to locally anesthetize the layers of the chest wall. The localization needle was inserted into the desired depth according to the standard four-hook wire procedure (Fig. 2a) [15].CT was performed again, and the needle inlet angle and depth were adjusted according to the image until the tip was located in the GGN or within 1 cm. The claw hook was released through a puncture needle. After successful localization, another CT scan was performed again to determine the spatial location relationship between the pulmonary nodules and the localization needle (Fig. 3a), as well as if there was pneumothorax and hemorrhage. The processes of hook wire localization were similar to those in the four-hook needle group. After the target nodule was confirmed, a reasonable path was chosen based on the CT images, and then the localization needle was inserted around the nodule (Fig. 3a and b). After successful positioning, the patient was placed in a moving bed or wheelchair and delivered to the operating room.
Thoracoscopic surgical procedure
After positioning, the patients were immediately transferred to the operating room for thoracoscopic surgery. After successful general anesthesia and endotracheal intubation, the patients were placed in an appropriate lateral decubital position. During thoracoscopic surgery, surgeons can easily determine the location of the pulmonary nodules and anchor depth according to the location of the localization needle (Figs. 2c and 3c). Partial lobe resection (wedge or segment resection) was performed using a margin of more than 2 cm from the edge of the lesion according to the preoperative surgical plan. The resected specimen was subjected to intraoperative rapid frozen pathology examination. The patients with malignant nodules greater than 2 cm in diameter underwent routine lobectomy and lymph node dissection or sampling.All patients received postoperative analgesia with patient controlled intravenous analgesia(PCIA )with sufentanil 0.05ug/Kg.h.
Variables
The primary outcomes were the marking time and procedure success. The time from obtaining the first CT image to obtaining the last CT image was defined as the marking time. Localization success was defined as a localization marker in or within 10 mm of the nodules measured on the final images of the procedure.The time from cutting the skin to closing the incision was defined as the operative time. Extubation time was the time from pleural drainage tube insertion to removal.Complications (e.g., pneumothorax and pulmonary hemorrhage) were assessed. The pain visual analog scale (0–10) was used to assess the pain level after positioning.
Statistical analysis
The statistical analysis software that was used was SPSS v21.0 (SPSS Inc., USA). Descriptive statistics for continuous variables are presented as the mean ± standard deviation or median. Continuous variables were analyzed by t tests, and categorical variables were compared by chi-square, Pearson, and Fisher tests. A value of P < 0.05 was considered significant.
Results
In total, 133 patients were included in this study. The clinical characteristics of the patients and nodules are shown in Table 1. There were no significant differences in age, sex, nodule distribution, operative technique or type of nodule between the two groups. The mean maximal transverse nodule diameters in the four-hook needle and hook wire groups were 8.97 ± 3.85 mm and 9.00 ± 3.19 mm, respectively (P = 0.967). The mean distances from the nodule margins to the superficial pleura in the four-hook needle and hook wire groups were 10.94 ± 1.63 mm and 11.32 ± 1.36 mm, respectively (P = 0.150). The localization times in the four-hook needle and hook wire groups were 20.58 ± 2.65 min and 21.43 ± 3.06 min, respectively (P = 0.09). Pneumothorax, hemorrhage and dislodgement were the primary localization complications. In this study, there was no significant difference between the groups regarding pneumothorax or hemorrhage. The dislodgement rate was significantly higher in the hook wire group than in the four-hook needle group (7.46% vs. 0, P = 0.024). The mean patient pain scores based on the visual analog scale in the four-hook needle and hook wire groups were 2.87 ± 0.67 and 6.10 ± 2.39, respectively (P = 0.000) (Table 2).
The pathological diagnostic results for the GGNs were as follows: invasive adenocarcinoma (n = 48), minimally invasive adenocarcinoma (n = 56), carcinoma in situ (n = 11), atypical adenomatous hyperplasia (n = 9), fibroinflammatory nodule (n = 5), inflammation (n = 2), hamartoma (n = 1) and cryptococcus infection (n = 1) (Table 3).
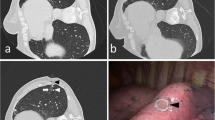
A 56-year-old female with a GGN in the right middle lobe who underwent CT-guided localization with a four-hook needle. (a) The lesion (black arrow) is observed on an axial CT image. (b) Postlocalization CT shows the relationship among the released anchor (white arrow), lesion (black arrow) and chest wall. (c) The end of the four-hook needle (white hollow arrow) is visualized during VATS.
A 65-year-old female with a GGN in the right lower lobe who underwent CT-guided localization with a hook wire needle. (a) The lesion (black arrow) is observed on an axial CT image. (b) A hook wire needle (black arrow) is inserted around the lesion; postlocalization CT shows the relationship among the needle (black arrow), lesion (white arrow) and chest wall. (c) The end of the four-hook needle (white hollow arrow) is visualized during VATS.
Discussion
With the implementation of lung cancer screening programs, an increasing number of pulmonary nodules have been detected, which provides a better opportunity for the early diagnosis and treatment of lung cancer. Early surgical treatment will improve the 5-year survival rate of postoperative lung cancer. The precise intraoperative localization of pulmonary nodules is a challenge for every thoracic surgeon. When the nodules are small or are pure ground glass nodules, it is difficult to accurately locate them through observation and touch during the operation, which increases the difficulty of the operation, extends the operation time, and increases the risk of resection of normal lung tissue. Thus, accurate and safe preoperative localization is very important. Previous localization methods have corresponding disadvantages [16]. For example, methylene blue injection may stain widely with dose and time, resulting in inaccurate localization [17]. The safety trauma of spring coil localization is small, but the possibility of shedding is large. In recent years, a new four-hook localization needle has emerged, and the four-hook needle and hook wire methods have become two commonly used localization methods. We retrospectively compared the use of the two localization needles in pulmonary nodule localization. The localization success rates of the four-hook needle and hook wire groups were 100% and 98.5%, respectively. There was no significant difference between the two groups for the marking time.
The hook wire is a commonly used localization tool in recent years and is used initially for breast nodule localization. The front end of the hook wire is a single barb with a rigid tail wire. After positioning, the metal barbs can fix it in the lung tissue. The attached guide wire extends outward across the chest wall and sticks to the skin, so changes in the body position and respiratory movement could lead to the dislodgement or migration of the localization needle and result in localization failure. In this study, dislodgement or migration occurred in 5 patents in the hook wire group, similar to reports in the literature [18]. Location needle decoupling often occurred while the patients were transported to the operating room or while waiting for surgery. Therefore, our experience revealed that after successful positioning, the patient should be transferred immediately to the operating room for surgery. Even if decoupling occurs, the location of the pulmonary nodules can be determined by the hematoma on the surface of the lung during surgery, and the pulmonary nodules can be successfully removed. In this study, the pulmonary nodules were successfully removed in all five decoupled patients in the hook wire group.
The four-hook needle is basically the same as the hook wire. However, the tip claw is composed of 4 metal hook claws, which have a strong binding force with the surrounding tissue, and the position is relatively fixed. The flexible wire left in the chest wall has a weak pull force on the anchor hook, which is not easy to shift while the patients are waiting for surgery, and even if the shallow lesions are located, the anchor hook does not easily fall off and shift. Because the anchoring force of the anchor hook on the surrounding lung tissue is strong enough, the lung tissue in the focal area can be raised through the lifting tricolour line during the operation, and the operative field is exposed easily. In this study, no cases of decoupling or displacement occurred in the four-hook needle group. From our experience at our center, the operator can obviously touch the anchor hook of the anterior segment of the four-hook needle, and the operator can easily determine the nodule position by judging the localization point and anchor hook position.
Pneumothorax and hemorrhage are common complications during localization. In this study, there were no significant differences between the two groups, indicating that the two positioning methods were both effective and safe.None of the patients required special treatment.
After hook wire positioning, the hard wire that was placed through the partial pleura and the chest wall was fixed on the body surface, leading to hard wire rubbing against the wall pleural membrane due to the motion of the lung tissue, resulting in poor experience and pain for the patient [19]. The localization line of the four-hook needle posterior connection is a soft line that can be released into the chest cavity during positioning, which can reduce the stimulation of the mural pleura and significantly reduce the patient’s chest pain [20]. In this study, the average patient pain score was significantly higher in the hook wire group than in the four-hook needle group before VATS resection. According to the standard visual analog scale, the mean patient pain score in the four-hook needle group was 2.87 ± 0.67 in this study, which was similar to the report of 2.96 ± 1.43. Due to the good comfort of the four-hook needle, it was not necessary to perform the surgery immediately after applying the four-hook needle positioning, which made it easier to arrange the localization and operation time [21]. In the hook wire group, one patient had a severe pleural reaction due to pain after localization because after positioning, the patient immediately had chest tightness, dyspnea, a pale face, sweating, and decreased heart rate and blood pressure. The patient’s pleural response symptoms gradually improved after emergency oxygen, fluid rehydration and anti-shock treatment. Some scholars believe that the pleura is rich in sensory nerves, and pain stimulation can lead to an increased incidence of pleural response. Pleural pain caused by puncture localization can stimulate the cerebral cortex and hypothalamus, causing dilation of blood vessels, lowering of blood pressure, slowing heart rate, and even shock in severe cases 22.
Our results have several shortcomings.This study is a single-center retrospective study and it lacks large multicenter, randomized controlled trials to support the present findings. In addition, We did not compare postoperative follow-up for the two localization methods.
Conclusions
This study identified that the two preoperative localization methods were safe, convenient and effective. There was no difference in the localization time, success rate, pneumothorax or hemorrhage complications. The postoperative localization pain score and dislodgement rate in the four-hook needle group were slightly lower than those in the hook wire group.
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- GGO:
-
Ground-glass opacity
- VATS:
-
Video-assisted thoracoscopic surgery
- GGN:
-
Ground-glass nodule
References
Sands J, Tammemagi MC, Couraud S, Baldwin DR, Borondy-Kitts A, Yankelevitz D, Lewis J, Grannis F, Kauczor HU, Von Stackelberg OJ. J. o. t. o. o. p. o. t. I. A. f. t. S. o. L. C., Lung Screening Benefits and Challenges: A Review of The Data and Outline for Implementation. 2021, (1), 16.
Mariusz C, Jacek P, Beata J-P, Joanna R, Anna SCJO, Therapy. Quality of life of patients with lung cancer. 2016, 9, 1023–8.
Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks J. D. J. N. E. J. M., Reduced lung-cancer mortality with low-dose computed tomographic screening. 2011, (5).
Wahidi MM, Govert JA, Goudar RK, Gould MK, Mccrory DCJC. Evidence for the treatment of patients with pulmonary nodules: when is it lung cancer? ACCP evidence-based Clinical Practice Guidelines (2nd Edition). 2007;132(3):94S–107S.
Michael K, Gould J, William D, Lynch R, Chest P. J. J., Evaluation of individuals with Pulmonary nodules: when is it Lung Cancer? Diagnosis and management of Lung Cancer. 3rd ed. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines; 2013.
Shimizu K, Ikeda N, Tsuboi M, Hirano T, Kato HJLC. Percutaneous CT-guided fine needle aspiration for lung cancer smaller than 2 cm and revealed by ground-glass opacity at CT. 2006, 51 (2), 173–9.
Fu YF, Zhang M, Wu WB, Wang TJ. J. L. A. S. T. A., Coil Localization-Guided Video-Assisted Thoracoscopic Surgery for Lung Nodules. 2017, lap.2017.0484.
Yao F, Wang J, Yao J, Xu L, Wang J, Gao L. J. I. J. o. S., Reevaluation of the efficacy of preoperative computed tomography-guided hook wire localization: A retrospective analysis. 2018, 51, 24–30.
Guisong S. ; Tong; Qiu; Yunpeng; Xuan; Yandong; Zhao; Wenjie; cancer, J. J. Z. f. a. z. z. C. j. o. l., [Clinical Application of Vectorial Localization of Peripheral Pulmonary Nodules Guided by Electromagnetic Navigation Bronchoscopy in Thoracic Surgery]. 2019, 22 (11), 709–713.
Hou Yo, Wang Y, Guo Hi, Zhang YK, Han HL. J. T. C., Ultrasound location of pulmonary nodules in video゛ssisted thoracoscopic surgery for precise sublobectomy. 2020, 11 (6).
Rho J, Lee JW, Quan YH, Choi BH, Shin BK, Han KN, Kim BM, Choi YH, Yong HS, Kim HK. J. A. S., Fluorescent and Iodized Emulsion for Preoperative Localization of Pulmonary Nodules. 2021, (5).
Wen-Hua; Zhang Y-Y, Bai W, Medicine GMG-Xia;C. L. J., Application of intrapulmonary wire combined with intrapleural fibrin glue in preoperative localization of small pulmonary nodules. 2019, 98 (4), e14029.
Wicky S, Mayor B, Cuttat JF, Schnyder PJC. CT-guided localizations of pulmonary nodules with methylene blue injections for thoracoscopic resections. 1994, 106 (5), 1326.
Zhao G, Yu X, Chen W, Geng G, Jiang JJ. J. o. C. S., Computed tomography-guided preoperative semi-rigid hook-wire localization of small pulmonary nodules: 74 cases report. 2019, 14 (1).
Chen ZM, Xu JY, Cai WQ, Liao FC, Huo SQ, Yang JW, Peng J. The 4-hook anchor coaxial needle with scaled suture is superior to the double spring coil for preoperative localization. J Journal of Thoracic Disease 2021, (7).
Liu B, Gu CJJ, o. CR, Therapeutics. Expert consensus workshop report: guidelines for preoperative assisted localization of small pulmonary nodules. 2020, 16 (5), 967–73.
Vandoni RE, Jean-François C, Stéphane W, Michel SJE. J. o. C.-T. S., CT-guided methylene-blue labelling before thoracoscopic resection of pulmonary nodules. 1998, (3), 265–270.
Chest CHPKHJHSM. L. J., Comparative effectiveness and safety of preoperative lung localization for pulmonary nodules. A Systematic Review and Meta-analysis; 2017.
Mayo JR, Clifton JC, Powell TI, English JC, Evans KG, Yee J, Mcwilliams AM, Lam SC, Finley RJ. J. R., Lung nodules: CT-guided placement of microcoils to direct video-assisted thoracoscopic surgical resection. 2009, (2), 250.
Liwen Fan AB, Haitang Yang CD, E LMY, A ZW, E JY, A YZ, Deng Cai A, A HZ, A, Surgery C. F. Y. J. T. J. o. T., Multicenter, prospective, observational study of a novel technique for preoperative pulmonary nodule localization - ScienceDirect. 2019.
Li CD, Huang ZG, Sun HL, Wang LT, Wang YL, Gao BX, Yang MXJE. r., marking ground glass nodules with pulmonary nodules localization needle prior to video-assisted thoracoscopic surgery. 2022, (7), 32.
Julia S, Zhiqiu X, Lisco SJ, Rozanski GJ, Schultz HD, Zucker IH, Han-Jun WJP. R., Sympatho〆xcitatory response to pulmonary chemosensitive spinal afferent activation in anesthetized, vagotomized rats. 2018, 6 (12), e13742-.
Acknowledgements
None.
Funding
This study was supported by the Science and Technology Development Project of Weifang (2021YX072).
Author information
Authors and Affiliations
Contributions
Lijun Jing and Yongming Wang contributed equally to this work. LJJ and YMW made substantial contributions to the conception and design of the work. GCW,CSL,SBW and JZL made substantial contributions to the acquisition, analysis, and interpretation of data for the work. All authors gave their final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. This study was approved by the Ethics Committee of the Second People’s Hospital of Weifang.
Consent for publication
We obtained consent to publish individual patient data from the participants (or legal parent or guardian).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Jing, L., Liang, C. et al. Comparison of the safety and effectiveness of the four-hook needle and hook wire for the preoperative positioning of localization ground glass nodules. J Cardiothorac Surg 19, 35 (2024). https://doi.org/10.1186/s13019-024-02497-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02497-1