Abstract
Background
Pregabalin may have some potential in alleviating pain after thoracic surgery, and this meta-analysis aims to explore the impact of pregabalin on pain intensity for patients undergoing thoracic surgery.
Methods
PubMed, EMbase, Web of science, EBSCO and Cochrane library databases were systematically searched, and we included randomized controlled trials (RCTs) assessing the effect of pregabalin on pain intensity after thoracic surgery.
Results
Five RCTs were finally included in the meta-analysis. Overall, compared with control intervention for thoracic surgery, pregabalin was associated with significantly reduced pain scores at 0 h (mean difference [MD]=-0.70; 95% confidence interval [CI]=-1.10 to -0.30; P = 0.0005), pain scores at 24 h (MD=-0.47; 95% CI=-0.75 to -0.18; P = 0.001) and neuropathic pain (odd ratio [OR] = 0.24; 95% CI = 0.12 to 0.47; P < 0.0001), but demonstrated no obvious impact on the incidence of dizziness (OR = 1.07; 95% CI = 0.15 to 7.46; P = 0.95), headache (OR = 1.00; 95% CI = 0.30 to 3.35; P = 1.00) or nausea (OR = 1.24; 95% CI = 0.46 to 3.35; P = 0.68).
Conclusions
Pregabalin may be effective to alleviate the pain after thoracic surgery.
Similar content being viewed by others
Introduction
Thoracic surgery is recognized as one of the most painful surgeries [1,2,3,4,5]. These patients may suffer from obviously postoperative pain which may develop into chronic pain [6,7,8]. Postoperative pain after thoracic surgery is burning and stabbing, and it shares many features of neuropathic pain, because tissue damage causes hyperalgesia and allodynia due to the increased sensitization of dorsal horn neurons [9,10,11,12]. However, there are still lack of effective approaches to alleviate pain after thoracic surgery.
Pregabalin is one important drug to reduce the excitability of the dorsal horn neurons [13,14,15]. It was first introduced as one anticonvulsant and anxiolytic drug [16]. Interestingly, pregabalin has been successfully used to alleviate the neuropathic pain after knee, laparoscopic and spinal surgeries, and similar positive results are found for intercostal neuralgia in patients with post-thoracotomy pain [17, 18].
Several RCTs reported that pregabalin may have the capability to alleviate pain intensity after thoracic surgery, but the results were not well established [19,20,21]. Considering these inconsistent effects, we therefore conducted this meta-analysis to evaluate the effectiveness of pregabalin on postoperative pain for thoracic surgery.
Materials and methods
Study selection and data collection
This meta-analysis of previously studies did not need ethical approval or patient consent. It was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement and Cochrane Handbook for Systematic Reviews of Interventions [22, 23].
We have searched PubMed, EMbase, Web of science, EBSCO, and the Cochrane library up to March 2023, using the search terms “thoracic surgery” AND “pregabalin”. The inclusion criteria were as follows: (1) study design was RCT; (2) patients underwent thoracic surgery; (3) intervention treatments were pregabalin versus control intervention. Patients were excluded if they had severe cardiovascular or respiratory diseases, impaired hepatic or renal function, and history of chronic use of analgesics.
Quality assessment
The Jadad Scale was used to evaluate the methodological quality of individual RCT [24]. This scale consisted of three evaluation elements: randomization (0–2 points), blinding (0–2 points), dropouts and withdrawals (0–1 points). The score of Jadad Scale varied from 0 to 5 points. Jadad score ≤ 2 suggested low quality, while Jadad score ≥ 3 indicated high quality [25].
Outcome measures
The following information was extracted: first author, publication year, sample size, age, male, smoking and methods of two groups. The primary outcomes were pain scores at 0 h and pain scores at 24 h. Secondary outcomes included neuropathic pain, dizziness, headache and nausea.
Statistical analysis
A team consisting of three authors did the statistical analyses. Odd ratio (OR) with 95% confidence interval (CI) was applied to evaluate dichotomous outcomes, while mean difference (MD) with 95% CI was used to assess continuous outcomes. I2 statistic was applied to assess the heterogeneity, and significant heterogeneity was observed when I2 > 50% [26]. The random-effect model was used when encountering significant heterogeneity, and otherwise fixed-effect model was applied. We conducted the sensitivity analysis through detecting the influence of a single study on the overall estimate via omitting one study in turn or using the subgroup analysis. P ≤ 0.05 indicated statistical significance and Review Manager Version 5.3 was used in all statistical analyses.
Results
Literature search, study characteristics and quality assessment
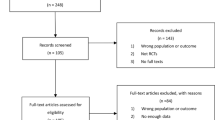
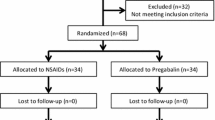
Figure 1 showed the flow chart for the selection process and detailed identification. 178 publications were searched after the initial search of databases. 53 duplicates and 117 papers after checking the titles/abstracts were excluded. Three studies were removed because of the study design and five RCTs were ultimately included in the meta-analysis [19,20,21, 27, 28].
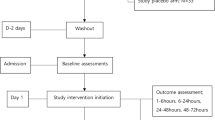
The baseline characteristics of five eligible RCTs were summarized in Table 1. The five studies were published between 2015 and 2019, and total sample size was 329. There were similar characteristics between pregabalin group and control group. Among the five RCTs, two studies reported pain scores at 0 h and pain scores at 24 h [20, 21], three studies reported neuropathic pain [19, 20, 28], three studies reported dizziness [20, 21, 28], two studies reported headache [20, 21] and three studies reported nausea [20, 21, 28]. Jadad scores of the five included studies ranged from 3 to 5, and all studies were considered to have high quality according to quality assessment.
Primary outcomes: pain scores at 0 h and pain scores at 24 h
The acute pain within 24 h after the thoracic surgery was crucial for patients’ recovery and satisfaction. There was no significant heterogeneity remained for the primary outcomes, and thus the fixed-effect model was used. Compared to control group for thoracic surgery, pregabalin was associated with significantly lower pain scores at 0 h (MD=-0.70; 95% CI=-1.10 to -0.30; P = 0.0005) with low heterogeneity among the studies (I2 = 19%, heterogeneity P = 0.27, Fig. 2) and pain scores at 24 h (MD=-0.47; 95% CI=-0.75 to -0.18; P = 0.001) with low heterogeneity among the studies (I2 = 26%, heterogeneity P = 0.24, Fig. 3).
Sensitivity analysis
There was low heterogeneity for the primary outcomes, and thus we did not perform the sensitivity analysis by omitting one study in turn.
Secondary outcomes
Pregabalin was also widely used to alleviate the neuropathic pain [13, 29, 30]. Compared with control intervention for thoracic surgery, pregabalin resulted in substantially reduced incidence of neuropathic pain (OR = 0.24; 95% CI = 0.12 to 0.47; P < 0.0001; Fig. 4), but showed no impact on dizziness (OR = 1.07; 95% CI = 0.15 to 7.46; P = 0.95; Fig. 5), headache (OR = 1.00; 95% CI = 0.30 to 3.35; P = 1.00; Fig. 6) or nausea (OR = 1.24; 95% CI = 0.46 to 3.35; P = 0.68; Fig. 7).
Discussion
Pain after thoracic surgery has become one common problem, and its prevalence has been reported to reach up to 80% [31]. In this meta-analysis, we included five RCTs and 329 patients undergoing thoracic surgery. The results confirmed that pregabalin was effective to significantly reduce pain scores at 0 h, pain scores at 24 h and neuropathic pain, but demonstrated no impact on the incidence of dizziness, headache, or nausea.
Our results confirmed the efficacy of pregabalin for pain control after thoracic surgery. Although there was no significant heterogeneity for the primary outcomes, several factors may result in some bias. Firstly, the doses and methods of pregabalin were not completely same, which may cause some heterogeneity. Secondly, the thoracic surgery may include different procedures, who may cause different levels of trauma and need different surgical time. Thirdly, different patients may have various response levels to pain stimulus.
Pregabalin is a γ-aminobutyric acid analogue that binds to α2-δ subunits of the voltage-gated calcium channels in the central nervous system [32]. As a first-line treatment for neuropathic pain conditions, perioperative use of pregabalin is able to prevent the development of pain via blocking presynaptic voltage-gated calcium channels implicated in central sensitization [33, 34]. Initiating analgesic treatment before tissue damage can reduce the hyperexcitability of dorsal horn neurons and central sensitization [35].
We should consider several limitations. Firstly, our analysis was based on only five RCTs and more studies with large patient samples should be conducted to confirm these findings. Secondly, the doses, administration timing and methods of pregabalin were different in the included studies, and may cause some bias. Thirdly, different operation procedures and experience of surgeons may produce various levels of trauma and need different surgical time, which may affect the pooling results.
Conclusion
Pregabalin may benefit to alleviate pain intensity after thoracic surgery, and more RCTs are needed to confirm this finding.
Data Availability
Not applicable.
References
Peng Z, Li H, Zhang C, Qian X, Feng Z, Zhu S. A retrospective study of chronic post-surgical pain following thoracic Surgery: prevalence, risk factors, incidence of neuropathic component, and impact on qualify of life. PLoS ONE. 2014;9(2):e90014.
Marshall K, McLaughlin K. Pain Management in thoracic Surgery. Torac Surg Clin. 2020;30(3):339–46.
van der Ploeg APT, Ayez N, Akkersdijk GP, van Rossem CC, de Rooij PD. Postoperative pain after lobectomy: robot-assisted, video-assisted and open thoracic Surgery. J Robotic Surg. 2020;14(1):131–6.
Brown LM, Kratz A, Verba S, Tancredi D, Clauw DJ, Palmieri T, Williams D. Pain and Opioid Use after thoracic Surgery: where we are and where we need to go. Ann Thorac Surg. 2020;109(6):1638–45.
de Cabo CMuñoz, Hermoso Alarza F, Cossio Rodriguez AM. Martín Delgado, Perioperative management in thoracic Surgery. Med Intensiva. 2020;44(3):185–91.
El-Hag-Aly MA, Nashy MR. Double edge closure: a novel technique for reducing post-thoracotomy pain. A randomized control study. Interact Cardiovasc Thorac Surg. 2015;21(5):630–5.
Garutti I, Cabañero A, Vicente R, Sánchez D, Granell M, Fraile CA, Real Navacerrada M, Novoa N, Sanchez-Pedrosa G, Congregado M, Gómez A, Miñana E, Piñeiro P, Cruz P, de la Gala F, Quero F, Huerta LJ, Rodríguez M, Jiménez E, Puente-Maestu L, Aragon S, Osorio-Salazar E, Sitges M, Lopez Maldonado MD, Rios FT, Morales JE, Callejas R, Gonzalez-Bardancas S, Botella S, Cortés M, Yepes MJ, Iranzo R, Sayas J. Recommendations of the Society of Thoracic Surgery and the Section of Cardiothoracic and Vascular Surgery of the Spanish Society of Anesthesia, Resuscitation and Pain Therapy, for patients undergoing lung surgery included in an intensified recovery program, Revista espanola de anestesiologia y reanimacion 69(4) (2022) 208–241.
Archer V, Cloutier Z, Park L, Briatico D, Walton JM. Intravenous acetaminophen for postoperative pain control after open abdominal and thoracic Surgery in pediatric patients: a systematic review and meta-analysis. Pediatr Surg Int. 2022;39(1):7.
Koehler RP, Keenan RJ. Management of postthoracotomy pain: acute and chronic. Torac Surg Clin. 2006;16(3):287–97.
Jack JM, McLellan E, Versyck B, Englesakis MF, Chin KJ. The role of serratus anterior plane and pectoral nerves blocks in cardiac Surgery, thoracic Surgery and trauma: a qualitative systematic review. Anaesthesia. 2020;75(10):1372–85.
Skelhorne-Gross G, Simone C, Gazala S, Zeldin RA, Safieddine N. A standardized minimal opioid prescription post-thoracic Surgery provides adequate Pain Control. Ann Thorac Surg. 2022;113(6):1901–10.
Guerra-Londono CE, Privorotskiy A, Cozowicz C, Hicklen RS, Memtsoudis SG, Mariano ER, Cata JP. Assessment of intercostal nerve Block Analgesia for thoracic Surgery: a systematic review and Meta-analysis. JAMA Netw open. 2021;4(11):e2133394.
Tesfaye S, Sloan G, Petrie J, White D, Bradburn M, Julious S, Rajbhandari S, Sharma S, Rayman G, Gouni R, Alam U, Cooper C, Loban A, Sutherland K, Glover R, Waterhouse S, Turton E, Horspool M, Gandhi R, Maguire D, Jude EB, Ahmed SH, Vas P, Hariman C, McDougall C, Devers M, Tsatlidis V, Johnson M, Rice ASC, Bouhassira D, Bennett DL, Selvarajah D. Comparison of Amitriptyline supplemented with Pregabalin, Pregabalin supplemented with Amitriptyline, and duloxetine supplemented with Pregabalin for the treatment of diabetic peripheral neuropathic pain (OPTION-DM): a multicentre, double-blind, randomised crossover trial. Lancet (London England). 2022;400(10353):680–90.
Wang XX, Dai J, Hu XG, Zhou AG, Pan DB. Oral Pregabalin in Cardiac Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, BioMed research international 2021 (2021) 8835891.
Robertson K, Marshman LAG, Plummer D, Downs E. Effect of Gabapentin vs Pregabalin on Pain Intensity in adults with chronic Sciatica: a Randomized Clinical Trial. JAMA Neurol. 2019;76(1):28–34.
Ogawa S, Satoh J, Arakawa A, Yoshiyama T, Suzuki M. Pregabalin treatment for peripheral neuropathic pain: a review of safety data from randomized controlled trials conducted in Japan and in the west. Drug Saf. 2012;35(10):793–806.
Zhang Y, He B, Zhao J, Zhang M, Ren Q, Zhang W, Xu S, Quan Z, Ou Y. Addition of Celebrex and Pregabalin to Ropivacaine for Posterior Spinal Surgery: A Randomized, Double-Blinded, Placebo-Controlled Trial, Drug design, development and therapy 15 (2021) 735–742.
Buvanendran A, Kroin JS, Della Valle CJ, Kari M, Moric M, Tuman KJ. Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: a prospective, randomized, controlled trial. Anesth Analg. 2010;110(1):199–207.
Homma T, Doki Y, Yamamoto Y, Ojima T, Shimada Y, Kitamura N, Akemoto Y, Hida Y, Yoshimura N. Efficacy of 50 mg Pregabalin for prevention of postoperative neuropathic pain after video-assisted thoracoscopic Surgery and thoracotomy: a 3-month prospective randomized controlled trial. J Thorac Disease. 2019;11(3):694–701.
Gaber S, Saleh E, Elshaikh S, Reyad R, Elramly M, Mourad I, Fattah MA. Role of Perioperative Pregabalin in the management of Acute and Chronic Post-thoracotomy Pain. Open Access Macedonian Journal of Medical Sciences. 2019;7(12):1974–8.
Kim JC, Byun S, Kim S, Lee SY, Lee JH, Ahn S. Effect of preoperative pregabalin as an adjunct to a multimodal analgesic regimen in video-assisted thoracoscopic Surgery: a randomized controlled trial. Medicine. 2017;96(49):e8644.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
HigginsJPT G. Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011], The cochrane collaboration (2011).
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in Meta-analyses. Ann Intern Med. 2001;135(11):982–9.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Miyazaki T, Sakai T, Sato S, Yamasaki N, Tsuchiya T, Matsumoto K, Kamohara R, Hatachi G, Doi R, Nagayasu T. Is early postoperative administration of pregabalin beneficial for patients with Lung cancer?-randomized control trial. J Thorac Disease. 2016;8(12):3572–9.
Yoshimura N, Iida H, Takenaka M, Tanabe K, Yamaguchi S, Kitoh K, Shirahashi K, Iwata H. Effect of Postoperative Administration of Pregabalin for Post-thoracotomy Pain: a randomized study. J Cardiothorac Vasc Anesth. 2015;29(6):1567–72.
Derry S, Bell RF, Straube S, Wiffen PJ, Aldington D, Moore RA. Pregabalin for neuropathic pain in adults, The Cochrane database of systematic reviews 1(1) (2019) Cd007076.
Onakpoya IJ, Thomas ET, Lee JJ, Goldacre B, Heneghan CJ. Benefits and harms of pregabalin in the management of neuropathic pain: a rapid review and meta-analysis of randomised clinical trials. BMJ open. 2019;9(1):e023600.
Gerner P. Postthoracotomy pain management problems, Anesthesiol Clin 26(2) (2008) 355 – 67, vii.
Mishriky BM, Waldron NH, Habib AS. Impact of Pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. Br J Anaesth. 2015;114(1):10–31.
Freynhagen R, Serpell M, Emir B, Whalen E, Parsons B, Clair A, Latymer M. A comprehensive drug safety evaluation of pregabalin in peripheral neuropathic pain. Pain Practice: The Official Journal of World Institute of Pain. 2015;15(1):47–57.
Brulotte V, Ruel MM, Lafontaine E, Chouinard P, Girard F. Impact of Pregabalin on the occurrence of postthoracotomy pain syndrome: a randomized trial. Reg Anesth Pain Med. 2015;40(3):262–9.
Bornemann-Cimenti H, Lederer AJ, Wejbora M, Michaeli K, Kern-Pirsch C, Archan S, Rumpold-Seitlinger G, Zigeuner R. Sandner-Kiesling, preoperative pregabalin administration significantly reduces postoperative opioid consumption and mechanical hyperalgesia after transperitoneal nephrectomy. Br J Anaesth. 2012;108(5):845–9.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ZL and YH wrote the main manuscript text and ZL prepared figures and table. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Declaration of conflict of interest
None.
Ethical approval
Not applicable.
Competing interests
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, L., Zhang, H. The efficacy of pregabalin for pain control after thoracic surgery: a meta-analysis. J Cardiothorac Surg 19, 4 (2024). https://doi.org/10.1186/s13019-023-02449-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02449-1