Abstract
Blunt aortic injury (BAI) as a result of thoracic trauma is a rare entity in the adult and pediatric population. The endovascular approach has been the preferred method of management over operative repair in adults. However, data on pediatrics is limited to case reports and case series with no long-term follow-up. There are no current guidelines for management in the pediatric population. We are reporting a successful repair of a traumatic thoracic aortic aneurysm in a 13 year old boy with covered stents, with a review of relevant literature.
Similar content being viewed by others
Introduction
Traumatic vascular injury in general and thoracic aortic injury in specific is relatively rare in children and adolescents compared to the adult population [1]. The mechanism of injury in such cases is most often blunt rather than penetrating trauma. Heckman et al. reports an incidence of < 1% for blunt traumatic aortic injury (BTAI) in the pediatric population using the data from US National Trauma Database [2]. A slightly higher incidence in the range of 1.5–2% is reported in adults [3]. The presence of such injury reflects on the severity of the mechanism and the possibility of other associated life-threatening injuries. Data from the National Pediatric Trauma Registry reports an overall mortality of 15% for children with blunt thoracic injury. The pediatric population is anatomically predisposed to thoracic injury. One of the reasons is the increased compliance of the chest wall due to incomplete rib ossification and a cartilaginous chest wall [4]. In addition, because of a relatively small volume to body surface area, children are at higher risk for injuries to multiple organs after blunt trauma [5,6,7].
The current society of vascular surgery classification grades aortic injury as minimal aortic injury (MAI) and significant aortic injury (SAI) based on the absence or presence of external aortic wall deformity, respectively [8]. MAI and SAI are further divided into four types ranging from Type I which is Intimal tear or flap to type IV which is open rupture. While there have been multiple studies evaluating the efficacy and success of conservative management of MAI, most of the cases of SAI have to undergo either endovascular or operative repair [9]. Below is a case report of a successful repair of traumatic thoracic aortic aneurysm in a 13 year old boy with covered stents, and a review of the literature for similar cases.
Case report
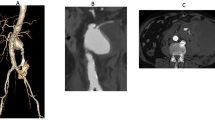
A previously healthy 13-year-old boy was brought to hospital following a motor vehicle accident. He was a front-seat passenger and was unrestrained. Speed at the time of impact was not known. At the time of presentation, he was alert and oriented with a Glascow-Coma Scale (GCS) of 15. Examination revealed a deep scalp laceration on the right side, tenderness over the right chest, left pelvic brim and restricted movement of the right arm and left leg. On X-ray imaging, the patient had multiple fractures including the right clavicle, the lower third of the sternum, the second to seventh ribs on the right, and the right sacral ala. Computed tomography (CT) showed an additional pulmonary contusion and low grade hepatic and splenic lacerations. There was a focal bulge of the anterior aspect of the distal aortic arch, with a thin periaortic hematoma, suggestive of a traumatic pseudoaneurysm. For further evaluation of the pseudoaneurysm, the patient underwent ECG gated CT Angiography. It demonstrated a saccular bulge suggesting pseudoaneurysm at the level of the aortic isthmus, measuring 1.1 long × 1.4 × 0.8 cm. The diameter of the aorta proximal to the aneurysm was 13 mm.There was no extra-luminal leakage of contrast to suggest rupture (Fig. 1). The rest of the thoracic aorta appeared unremarkable.
The patient’s initial management included fluid resuscitation, pain management and blood pressure control along with conservative management of other injuries. He was transferred afterwards to the pediatric tertiary care center. A multi-disciplinary team discussion involving pediatric surgery, vascular and cardiac surgery led to the decision to defer any acute treatments to allow for the recovery from associated injuries, and to attempt endovascular stenting after ensuring hemodynamic stability and that there is no ongoing blood loss. During this period, the patient was treated conservatively with blood pressure control and analgesics.
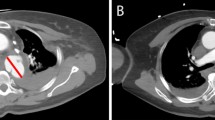
After a week of ICU care, the patient underwent endovascular aortic stenting. Access was obtained through the right femoral artery. Baseline aortogram showed the aneurysm of descending thoracic aorta distal to left subclavian artery (Fig. 2). A 39 mm long covered CP stent (cheathum platinum) from NuMED ® was placed at the site of the aneurysm using a 20 mm BiB balloon. An angiogram done afterwards still showed some flow through the pseudoaneurysm (Fig. 3). So, another covered stent 34 mm overlapping the first one was placed. There was no flow noted in the pseudoaneurysm in completion imaging. (Fig. 4).
The procedure was uneventful and there were no immediate complications. The patient was discharged 2 days after the procedure. He was lost to follow-up, and returned to clinic at 6 months, where he was found to have good blood pressure control and continues to be on aspirin. Follow up echo showed the stents to be in a good position and confirmed its patency. He is gradually being weaned off the anti-hypertensive medications. We have planned an additional follow-up in 1 year with echo.
Discussion
Blunt thoracic injury is one of the leading causes of death after motor vehicle accidents. Most of the patients having BTAI unfortunately die at the scene [10]. The treatment modality of aortic repair is often dictated by other associated injuries. Most of these patients have traditionally undergone a thoracotomy with or without an alternative perfusion pathway. They often require one lung ventilation if the associated injuries allow it. Historically, open repair has been associated with a high mortality rate reported at 28%, and spinal cord ischemia leading to paraplegia reported at 14% [11].
Thoracic endovascular repair for aortic injuries (TEVAR) is a relatively recent intervention that was approved by the FDA in 2005. This practice was very quickly adopted as an alternative method of management of BTAI. It involves placing an endovascular stent in the thoracic aorta at the location of injury from a remote access site under image guidance. Since its introduction there has been a consistent decline in the open surgery (OS).
Demetriades et al. compared TEVAR and OS after BTAI in adults [12]. In this prospective, observational multicenter study, 125 out of 193 patients examined had undergone TEVAR, with 68 of 193 having had OS. The patients in TEVAR group had significantly lower mortality (7.2% vs. 23.5 in OS group with OR of 8.42), blood transfusions (adjusted mean difference of 4.98 units) as well as procedure related paraplegia (0.8% vs. 2.9%) [12]. Stent related complications were reported in 20% of patients. The most common complication identified was endoleak, which was found in 18 cases (14.4%), 6 of which needed open repair. Other injuries included access vessel injuries (tear or thrombosis), occlusion of the left subclavian artery or left common carotid artery, stroke, paraplegia, and infection of the access site. Comparatively higher mortality and higher blood transfusion requirements were found in the OS group regardless of associated injuries [12].
In a landmark systematic review conducted by Murad et al., 139 studies were evaluated. Among the 7768 adult patients included, the mortality rate was lowest in those who underwent TEVAR (9%), followed by OS (19%) and highest in non-operative conservative treatment (46%) [13]. The risk of spinal cord ischemia, end stage renal disease, graft infection and systemic infections was higher with open repair compared to endovascular repair. Although, with endovascular repair an increased trend towards the need for a secondary procedure was seen [13].
The largest retrospective study in the pediatric population was done by Hasjim et al. in 2019 [14]. One-hundred and fifty nine patients with BTAI were identified over a period of 9 years (2007–2015). Of these, 124 (78.0%) underwent TEVAR and 35 (22.0%) underwent OS. Compared to patients undergoing OS, those with TEVAR had a shorter mean hospital length of stay (LOS) (16.4 vs. 21.4 days, p = 0.02) and ICU LOS (10.1 vs. 12.2 days, p = 0.01). There was no difference in the rates of mortality (5.5% vs. 8.6%, p = 0.56), or in in-hospital complications that included blood transfusions, acute kidney injury, pneumonia/ARDS, unplanned intubation, and cerebrovascular accident (p > 0.05) [14].
Our literature review yielded 23 other case reports of TEVAR for BTAI in the pediatric population. The majority of cases reported were for older children 8–17 years of age), with only one reported in a 16 month old child (See Table 1). The mortality rate was 13% (3/23), mostly attributed to associated injuries The mean follow up was 11 months (refer to Table 1).
The current guidelines in adult trauma by the society of vascular surgery (SVS) are based on the above mentioned review. The guideline suggests that endovascular repair of traumatic thoracic aortic injuries be performed preferentially over open surgical repair or nonoperative management, for grades II–IV. Non-operative management is recommended for Grade I [29]. This recommendation is based on very low quality evidence. There is unanimity of opinion that anatomic suitability is important for TEVAR but age should not be a factor in deciding the type of repair.
The use of TEVAR in pediatric BTAI is less established and is limited to case reports and case series. The anatomic challenge to the use of TEVAR is related to the small diameter of access vessels which may not accommodate the size of the delivery device. Currently no device has been approved by the FDA for traumatic aortic injury for the pediatric population, although off-label application of different endografts have been used.
According to SVC guidelines, TEVAR repair is best done within 24 h of injury if feasible, or at least prior to discharge (weak recommendation, low quality evidence) [29]. This was mainly based on adult literature. There is no such recommendation in children. In the case at hand, following a multidisciplinary discussion, we chose to delay the treatment for a weeks to allow for resolution and stabilization of associated injuries.
Given the rarity of the condition, there is very limited knowledge of the sequelae of endovascular management in this population. Long-term physiologic changes were depicted in a recent review of traumatic thoracic and abdominal injuries in otherwise healthy adults of age 45 ± 5.7 years [30]. These changes include increased aortic stiffness, blood pressure, cardiac mass, and aortic size after endovascular aortic repair in young patients suffering BTA [30]. The other concluded, however, that these effects might warrant close monitoring and management, but shouldn’t deter from choosing TEVAR over open repair. These effects might or might not be relevant in the younger pediatric patients. Some other potential long term concerns include stent occlusion, graft migration, pseudo-coarctation and durability of stent. Need for future open operative repair or upsizing of the stent also needs to be addressed. The incidence of these complications was not reported in pediatrics. The radiation burden and contrast related exposure is yet another concern in the younger population Therefore, long-term outcomes beyond 2 years have not been reported extensively. These are needed prior to establishing any recommendations in the pediatric age group.
Conclusion
The management of BTAI in the pediatric population is an ongoing discussion. Although there have been a significant number of studies done in adults to evaluate the role of endovascular approach to repair the aortic injury, its use in the pediatric population has been limited to case reports and cases series. This case and others from literature highlight the short term safety and efficacy of TEVAR in the management of BTAI. The benefits and risks need to be evaluated on a case to case basis taking into consideration the site of injury, size of the patient, and associated injuries. Further studies are needed to decide on the long term effects of stenting in a young age, especially the durability of grafts, patency and their effect on aorta in the pediatric age group.
References
Barmparas G, Inaba K, Talving P, David JS, Lam L, Plurad D, Green D, Demetriades D. Pediatric vs adult vascular trauma: a National Trauma Databank review. J Pediatr Surg. 2010;45(7):1404–12.
Heckman SR, Trooskin SZ, Burd RS. Risk factors for blunt thoracic aortic injury in children. J Pediatr Surg. 2005;40(1):98–102.
Fabian TC, Richardson JD, Croce MA, Smith JS, Rodman G, Kearney PA, Flynn W, Ney AL, Cone JB, Luchette FA, Wisner DH. Prospective study of blunt aortic injury: multicenter trial of the American Association for the Surgery of Trauma. J Trauma Acute Care Surg. 1997;42(3):374–83.
Saillant NN, Sein V. Management of severe chest wall trauma. J Emerg Crit Care Med. 2018;2:41–41.
Tripp HF, Robicsek F, Thomason M, Thubrikar M. Transected thoracic aorta: age-specific differences in incidence and possible reasons. Cardiovasc Surg. 1997;5(3):291–4.
Roach MR, Burton AC. The effect of age on the elasticity of human iliac arteries. Can J Biochem Physiol. 1959;37(4):557–70.
Schlatmann TJ, Becker AE. Histologic changes in the normal aging aorta: implications for dissecting aortic aneurysm. Am J Cardiol. 1977;39(1):13.
Heneghan RE, Aarabi S, Quiroga E, Gunn ML, Singh N, Starnes BW. Call for a new classification system and treatment strategy in blunt aortic injury. J Vasc Surg. 2016;64(1):171–6. https://doi.org/10.1016/j.jvs.2016.02.047.
Kapoor H, Lee JT, Orr NT, Nisiewicz MJ, Pawley BK, Zagurovskaya M. Minimal aortic injury: mechanisms, imaging manifestations, natural history, and management. Radiographics. 2020;40(7):1834–47.
Arthurs ZM, Starnes BW, Sohn VY, Singh N, Martin MJ, Andersen CA. Functional and survival outcomes in traumatic blunt thoracic aortic injuries: an analysis of the National Trauma Databank. J Vasc Surg. 2009;49(4):988–94.
Cowley RA, Turney SZ, Hankins JR, Rodriguez A, Attar S, Shankar BS. Rupture of thoracic aorta caused by blunt trauma: a fifteen-year experience. J Thorac Cardiovasc Surg. 1990;100(5):652–61.
Demetriades D, Velmahos GC, Scalea TM, Jurkovich GJ, Karmy-Jones R, Teixeira PG, Hemmila MR, O’Connor JV, McKenney MO, Moore FO, London J. Operative repair or endovascular stent graft in blunt traumatic thoracic aortic injuries: results of an American Association for the Surgery of Trauma Multicenter Study. J Trauma Acute Care Surg. 2008;64(3):561–71.
Murad MH, Rizvi AZ, Malgor R, Carey J, Alkatib AA, Erwin PJ, Lee WA, Fairman RM. Comparative effectiveness of the treatments for thoracic aortic transaction. J Vasc Surg. 2011;53(1):193–9.
Hasjim BJ, Grigorian A, Barrios C Jr, Schubl S, Nahmias J, Gabriel V, Spencer D, Donayre C. National trends of thoracic endovascular aortic repair versus open thoracic aortic repair in pediatric blunt thoracic aortic injury. Ann Vasc Surg. 2019;59:150–7.
Rousseau H, Soula P, Perreault P, Bui B, d’Othee BJ, Massabuau P, Meites G, Concina P, Mazerolles M, Joffre F, Otal P. Delayed treatment of traumatic rupture of the thoracic aorta with endoluminal covered stent. Circulation. 1999;99(4):498–504.
Karmy-Jones R, Hoffer E, Meissner M, et al. Management of traumatic rupture of the thoracic aorta in pediatric patients. Ann Thorac Surg. 2003;75:1513–7.
Wellons ED, Milner R, Solis M, et al. Stent-graft repair of traumatic thoracic aortic disruptions. J Vasc Surg. 2004;40:1095–100.
Milas ZL, Milner R, Chaikoff E, et al. Endograft stenting in the adolescent population for traumatic aortic injuries. J Pediatr Surg. 2006;41:e27–30.
Saad NEA, Pegoli W, Alfieris G. Endovascular repair of a traumatic aortic transection in a pediatric patient. J Vasc Interv Radiol. 2007;18:443–6.
Azizzadeh A, Keyhani K, Miller CC III, et al. Blunt traumatic aortic injury: initial experience with endovascular repair. J Vasc Surg. 2009;49:1403–8.
Gunabushanam V, Mishra N, Calderin J, et al. Endovascular stenting of blunt thoracic aortic injury in an 11-year-old. J Pediatr Surg. 2010;45:E15–8.
Goldstein BH, Hirsch R, Zussman ME, et al. Percutaneous balloon-expandable covered stent implantation for treatment of traumatic aortic injury in children and adolescents. Am J Cardiol. 2012;110:1541–5.
Hosn MA, Nicholson R, Turek J, Sharp WJ, Pascarella L. Endovascular treatment of a traumatic thoracic aortic injury in an eight-year old patient: case report and review of literature. Ann Vasc Surg. 2017;39:292-e1.
Gombert A, Barbati ME, Grommes J, Jalaie H, Schleimer K, Jacobs MJ, Kalder J. Blunt thoracic aortic injury in case of a 15-year-old boy: difficulties and possibilities of the endovascular approach. Ann Vasc Surg. 2016;33:228-e15.
Nicholas NW, Shaw DR, Puppala S. Pictorial review on the endovascular management of paediatric aortic injuries. Br J Radiol. 2020;93(1106):20190017.
Stahlschmidt CM, Von Bahten LC, Nicoluzzi JL, Corvello A, Stahlschmidt FL, Guimaraes F. Successful endovascular management of a traumatic aortic rupture in a pediatric patient: case report and literature review. Ulus Travma Acil Cerrahi Derg. 2010;16(1):84–6.
Deeney S, Bruny JL. Endovascular repair of traumatic aortic injury in a 16 month old. J Pediatr Surg Case Rep. 2015;3(12):551–3.
Stringel G, Xu ML, Erb M. Endovascular repair of blunt thoracic aortic injury. J Pediatr Surg Case Rep. 2018;30:52–5.
Lee WA, Matsumura JS, Mitchell RS, Farber MA, Greenberg RK, Azizzadeh A, Murad MH, Fairman RM. Endovascular repair of traumatic thoracic aortic injury: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 2011;53(1):187–92.
Spencer SM, Safcsak K, Smith CP, Cheatham ML, Bhullar IS. Nonoperative management rather than endovascular repair may be safe for grade II blunt traumatic aortic injuries: an 11-year retrospective analysis. J Trauma Acute Care Surg. 2018;84(1):133–8. https://doi.org/10.1097/TA.0000000000001630.
Funding
Open Access funding provided by the Qatar National Library. No funding received for this case report.
Author information
Authors and Affiliations
Contributions
All authors contributed to this manuscript during write up and literature review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
No interests to disclose of a financial or personal nature for any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Afzal, M., Abdulreda Najar, S., Baghazal, H. et al. Endovascular treatment of a traumatic thoracic pseudo-aneurysm in a pediatric patient: a case report with review of literature. J Cardiothorac Surg 18, 183 (2023). https://doi.org/10.1186/s13019-023-02265-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02265-7