Abstract
Background
We discuss a rare case of an adult patient with different pathologies involving the aortic and pulmonary valves in need of surgery.
Case presentation
The patient had a history of congenital PV stenosis and surgical valvuloplasty. Almost 50 years later the patient underwent a complex second heart surgery due to infective endocarditis of the aortic valve and high-grade restenosis of the pulmonary valve. Replacement of the aortic and pulmonary valve, as well as reconstruction of the RVOT and closure of a persistent foramen ovale, followed. Postoperative course was uneventful and the patient was discharged home a week after surgery.
Conclusion
Simultaneous surgery of pulmonary and aortic valves due to different pathologies is rare but can be performed successfully even in advanced age and can improve quality of life.
Similar content being viewed by others
Background
While aortic valve (AV) pathologies are mainly acquired, pulmonary valve (PV) pathologies are usually congenital.
However, simultaneous different diseases of the pulmonary and aortic valves in need of surgical treatment are uncommon. The only surgical procedure involving both of the above-mentioned valves is the Ross procedure in which the healthy autologous pulmonary valve is used to replace a diseased aortic valve in children. Even in this procedure only one of the valves is diseased. [1, 2]
We however present the surgical approach to a rare case of a patient with two different pathologies of these valves (aortic valve infective endocarditis (IE) and concomitant restenosis of the pulmonary valve).
Case presentation
A 67-year-old patient was admitted to the emergency department with fever, vertigo, palpitations and a progressive feeling of weakness. Echocardiography showed a vegetation on the right coronary cusp (RCC) 0.3 × 0.6 cm. Streptococcus sanguinis was isolated in blood cultures. According to the Duke criteria, the diagnosis of IE was made. A tooth was considered as a possible focus of the infection and extracted during the hospitalization. Antibiotics were administered according to guidelines.
In the following echocardiographic examinations, no changes regarding the size of the vegetation were seen. Additionally, a high-grade stenosis with a middle-grade insufficiency of the PV [flow acceleration over the PV to just under 5.7 m/s (Max PG 128 mmHg)] and a moderately dilated right ventricle with an impaired systolic function were seen. Noteworthy was the patient’s history of congenital PV stenosis and surgical valvuloplasty in the seventies. Right heart catheterization revealed severe PV stenosis with a calculated valve opening area of 0.25 cm2 (peak-to-peak pressure gradient of 106 mmHg and a mean pressure gradient of 75.8 mmHg). Pulmonary hypertension was ruled out. Relevant stenosis of the coronary arteries was ruled out through coronarography. The decision for surgical treatment was made primarily due to high-grade PV restenosis.
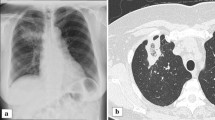
During the operation, severe adhesions as a consequence of pulmonary valve surgery in childhood were seen and detached. Following heparinization, the ascending aorta and both caval veins were cannulated. A vent catheter was inserted through the upper right pulmonary vein. Cooling of the patient to 34 °C followed. Two liters of Bretschneider solution were used for cardioplegia. Opening of the right atrium and direct closure of a persistent foramen ovale (5 × 5 mm) with subsequent closure of the right atrium followed. After aortotomy, multiple vegetations on the RCC were seen. The endocarditis-altered valve as well as a subvalvular membrane extending to the right and left coronary cusps were excised. A 21 mm CE Magna Ease valve was implanted and the aortotomy was closed. Next, following a longitudinal opening of the proximal pulmonary artery, the fibrotic altered valve with restricted mobility and a pronounced subvalvular hypertrophy with almost complete occlusion of the right ventricular outflow tract (RVOT) were seen. After a transannular extension to the right ventricle, of the initial longitudinal incision in the pulmonary artery, excision of the hypertrophied muscles and freeing of the cavity from trabecularized muscle parts followed. After sizing the RVOT using a 26 mm Hegar dilator, an 8 × 5 cm rhomboid Gore-Tex patch was sewn in with a continuous seam in the area of the RVOT. Insertion of 18 sutures into the pulmonary valve annulus and the Gore-Tex patch with anchoring of a 23 mm CE Magna Ease prosthesis with the Cor-Knot system followed. At last, completion of the transannular patch enlargement in the area of the pulmonary artery with a continuous suture was done (Fig. 1). Weaning from the cardiopulmonary bypass and postoperative course were uneventful.
Subsequent TTE showed a good function of both prostheses. The patient was discharged from the hospital on the seventh postoperative day and antibiotics were administered remotely. A control TTE three months later showed a good function of both prosthetic valves and an improvement in the function of the right ventricle.
Discussion
At the time of the patient’s first surgery in the seventies, balloon valvuloplasty was not yet available as a treatment option for PV stenosis. The first balloon valvuloplasty in humans was performed in 1982. Since then it has become the first choice of treatment in isolated valvular PV stenosis [3].
On the contrary pulmonary stenosis at different levels requires surgical treatment. Due to the necessity of early correction of congenital heart diseases, transannular patch plasty is more often performed in children. However, as described, it can be performed successfully even in adulthood, reducing heart load and improving quality of life. This technique can also be used in adults with infiltrative tumors of the right heart.
Even patients with corrected tetralogy of Fallot, in need of simultaneous reoperation on the aortic root and pulmonary valve are usually younger [4].
PV replacement with a homograft or biological valve is preferred due to a higher risk of thrombosis with mechanical valves on the PV position [5].
Follow-up studies have shown that while patients who have been treated for PV stenosis have a good outcome, 20% need a second intervention more than 20 years after the first one. Early treatment of patients with pulmonary stenosis has led to an increase in their life expectancy, it has also led to an increase in the number of patients who reach adulthood and need re-intervention [6]. Therefore, it is important to emphasize the need for regular check-ups to these patients, who consider themselves healed.
In our case, the patient did not have regular follow-ups after surgery and underwent a second intervention almost 50 years after the first one. A balloon valvuloplasty was not an option due to pulmonary stenosis at different levels as well as due to the coexistence of endocarditis of the aortic valve. Fetal endocarditis has been suggested as a possible etiology of pulmonary valve stenosis [2]. Studies show a possible genetic susceptibility to IE [7]. Moreau et al. showed a possible protective effect of SNPs on chromosome 3 against IE during Staph. aureus bacteremia [8]. Further studies on genetic susceptibility to endocarditis should be performed.
Conclusion
Simultaneous surgery of pulmonary and aortic valves due to different pathologies is rare but can be performed successfully even in elderly patients and can improve quality of life. This case can serve as an additional reminder of how important good communication is, to raise the patient's adherence to therapy.
Availability of data and materials
Not applicable.
References
Haas N, Kleideiter U. Kinderkardiologie; Klinik und Praxis der Herzerkrankungen bei Kindern, Jugendlichen und jungen Erwachsenen. Stuttgart: Thieme; 2018. p. 195–200.
Kliegman RM, St. Geme JN. Textbook of pediatrics, vol. 2. Philadelphia: Elsevier; 2019. p. 2384–7.
Buchanan J, Anderson J, White R. The 1st balloon valvuloplasty: an historical note. J Vet Intern Med. 2002;16:116–7.
Oechslin EN, Harrison DA, Harris L, Downar E, Webb GD, Siu SS, et al. Reoperation in adults with repair of tetralogy of fallot: indications and outcomes. J Thorac Cardiovasc Surg. 1999;118(2):245–51.
Cuypers JAAE, Witsenburg M, van der Linde D, et al. Pulmonary stenosis: update on diagnosis and therapeutic options. Heart. 2013;99:339.
Nielsen EA, Hjortdal VE. Surgically treated pulmonary stenosis: over 50 years of follow-up. Cardiol Young. 2016;26:860–6.
Weinstock M, Grimm I, Dreier J, et al. Genetic variants in genes of the inflammatory response in association with infective endocarditis. PLoS ONE. 2014;9:1–9.
Moreau K, Clemenceau A, Le Moing V, et al. Human genetic susceptibility to native valve staphylococcus aureus endocarditis in patients with S. aureus Bacteremia: genome-wide association study. Front Microbiol. 2018. https://doi.org/10.3389/fmicb.2018.00640.
Acknowledgements
Not applicable
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
EK wrote on the manuscript. GV; GS; performed surgery and wrote on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Available.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Korça, E., Veres, G. & Szabó, G. Case report: Aortic valve endocarditis and recurrent pulmonary valve stenosis. J Cardiothorac Surg 18, 89 (2023). https://doi.org/10.1186/s13019-023-02184-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02184-7