Abstract
Background
Concomitant tricuspid repair in MR surgery is indicated in patients with severa tricuspid regurgitation, however, concomitant repair in less-than-severe TR patients is still a matter of debate.
Methods
In December 2021, we systematically searched PubMed, Embase and Cochrane databases for randomised control trials (RCTs) comparing isolated MR surgery versus MR surgery with concomitant TR annuloplasty. Four studies were included, resulting in 651 patients (323 in the prophylactic tricuspid intervention group and 328 in the no tricuspid intervention group).
Results
Our meta-analysis showed a similar all-cause mortality and perioperative mortality for concomitant prophylactic tricuspid repair when compared with no tricuspid intervention (pooled odds ratio (OR), 0.54; 95% confidence interval (CI): 0.25–1.15, P = 0.11; I2 = 0% and pooled OR, 0.54; 95% CI: 0.25–1.15, P = 0.11; I2 = 0%, respectively) in patients undergoing MV surgery. despite a significantly lower TR progression (pooled OR, 0.06; 95% CI: 0.02–0.24, P < 0.01; I2 = 0%). Additionally, similar New York Heart Association (NYHA) classes III and IV were identified in both concomitant prophylactic tricuspid repair and no tricuspid intervention, despite a lower trend in the tricuspid intervention group (pooled OR, 0.63; 95% CI: 0.38–1.06, P = 0.08; I2 = 0%).
Conclusions
Our pooled analyses suggested that TV repair at the time of MV surgery in patients with moderate or less-than-moderate TR did not impact on perioperative or postoperative all-cause mortality, despite reducing TR severity and TR progression following the intervention.
Similar content being viewed by others
Background
Tricuspid regurgitation (TR) is a common condition and is observed in 0.55% of the general population: its prevalence increases with age and affects 4% of individuals over 75 years old [1]. A secondary aetiology represents the majority of cases and is associated with left-sided valvular or myocardial dysfunction. Secondary TR may also develop later after left-sided valve surgery [1]. Additionally, late reoperation for severe TR in patients with right heart failure is associated with high perioperative mortality [2, 3]. Therefore, a growing consensus suggests that severe TR should be addressed during index procedures, particularly in symptomatic patients [4]. These recommendations are largely based on observational data [5, 6].
The operative approach for less-than severe TR is widely debated. Mild or moderate TR, not corrected at the time of left-sided cardiac surgery, may progress in 25% of patients leading to poorer late survival and functional outcomes [5, 7]. Risk factors for TR progression include annular dilation measuring 40 mm or more in diameter on preoperative transthoracic echocardiography, right ventricular (RV) dysfunction and the presence of leaflet tethering, pulmonary hypertension, atrial fibrillation or transvalvular pacing or defibrillator leads [7,8,9].
Accordingly, wide variations exist for managing less-than-severe TR at the time of left-sided cardiac surgery: the frequency of tricuspid-valve (TV) repair at the time of mitral-valve surgery ranges from 5 to 75% [10].
In our systematic review and meta-analysis, we assessed the prognostic benefits and interventional risks associated with TV repair at the time of MV surgery in patients with moderate or less-than-moderate TR.
Methods
Study protocol and registration
This study was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Additional file 1: Table S2). The study was also registered in the International Prospective Register of Systematic Reviews database (CRD42022296613).
Study selection criteria/eligibility criteria
Only studies investigating adult populations (≥ 18 years old) with moderate TR or less than moderate TR with annulus dilation were included. Studies with secondary mitral regurgitation (MR), primary TV disease and endocarditis were excluded. We focused on trials that used placement of tricuspid annulus ring or suture-type annuloplasty (e.g., DeVega annuloplasty) techniques at the time of MV intervention. Partial annuloplasty techniques were excluded (e.g., Kay annuloplasty). We included randomised controlled trials (RCTs) with parallel-group designs and excluded single-arm studies. We also excluded all cohort and case–control studies, and the following: reviews, dissertations, theses, editorials, study protocol, clinical guidelines, commentaries and letters. Only studies that used medical therapies as comparators were included. Studies had to assess individual outcomes of all-cause mortality, perioperative mortality (30-day mortality post-surgery), reoperation for TR, TR progression by two grades and the presence of moderate-severe TR or patients with a New York Heart Association (NYHA) class III–IV condition.
Information sources and search strategy
The search strategy was devised by GC and JC. Bibliographic databases were systematically searched. RCTs on tricuspid repair in MV surgeries were extracted and merged with hits from the bibliographic database search. Electronic database searches were complemented by searching clinicaltrials.gov to capture results from ongoing or recently completed RCTs not yet published. We also scanned the reference lists of eligible studies to capture additional trial articles by cross-referencing. The search strategy is shown (Additional file 1: Table S2). We conducted searches in PubMed, Embase and Cochrane Central Register of Controlled Trials databases.
The search strategy included the following terms and all variants in multiple combinations in each database: "mitral valve repair," "mitral valve surgery," and "tricuspid insufficiency." Standard search terms for RCTs were also used wherever possible. No planned search restrictions in the search strategy were used to prevent overlooking important studies that were not correctly classified in the respective bibliographic databases. Databases were searched from database inception, without time restrictions. We also limited our searches to English language studies. Literature searches were updated during peer-review to include the most up to date literature.
Data collection and management
Study selection and data extraction were performed in duplicate by two reviewers. Both were blinded to each other’s decisions but not to journal titles, study authors, or institutions. Mendeley software was used to store, organise and manage references, and allow a transparent and reproducible systematic search. Both reviewers independently scanned study titles and abstracts against eligibility criteria. Full texts were acquired from studies meeting inclusion criteria. Reviewers’ results were compared and when disagreements occurred, critical points were discussed until a consensus was reached. If necessary, other study authors were asked to resolve eligibility issues. Reasons for excluding trials were fully documented. After eligible studies were selected, two reviewers independently extracted predefined data from the abstracts and full texts. Extracted items included first author, publication year, country, number of participants, sex, mean/median age, race/ethnicity, mean/median body mass index, echocardiographic mitral and tricuspid parameters, type of procedure and cardiovascular risk factors. If summary data were not published, they were calculated from study data.
Quality assessments
All planned statistical analyses were registered in PROSPERO before data collection to preclude data-driven analyses and the selective reporting of statistically significant findings. The study protocol was developed in line with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P), the Cochrane Handbook for Systematic Reviews of Interventions. We adhered to current PRISMA guidelines.
Descriptive and meta-analyses
Outcomes were addressed by estimating odds ratios (ORs) and 95% confidence intervals (CIs). Results of the intention-to treat (ITT) approach were used, including all patients randomised when both ITT and per-protocol results were provided. Effect estimates from eligible studies was assessed with random-effects model through the DerSimonian and Laird method (primary analysis). Heterogeneity was visually represented using forest plots and statistically assessed by Cochran’s Q test (significance level = 0.05) and the I2 index (< 25% low, 25–50% moderate and > 50% high heterogeneity). A meta-analysis was conducted even if high heterogeneity was detected, with results discussed within a heterogeneous context. Heterogeneous sources were explored using sensitivity analyses; we excluded studies with a high or unknown risk of bias according to the Cochrane RoB-2 assessment tool for randomised trials. The quality assessment for each study is presented in the “risk of bias summary” (Table 1) Publication bias was visually represented in funnel plots and tested using the Egger’s test (Additional file 1: Figures S1–S4). The certainty of the evidence was evaluated using the GRADE approach (Additional file 1: Table S3).
Results
Search results
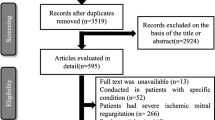
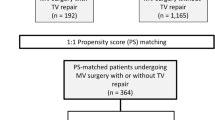
We identified 1209 articles from our literature search. After duplicate removal, we excluded 996 publications based on titles and abstracts, study type and study population assessments (Fig. 1). Four studies were finally included, resulting in 651 patients (323 in the prophylactic tricuspid intervention group and 328 in the no tricuspid intervention group). Study characteristics are described (Table 2) and patient baseline characteristics are outlined (Table 3).
Study outcomes
Overall, we identified a similar postoperative all-cause mortality for concomitant prophylactic tricuspid repair when compared with no tricuspid intervention (pooled OR, 0.54; 95% CI: 0.25–1.15, P = 0.11; I2 = 0%) (Fig. 2). In terms of perioperative mortality, no significant differences were observed (pooled OR, 0.54; 95% CI: 0.25–1.15, P = 0.11; I2 = 0%) (Fig. 3).
Additionally, we identified similar NYHA III–IV classes in both groups, despite a lower trend in the tricuspid intervention group (pooled OR, 0.63; 95% CI: 0.38–1.06, P = 0.08; I2 = 0%) (Fig. 4). We identified a significantly lower TR progression (pooled OR, 0.06; 95% CI: 0.02–0.24, P < 0.01; I2 = 0%) and postoperative moderate-severe TR (pooled OR, 0.23; 95% CI: 0.11–0.46, P < 0.01; I2 = 27%) (Fig. 5) in the group that underwent prophylactic tricuspid surgery.
Discussion
From our systematic review and meta-analyses, a TV repair at the time of MV surgery in patients with moderate or less-than-moderate TR did not impact perioperative or postoperative all-cause mortality. Moreover, we observed a significant reduction in TR severity and TR progression following an intervention. However, no significant improvement in the NYHA functional classification was observed.
Previous research reported that increasing TR grades were associated with an increased risk of death in non-surgical populations, regardless of pulmonary hypertension or ejection fraction [11], whereas isolated moderate or severe TR was associated with an increased risk of death, regardless of cardiovascular or comorbid conditions [12]. Additionally, untreated TR increased mortality risks in patients undergoing left-sided transcatheter valve procedures, with two-fold mortality risk increases in patients with significant untreated TR and severe aortic stenosis undergoing transcatheter aortic valve replacement [13], and moderate to severe TR, which independently predicted death and re-hospitalisation at 12 months in percutaneous mitral intervention patients [14]. Although it is unclear how TR decreases survival, it is most likely related to impaired RV function. Along with survival, it has been demonstrated that TR may have a detrimental effect on functional status, as untreated moderate or greater TR was a risk factor for worse midterm survival and a higher NYHA class in a propensity-matched analysis when compared with De Vega tricuspid repair [15]. Although the same effects of TR progression may be inferred in our study population, a short-term follow-up of approximately two years did not provide enough information on long-term mortality and morbidity effects of TR progression.
The analysis of the studies included did not allow for a comparison between different etiologies of TR, as only two of the studies compared TR in these different settings with one study including only degenerative disease. Previous studies have reported contrasting results in TR progression after MVR in some subgroups [16], particularly regarding degenerative disease with some studies failing to show a correlation between tricuspid annular dimensions and TR progression [17]. As such, care must be taken, in future research, to differentiate between these different pathological settings and avoid generalization in treatment indications.
Additional valvular procedures carry increased risk and operative mortality [18]. Nevertheless, our meta-analysis did not identify added morbidity or mortality in patients undergoing MV surgery and concomitant TV repair. This finding was supported by a Society of Thoracic Surgeons Adult Cardiac Surgery Database analysis, which showed no increase in risk-adjusted operative mortality for TV repair at all TR grades, suggesting concomitant tricuspid surgery may not confer added mortality risk [10]. Conversely, operative risks for patients requiring a subsequent reoperation for residual/recurrent TR remained as high as 35% [19]. Gammie et al. has planned to conduct a 5-year follow-up, which may delineate long-term clinical effects.
Dreyfus et al. concluded that remodelling TV annuloplasty based on tricuspid dilation improved functional status irrespective of the regurgitation grade. The authors intraoperatively measured the tricuspid annular diameter from the anteroseptal to the antero-posterior commissure. Patients with a tricuspid annular dimension ≥ 70 mm undergoing tricuspid annuloplasty had an improved functional status. However, a tricuspid annulus diameter ≥ 40 mm or > 21 mm/m2 was proposed as an alternative cut-off as this value accurately identified patients undergoing MV repair without concomitant TV annuloplasty and who had poor echocardiographic outcomes, including significant TR and a lack of RV reverse remodelling at follow-up [20].
In terms of adverse events, Gammie et al. reported a substantially higher rate of permanent pacemaker implantation [21]. TV annuloplasty was previously associated with higher rates of this pacemaker necessity [22], which were associated subsequently with device malfunction, thrombosis, infection, recurrent or progressive TR, RV remodelling and reduced survival risks [23]. However, no other selected study reported pacemaker implantation rates.
Study limitations
Some limitations were identified in our investigation. Firstly, only four studies were selected for analysis, however, these represent the totality of RCTs currently published on the subject, and the potential bias risk was considered accordingly. Secondly, we did not have access to individual patient data. Thirdly, heterogeneous TR-group inclusion criteria and several TV repair techniques were used in different studies; however, significant heterogeneity was not identified in our analyses. Fourthly, several studies did not report adverse events, especially pacemaker implantation rates, which should be factored into shared decision-making with patients. Lastly, the average follow-up period was 1–3.8 years, thus, we suggest that significant differences in functional status and mortality may be observed over a longer time-frame due to TR progression and consequent RV remodelling\failure.
Conclusions
Our pooled analyses suggested that a tricuspid-valve repair at the time of MV surgery in patients with moderate or less-than-moderate TR did not impact perioperative or all-cause mortality, despite reducing TR severity and TR progression following intervention. To the authors knowledge this is the first systematic review and meta-analysis performed on this subject.
Availability of data and materials
All data generated or analyzed during this study is included in this published article [and its Additional file 1].
Abbreviations
- ITT:
-
Intention-to-treat
- NYHA:
-
New York Association
- OR:
-
Odds Ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- RCTs:
-
Randomised Clinical Trials
- TR:
-
Tricuspid Regurgitation
- TV:
-
Tricuspid Valve
References
Topilsky Y, Maltais S, Medina Inojosa J, Oguz D, Michelena H, Maalouf J, et al. Burden of tricuspid regurgitation in patients diagnosed in the community setting. JACC Cardiovasc Imaging. 2019;12(3):433–42.
Pfannmüller B, Moz M, Misfeld M, Borger MA, Funkat AK, Garbade J, et al. Isolated tricuspid valve surgery in patients with previous cardiac surgery. J Thorac Cardiovasc Surg. 2013;146(4):841–7.
Jeganathan R, Armstrong S, Al-Alao B, David T. The risk and outcomes of reoperative tricuspid valve surgery. Ann Thorac Surg. 2013;95(1):119–24.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2021;7:411–6.
Van De Veire NR, Braun J, Delgado V, Versteegh MIM, Dion RA, Klautz RJM, et al. Tricuspid annuloplasty prevents right ventricular dilatation and progression of tricuspid regurgitation in patients with tricuspid annular dilatation undergoing mitral valve repair. J Thorac Cardiovasc Surg. 2011;141(6):1431–9.
Chikwe J, Itagaki S, Anyanwu A, Adams DH. Impact of concomitant tricuspid annuloplasty on tricuspid regurgitation, right ventricular function, and pulmonary artery hypertension after repair of mitral valve prolapse. J Am Coll Cardiol. 2015;65(18):1931–8.
Desai RR, Vargas Abello LM, Klein AL, Marwick TH, Krasuski RA, Ye Y, et al. Tricuspid regurgitation and right ventricular function after mitral valve surgery with or without concomitant tricuspid valve procedure. J Thorac Cardiovasc Surg. 2013;146(5):1126–32.
Bertrand PB, Koppers G, Verbrugge FH, Mullens W, Vandervoort P, Dion R, et al. Tricuspid annuloplasty concomitant with mitral valve surgery: effects on right ventricular remodeling. J Thorac Cardiovasc Surg. 2014;147(4):1256–64.
Benedetto U, Melina G, Angeloni E, Refice S, Roscitano A, Comito C, et al. Prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing mitral valve surgery. Circulation. 2012;143(3):632–8.
Badhwar V, Rankin JS, He M, Jacobs JP, Furnary AP, Fazzalari FL, et al. Performing concomitant tricuspid valve repair at the time of mitral valve operations is not associated with increased operative mortality. Ann Thorac Surg. 2017;103(2):587–93.
Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004;43(3):405–9.
Topilsky Y, Nkomo VT, Vatury O, Michelena HI, Letourneau T, Suri RM, et al. Clinical outcome of isolated tricuspid regurgitation. JACC Cardiovasc Imaging. 2014;7(12):1185–94.
Prasitlumkum N, Kewcharoen J, Kittipibul V, Angsubhakorn N, Tokavanich N, Vutthikraivit W, et al. Baseline significant tricuspid regurgitation increases risk of mortality in post transcatheter aortic valve replacement: systemic review and meta-analysis of multivariable adjusted observational studies. J Am Coll Cardiol. 2019;73(9):1198.
Ohno Y, Attizzani GF, Capodanno D, Cannata S, Dipasqua F, Immé S, et al. Association of tricuspid regurgitation with clinical and echocardiographic outcomes after percutaneous mitral valve repair with the MitraClip System: 30-day and 12-month follow-up from the GRASP Registry. Eur Hear J Cardiovasc Imaging. 2014;15(11):1246–55.
Calafiore AM, Gallina S, Iacò AL, Contini M, Bivona A, Gagliardi M, et al. Mitral valve surgery for functional mitral regurgitation: should moderate-or-more tricuspid regurgitation be treated? A propensity score analysis. Ann Thorac Surg. 2009;87(3):698–703.
David TE, David CM, Fan CPS, Manlhiot C. Tricuspid regurgitation is uncommon after mitral valve repair for degenerative diseases. J Thorac Cardiovasc Surg. 2017;154(1):110-22.e1. https://doi.org/10.1016/j.jtcvs.2016.12.046.
Sordelli C, Lancellotti P, Carlomagno G, Di Giannuario G, Alati E, De Bonis M, et al. Tricuspid annular size and regurgitation progression after surgical repair for degenerative mitral regurgitation. Am J Cardiol. 2016;118(3):424–31. https://doi.org/10.1016/j.amjcard.2016.05.014.
Rankin JS, Hammill BG, Ferguson TB, Glower DD, O’Brien SM, DeLong ER, et al. Determinants of operative mortality in valvular heart surgery. J Thorac Cardiovasc Surg. 2006;131(3):547–57.
Bernal JM, Morales D, Revuelta C, Llorca J, Gutiérrez-Morlote J, Revuelta JM. Reoperations after tricuspid valve repair. J Thorac Cardiovasc Surg. 2005;130(2):498–503.
Topilsky Y, Tribouilloy C, Michelena HI, Pislaru S, Mahoney DW, Enriquez-Sarano M. Pathophysiology of tricuspid regurgitation: quantitative Doppler echocardiographic assessment of respiratory dependence. Circulation. 2010;122(15):1505–13.
Gammie JS, Chu MWA, Falk V, Overbey JR, Moskowitz AJ, Gillinov M, et al. Concomitant tricuspid repair in patients with degenerative mitral regurgitation. N Engl J Med. 2021;386:1–13.
Dreyfus GD, Corbi PJ, Chan KMJ, Bahrami T. Secondary tricuspid regurgitation or dilatation: Which should be the criteria for surgical repair? Ann Thorac Surg. 2005;79(1):127–32.
Mar PL, Angus CR, Kabra R, Migliore CK, Goswami R, John LA, et al. Perioperative predictors of permanent pacing and long-term dependence following tricuspid valve surgery: a multicentre analysis. Europace. 2017;19(12):1988–93.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. All authors have contributed significantly to the content of the article according to ICMJE criteria.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Funnel Plots and Supplemental Tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cardoso, J.L., Ferraz Costa, G., Neves, F. et al. Tricuspid repair in mitral regurgitation surgery: a systematic review and meta-analysis. J Cardiothorac Surg 18, 76 (2023). https://doi.org/10.1186/s13019-023-02158-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02158-9