Abstract
Background
Azygos vein aneurysms (AVAs) are extremely rare. The majority of patients have no obvious clinical symptoms, so they are found by physical examination or by chance. There is limited clinical treatment experience that can be referred to, and there are no clear guidelines or research evidence standardizing the surgical and interventional therapy. Here, we report a patient with idiopathic AVA whose three-dimensional reconstruction of the tumor was completed before surgery. On the basis of three-dimensional reconstruction, single-port thoracoscopic resection of the AVA was successfully completed and reported for the first time. The previously reported cases are summarized to provide guidance for the diagnosis and treatment of patients with AVAs.
Case presentation
A 56-year-old man was transferred to our hospital due to “dysphagia”. The diagnosis of AVA was made after enhanced computed tomography, gastroscopy, fiberoptic bronchoscopy, and three-dimensional reconstruction. Congenital weakness or degenerative changes causes the vein walls to be extremely thin that the AVA had the risk of ruptur. Furthermore, the patient had symptoms of dysphagia, he received single-port thoracoscopic surgery. After the operation, his dysphagia disappeared. The postoperative pathology confirmed hemangioma. The patient was discharged 3 days after surgery without any complications.
Conclusions
AVAs are rare. Preoperative three-dimensional reconstruction can greatly help surgeons clarify the disease diagnosis, formulate the surgical plan, avoid damage to the surrounding vital organs, and reduce intraoperative bleeding. Thoracoscopic surgery to remove AVAs is difficult and has a high risk of bleeding, while more minimally invasive single-port thoracoscopic surgery is also safe and effective for the treatment of AVAs.
Similar content being viewed by others
Background
Azygos vein aneurysms (AVAs) are rare [1]. In radiologic studies, the normal diameter of the AV is defifined as no more than 1 cm [2]. Underlying causes of AVA formation that have been proposed include cardiac decompensation [3, 4], portal hypertension [4, 5], pregnancy [3], and compression of the SVC due to neoplasms [3, 5]. It may occur rupture, thromboembolism, mediastinal mass effects, and pulmonary artery hypertension with progressive gradual enlargement of the AVA [3]. Because most patients are asymptomatic, the diagnosis is mostly an incidental finding. The optimal management of AVAs remains uncertain, and there is no clear distinction of criteria indicating conservative and surgical or interventional therapy. Usually, surgical resection is required in cases of compression of adjacent structures, appearance of clinical symptoms, azygos vein (AV) thrombus formation in patients with oral anticoagulation, contraindication to oral anticoagulation, pulmonary embolism, and considerable increase in the diameter of an AVA [1]. Due to the high difficulty of thoracoscopic surgical resection and the risk of embolism migration. Most patients underwent thoracotomy to remove AVAs, and only a few cases reported successful thoracoscopic resection [1]. There is no report of single-port thoracoscopic resection of an AVA. On the basis of three-dimensional reconstruction, we report a case of single-port thoracoscopic-based management of an idiopathic AVA with symptoms of dysphagia. At the same time, we review the symptoms, diagnosis, and treatment of AVAs in the published literature.
Case report
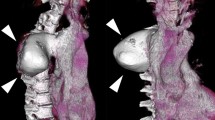
A 56-year-old man complained of dysphagia. He was referred to our hospital without special treatment because of a mediastinal mass on chest computed tomography (CT). The patient had no relevant medical history. He denied any falls or other trauma. Body temperature was 37.0 °C, heart rate was 78 beats/min, blood pressure was 127/74 mmHg, and respiratory rate was 20 breaths/min. Breath sounds were normal. No moist or dry rales. No heart murmurs or muffled heart tones. Contrast-enhanced CT revealed a mediastinal mass (4.2 × 3.7 × 2.6 cm) located at the tracheal bifurcation. It has smooth borders with no obvious nodules. No other aneurysmal malformations were detected. The esophagus was obviously compressed on the corresponding plane. At the same time, contrast-enhanced CT suggests unremarkable enhancement in the arterial phase. It showed delayed enhancement with a CT value of approximately 118 HU in the venous phase (Fig. 1A). Bronchoscopy revealed external pressure stenosis at the bronchial origin of the left lower lobe (Fig. 1B). Gastroscopy showed no obvious abnormalities. The initial diagnosis was hemangioma or bronchial cyst. Three-dimensional reconstruction showed that the mass was connected to the AV and superior vena cava. The mass body obviously extruded into the esophagus and trachea. There were two arteries from the aorta running among the mass body, the esophagus and the trachea (Fig. 1C, D). These findings revealed that the mass is considered to be initial diagnosed as a hemangioma originating from the azygos vein arch. Surgical resection should take care with the aortic branch behind the AVA to prevent uncontrollable bleed. At the same time, we need to protect the vagus nerve and the thoracic duct. Avoid damaging them to prevent gastrointestinal symptoms and chylothorax.
A Chest contrast-enhanced CT revealed that the mass located at the tracheal bifurcation. B Bronchoscopy revealed external pressure stenosis at the bronchial origin of the left lower lobe. C Three-dimensional reconstruction showed that the mass is a hemangioma originating from the azygos vein arch. There were two arteries from the aorta running among the tumor body, the esophagus and the trachea. D The tumor body obviously extruded the esophagus and trachea
Dysphagia caused by AVA extruded the esophagus and the left bronchus. Interventional treatment may can’t cure dysphagia symptom. In addition, interventional treatment may not prevent future migration and embolization of the thrombus. So, we chose single-port video-assisted thoracoscopic surgery (VATS) to respect the AVA under double-lumen tracheal intubation 3 days after hospitalization. The patient was in the left lateral decubitus position during surgery. The intraoperative exploration results were consistent with the three-dimensional reconstruction. The AVA was located in the azygos vein arch, and there was no abnormal pulmonary artery or pulmonary vein connected with it (Fig. 2A). The AVA obviously extruded into the esophagus and the left bronchus, and the AVA tightly adhered to the esophageal wall. We used an electrocoagulation hook and an ultrasonic scalpel to open the mediastinal pleura at the junction of the AVA and the superior vena cava, denuded the AV, and cut it off with an ultrasonic scalpel after hemolock clip was clamped. Then, the stump end was pulled to separate the tumor from the left main bronchus and esophagus wall. The ultrasonic scalpel and electrocoagulation hook were used to dissociate the surrounding tissue of the AVA. The aortic branches behind the tumor were carefully separated, the ultrasonic scalpel was cut off, and the venous aneurysm was completely removed (Fig. 2B). After the operation, a 16-F drainage tube was placed in the surgical incision (Fig. 2C). The operation lasted approximately 60 min, and intraoperative blood loss was 20 ml. The patient recovered well after surgery. All symptoms of dysphagia disappeared after the operation, and the patient was discharged 3 days after the operation. Histopathology showed that the venous layer to be affected is the media. Thinning of the AV wall and loss of the smooth muscle layer of the vascular wall. No malignant cells were seen. So it was considered an idiopathic AVA (Fig. 2D). At the 1-month follow-up, CT showed no recurrence.
A exploration revealed that the AVA was located in the azygos vein arch. B the venous aneurysm was completely removed. C A 16F drainage tube was placed in the surgical incision after single-port thoracoscopic surgery. D Histopathology showed thinning of the AV wall and loss of the smooth muscle layer of the vascular wall
Discussion
AVA is a rare disease. AVA is generally defined as a diameter of the AV exceeding 2.5 times the normal diameter. According to its morphology, it is currently divided into fusiform AVAs, with the overall expansion of the AV, and saccular AVAs, with local expansion of the azygos wall [3]. According to the etiology, it can be divided into (1) idiopathic AVA, (2) acquired AVA, and (3) traumatic AVA [1]. As far as we know, a total of 73 patients with AVAs have been reported in the available literature, who are summarized in Table 1 [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]. Among them, there were 29 males and 41 females. Their ages ranged from 3 months to 86 years (mean, 56.2 years), and their tumor diameters ranged from 1.2 to 15 cm (mean, 4.4 cm). There were 14 cases of fusiform AVAs and 32 cases of saccular AVAs. There were 54 cases of idiopathic AVAs and 6 cases of acquired AVAs. However, 3 patients' AVAs was accidentally discovered from trauma, and none were proven to be caused by trauma. Summarizing the previously reported cases, most of the patients were asymptomatic or had their AVA discovered incidentally on physical examination for other reasons. Among the common symptoms in patients, 13 patients had chest pain [12,13,14,15, 17, 18, 20, 22, 26, 35, 44, 48, 60], 10 patients had chest tightness and even dyspnea [3, 6, 19,20,21, 23, 25, 45], 4 patients had cough [3, 9, 43, 53], 3 patients had symptoms of dysphagia [19, 43, 59], and 3 patients' AVAs were accidentally discovered in trauma [3, 11]. Contrast-enhanced CT and magnetic resonance imaging (MRI) are the main noninvasive methods for the diagnosis of AVA. CT was completed in 72 patients of all reported 74 patients, and 22 patients completed MRI. Further completion of gastroscopy and fiberoptic bronchoscopy is an important supplement to CT and MRI when patients have symptoms such as dysphagia and dyspnea [6, 60]. However, poor tumor enhancement or intratumoral thrombus formation in the AVA may lead to misdiagnosis of AVA as a solid tumor or mediastinal lymphadenopathy [24]. When a mediastinal mass does not exclude the diagnosis of azygosmosis, needle biopsy is not recommended because of the risk of massive bleeding [25, 26]. In the present case, the three-dimensional reconstruction of the patient showed that the tumor was located in the AV, and the tumor was connected with the superior vena cava and the AV, which confirmed the diagnosis of AVA. At the same time, the three-dimensional reconstruction showed the surrounding tissues of the tumor. The tumor was closely related to the esophagus and airway. There were two arteries from the aorta running among the tumor body, the esophagus and trachea. During the operation, it was found that the tumor and esophagus were tightly adhered. When separating the posterior part of the tumor, we predict the location of arterial branches in advance. A combination of an ultrasonic scalpel and electrocoagulation hook was used to carefully separate the area of the aortic branch to avoid the risk of bleeding. Therefore, preoperative three-dimensional reconstruction plays an important role in the diagnosis of AVAs and the formulation of surgical plans [6, 8, 16, 33].
Currently, there are no guidelines on the optimal treatment of AVAs. In a previous report, conservative observation combined with oral anticoagulation was successful in asymptomatic AVA patients. Ko et al. [3] reported that only 2 of 10 patients with idiopathic AVAs underwent surgical resection immediately after diagnosis. Six patients underwent surgery due to thrombosis and tumor enlargement during follow-up. Patients should be re-evaluated regularly, and surgery or interventional therapy should strongly be considered in cases of compression of adjacent structures, appearance of clinical symptoms, thrombus formation in the aneurysm sac in patients with oral anticoagulation, contraindication to oral anticoagulation, pulmonary embolism, and considerable increase in the diameter of the AVA [1, 3, 18, 20]. In 21 of 72 patients, thoracotomy or thoracoscopic-assisted thoracotomy was performed to remove the AVA. With the advancement of endoscopic techniques, 19 of 72 patients were also reported to have AVAs removed by three-port or four-port thoracoscopic surgery, and 1 AVA was resected by robotic-assisted four-port endoscopy [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]. Single-port thoracoscopy causes less surgical trauma and pain. With the development of minimally invasive techniques, surgeon are increasingly selecting the single-port thoracoscope instead of the multi-port thoracoscope in thoracic surgery. We finally decided to select single-port thoracotomy AVA resection which had been no reports until this one. Although the single-port thoracoscope has less space to operate and more interference between operating instruments, the surgeon can overcome that through constant practice. The single-port thoracoscope also has its unique advantages. The single-port thoracoscope lens is in the same direction as the operator's vision. So the operation direction is in the same as the vision on the display that making the operation more accurate. However, the multi-port thoracoscope lens forms an angle with the operator's direction of operation. So there is a visual deviation between the direction of operation and the display, which may increase difficulty and the risk of bleeding for vascular operation. During the surgery, we avoided unnecessary clamping of the mass to prevent bleeding. The proximal end of the AVA was blocked first to prevent thrombus migration from causing pulmonary embolism. At the same time, the surgical plan was formulated based on preoperative three-dimensional reconstruction. We predict the location of arterial branches in advance, which further reduces the risks associated with surgery. Finally, the tumor was successfully resected safely under single-port thoracoscopic surgery. We have proved that single-port thoracoscopic surgery is safe and effective for the treatment of AVA.
At the same time, interventional therapy is a relatively new option for AVA. There are case reports of successful implantation of covered stents within the aneurysm [12, 14, 25, 35], transcatheter embolization of the aneurysms [7, 13] and Amplatzer closure occlusion of tumor blood vessels [35]. Although interventional treatment has less trauma than surgery. However, patients should be treated with surgery in case of excessive physiological curvature of the AV anticipates difficulty in passing the interventional guidewire, compression of adjacent structures, appearance of clinical symptoms, thrombus formation in the aneurysm sac in patients, severe pulmonary embolism requiring surgical intervention. We believe that the surgical resection, especially minimally invasive resection, is simpler and safer in patients with AVAs and therefore generally recommend earlier treatment even if there is no thrombus within the AVA [1, 29]. At the same time, embolization cannot prevent thrombus migration or tumor compression symptoms [13]. Moreover, the embolization device may aggravate compression symptoms after thrombosis.
Conclusion
In conclusion, some patients may have symptoms such as dysphagia and chest tightness due to tumor compression of the esophagus and trachea. Preoperative three-dimensional reconstruction greatly helps surgeons clarify the disease diagnoses, formulate surgical plans, avoid damage to the surrounding vital organs, and reduce intraoperative bleed. We proved that minimally invasive single-port thoracoscopic surgery is also safe and effective for the treatment of AVA.
Availability of data and materials
Not applicable.
Abbreviations
- AV:
-
Azygos vein
- AVA:
-
Azygos vein aneurysm
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- VATS:
-
Video-assisted thoracoscopic surgery
References
Kreibich M, Siepe M, Grohmann J, et al. Aneurysms of the azygos vein. J Vasc Surg Venous Lymphat Disord. 2017;5(4):576–86.
Kazerooni EA, Gross BH. Cardiopulmonary imaging. Lippincott Williams & Wilkins; 2004. p. 217–54.
Ko SF, Huang CC, Lin JW, et al. Imaging features and outcomes in 10 cases of idiopathic azygos vein aneurysm. Ann Thorac Surg. 2014;97(3):873–8.
Choo JY, Lee KY, Oh SJ, et al. Azygos vein aneurysm mimicking paratracheal mass: dynamic magnetic resonance imaging findings. Balkan Med J. 2013;30(1):111–5.
He J, Mao H, Li H, et al. A case of idiopathic azygos vein aneurysm and review of the literature. J Thorac Imaging. 2012;27:W91–3.
Briones-Claudett KH, Briones-Claudett MH, Posligua MA, et al. Azygos vein aneurysm with thrombosis and aspergillus fumigatus diagnosed using bronchoscopy: case report. Am J Case Rep. 2020;29(21):e923401.
Irurzun J, de Espana F, Arenas J, et al. Successful endovascular treatment of a large idiopathic azygos arch aneurysm. J Vasc Interv Radiol. 2008;19(8):1251–4.
Figueiredo F, Costa J, Lameiras R, Ramalho M. Spontaneous splenoazygos shunt in a patient with portal hypertension: an exceedingly rare occurrence. Rev Esp Enferm Dig. 2019;111(8):637–8.
Guo B, Guo D, Fu W, et al. A giant azygos venous aneurysm caused by the resection of hemangioma. J Vasc Surg Venous Lymphat Disord. 2014;2(3):328.
Ichiki Y, Hamatsu T, Suehiro T, et al. An idiopathic azygos vein aneurysm mimicking a mediastinal mass. Ann Thorac Surg. 2014;98(1):338–40.
Mohajeri G, Hekmatnia A, Ahrar H, et al. Azygos vein aneurysm as a posterior mediastinal mass discovered after minor chest trauma. Iran J Radiol. 2014;11(1):e7467.
DeMaio K, Kaushik S, Vadlamudi V. Endovascular treatment of traumatic azygous vein injuries: a case report. CVIR Endovasc. 2021;4(1):48.
Weber HS. Transcatheter occlusion of an azygous vein aneurysm. Catheter Cardiovasc Interv. 2010;77(1):99–102.
Favelier S, Estivalet L, Pottecher P, et al. Successful endovascular treatment of a large azygos vein aneurysm with stent-graft implantation. Ann Thorac Surg. 2015;99(4):1455.
Icard P, Fares E, Regnard JF, et al. Thrombosis of an idiopathic saccular azygos aneurysm. Eur J Cardiothorac Surg. 1999;15(6):870–2.
Tang F, Tan Y, Tang SJ, et al. A case report of azygos vein aneurysm. Chin J Thorac Cardiovasc Surg. 2011;27(4):196.
Du XJ, Xie H, Zhang Y, et al. Cystic aneurysm of the azygos vein-case series. Chin J Thorac Cardiovasc Surg. 2019;35(12):752–4.
Xie H, Yang F, Zhou S, et al. Cavernous hemangioma of azygos vein: a case report. Chin J Radiol. 2019;53(4):322–3.
Morton S, Grubic AD, Ayazi S, et al. Multifactorial dysphagia: azygos vein aneurysm (AVA) and esophagogastric junction outflow obstruction (EGJOO). Int J Surg Case Rep. 2021;83:106017.
Wang ZX, Yang LL, Xu ZN, et al. Surgical therapy for hemangioma of the azygos vein arch under thoracoscopy: a case report. World J Clin Cases. 2021;9(11):2655–61.
Choi J, Song J, Huh J, et al. Complicated azygos vein aneurysm in an infant presenting with acute pulmonary thromboembolism. Korean Circ J. 2016;46(2):264–7.
Takamori S, Oizumi H, Utsunomiya A, et al. Thoracoscopic removal of an azygos vein aneurysm with thrombus formation. Gen Thorac Cardiovasc Surg. 2021;69(9):1335–7.
Zhang YF, Liu XF, Wang RP, et al. Azygos venous arch tumor with atrial septal bulge and defect: a case report. Chin J Radiol. 2021;55(09):991–2.
Gomez MA, Delhommais A, Presicci PF, et al. Partial thrombosis of an idiopathic azygos vein aneurysm. Br J Radiol. 2004;77(916):342–3.
Rothman JM, Galindo A, Evans WN, et al. Exclusion of an azygos vein varix with a covered stent. JACC Case Rep. 2020;2(12):1911–6.
Go H, Takuro M, Tomohiro O, et al. Successful resection to treat idiopathic azygos vein aneurysm. Asian J Endosc Surg. 2018;11(4):392–4.
Kurihara C, Kiyoshima M, Asato Y, et al. Resection of an azygos vein aneurysm that formed a thrombus during a 6-year follow-up period. Ann Thorac Surg. 2012;94(3):1008–10.
Zhang C, Luo W, Ma L, et al. Venous hemangioma of the azygos arch. Eur J Cardiothorac Surg. 2007;32:669–70.
Ueda Y, Tokuno J, Shoji T, et al. An azygos vein aneurysm resected by video-assisted thoracic surgery after preoperative evaluation of multidetector computed tomography. Interact Cardiovasc Thorac Surg. 2014;18(1):135–6.
Lee DH, Keum DY, Park CK, et al. Azygos vein aneurysm: a case for elective resection by video-assisted thoracic surgery. Korean J Thorac Cardiovasc Surg. 2011;44(4):304–6.
Miura H, Miura J, Hirano H. Azygos vein varix mimicking bronchial cysts. Respirol Case Rep. 2018;6(7):e00353.
Guo DH, Zou M, Zhou Z, et al. Da Vinci robot assistance surgical coordination for the resection of azygous vein aneurysm: a case report. Chin J Prac Nurs. 2018;34(32):2517–9.
Hu H, Liu W, Tang J, et al. Aorto-azygous fistula complicated by arteriovenous aneurysm treated with video-assisted thoracic surgery. Ann Thorac Surg. 2015;99(5):e107–9.
Obeso A, Souilamas R. Unexpected intraoperative finding of azygos vein aneurysm mimicking a metastatic lymph node. Arch Bronconeumol. 2018;54(4):217.
Davis BS, Cretcher MR, Gover DD, et al. Arch of the azygos vein varix: a source of pulmonary emboli excluded with AMPLATZER plug occlusion. J Vasc Interv Radiol. 2017;28(2):186–7.
Suzuki Y, Kaji M, Hirose S, et al. Azygos vein aneurysm resection concomitant with heart valve repair via right thoracotomy. Interact Cardiovasc Thorac Surg. 2016;23(6):982–4.
Córdoba Rovira SM, Guedea Martin A, Salvador Adell I, et al. Saccular aneurysm of the azygos vein in a patient with azygos accessory fissure. Radiologia. 2015;57(2):167–70.
Seo HJ, Kang KW, Lee DS, et al. Evaluation of Azygous Vein Aneurysm Using Integrated PET/MRI. Nucl Med Mol Imaging. 2014;48(2):161–2.
Imori Y, Fujimoto H, Hanada S, et al. Idiopathic accessory hemiazygos vein aneurysm with an incidental mediastinal mass. Intern Med. 2012;51(17):2347–9.
Yang JY, Kim DH, Lee JH, et al. Evaluating a thrombosed azygous vein aneurysm combined with pulmonary arterial thromboembolism by ECG-gated multidetector CT: a case report. Korean J Radiol. 2011;12(6):754–6.
Ishikura H, Kimura S, Fukumura Y, et al. Resection of an azygos vein aneurysm with thrombosis. Gen Thorac Cardiovasc Surg. 2010;58(4):209–11.
Ichihara E, Kaneko M, Fujii H, et al. Azygos vein aneurysm occurring simultaneously with hemoptysis. Nihon Kokyuki Gakkai Zasshi. 2007;45(6):479–82.
Gnanamuthu BR, Tharion J. Azygos vein aneurysm: a case for elective resection. Heart Lung Circ. 2008;17(1):62–4.
Nakamura Y, Nakano K, Nakatani H, et al. Surgical exclusion of a thrombosed azygos vein aneurysm causing pulmonary embolism. J Thorac Cardiovasc Surg. 2007;133(3):834–5.
D’Souza ES, Williams DM, Deeb GM, et al. Resolution of large azygos vein aneurysm following stent-graft shunt placement in a patient with Ehlers-Danlos syndrome type IV. Cardiovasc Intervent Radiol. 2006;29(5):915–9.
Abad Santamaría N, García Díez JM, Pavón Fernández MJ, et al. Azygos vein aneurysm forming a mediastinal mass. Arch Bronconeumol. 2006;42(8):410–2.
Person TD, Komanapalli CB, Chaugle H, et al. Thoracoscopic approach to the resection of an azygos vein aneurysm. J Thorac Cardiovasc Surg. 2005;130(1):230–1.
Dilege S, Tanju S, Bayrak Y, et al. Posterior mediastinal lesion–aneurysm of azygos vein. Eur J Cardiothorac Surg. 2004;26(1):215–6.
Bobbio A, Miranda J, Gossot D, et al. Azygos vein aneurysm as a diagnostic pitfall: the role of thoracoscopy. Surg Endosc. 2001;15(9):1049–50.
Sakaguchi M, Hanazaki K, Nakamura T, et al. Idiopathic saccular aneurysm of the azygos vein. J Card Surg. 1999;14(3):178–80.
Gallego M, Mirapeix RM, Castañer E, et al. Idiopathic azygos vein aneurysm: a rare cause of mediastinal mass. Thorax. 1999;54(7):653–5.
Poll LW, Koch JA, Finken S, et al. Azygos continuation syndrome with aneurysm of the azygos vein: CT and MR appearances. J Comput Assist Tomogr. 1999;23(1):19–22.
Watanabe A, Kusajima K, Aisaka N, et al. Idiopathic saccular azygos vein aneurysm. Ann Thorac Surg. 1998;65(5):1459–61.
Mehta M, Towers M. Computed tomography appearance of idiopathic aneurysm of the azygos vein. Can Assoc Radiol J. 1996;47(4):288–90.
Léna H, Desrues B, Heresbach D, et al. Azygos vein aneurysm: contribution of transesophageal echography. Ann Thorac Surg. 1996;61(4):1253–5.
Kurihara Y, Nakajima Y, Ishikawa T. Case report: saccular aneurysm of the azygos vein simulating a paratracheal tumour. Clin Radiol. 1993;48(6):427–8.
Seebauer L, Präuer HW, Gmeinwieser J, et al. A mediastinal tumor simulated by a sacculated aneurysm of the azygos vein. Thorac Cardiovasc Surg. 1989;37(2):112–4.
Ikushima T, Ujiie H, Tsuneta S, et al. Presurgical assessment of flow variability in an azygos vein aneurysm using 4D-flow MRI. Gen Thorac Cardiovasc Surg. 2022. https://doi.org/10.1007/s11748-022-01813-7.
Bhojwani R, Jain N. Thoracoscopic oesophago-oesophagostomy in the prone position for oesophageal stenosis caused by dilated azygos vein in polysplenia-associated heterotaxy. J Minim Access Surg. 2021;17(3):395–8.
Savu C, Melinte A, Balescu I, et al. Azygos vein aneurysm mimicking a mediastinal mass. In Vivo. 2020;34(4):2135–40.
Zhou ZY, Shen HL, Du HD, et al. Idiopathic azygos vein aneurysm: a report of 2 cases and literature review. Anhui Med Pharm J. 2021;25(12):2463–5.
Zhang CX, Zhao S, Li XN, et al. A case report of thoracoscopic surgery for azygostomy. Chin J Gerontol. 2012;32(1):150–1.
Sun ZW, Liu GW, Wang SD, et al. Resection of an azygos vein aneurysm by video-assisted thoracic surgery. Chin J Thorac Cardiovasc Surg. 2017;33(1):55–55.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Participated in the care of the patient: YY, XX, GL, XL, JL. Performed the literature review and drafted the manuscript: YY, QH, YL, CL, YY, YW, and LL. Obtained the image data: YY, QH. Critical Review: JL, XX. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent for publication was obtained.
Competing interests
The authors have no competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yao, Y., Hu, Q., Xie, X. et al. Single-port thoracoscopic removal of an azygos vein aneurysm: a case report and literature review. J Cardiothorac Surg 18, 29 (2023). https://doi.org/10.1186/s13019-023-02143-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02143-2