Abstract
Background
Tobacco smoking has been associated with an increased risk of complications after conventional coronary surgery. However, the impact of smoking on the risk of postoperative complications in minimally invasive coronary surgery is yet to be studied. We aimed to analyze the impact of the preoperative smoking status on the short- and long-term outcomes of minimally invasive direct coronary artery bypass grafting (MIDCAB) in the context of isolated surgical revascularization or in association with percutaneous coronary intervention.
Methods
This was a retrospective observational study of all patients undergoing MIDCAB at our institution between 2006 and 2020. Patients were divided into three groups: active smokers, ex-smokers who have quit smoking for at least 1 month before surgery, and non-smokers. The groups were compared using conventional statistical methods. Multivariate analysis was then performed where significant differences were found to eliminate bias.
Results
Throughout the study period, 541 patients underwent MIDCAB, of which 135 (25%) were active smokers, 183 (34%) were ex-smokers, and 223 (41%) were non-smokers. Smokers presented for surgery at a younger age (p < 0.0001), more frequently with a history of myocardial infarction (p < 0.001), peripheral artery disease (p < 0.001) and chronic obstructive pulmonary disease (p < 0.0001). Using multivariate analysis, active smoking was determined to be a significant risk factor for the need of urgent revascularization (odds ratio 2.36 [1.00–5.56], p = 0.049) and the composite of pulmonary complications (including pneumothorax, respiratory infection, respiratory dysfunction, subcutaneous emphysema and exacerbation of chronic obstructive pulmonary disease; odds ratio 2.84 [1.64–4.94], p < 0.001). Preoperative smoking status did not influence the long-term survival (p = 0.83).
Conclusions
In our study, active smokers presented for MIDCAB at a younger age and more often with signs of atherosclerotic disease (history of myocardial infarction and peripheral artery disease). Active smoking was found to be the most significant risk factor for postoperative pulmonary complications, and is also associated with a more frequent need for urgent surgery at diagnosis. Long-term postoperative survival is not affected by the preoperative smoking status.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Surgical revascularization of the myocardium has been the standard of care in patients with severe coronary artery disease for decades. Coronary surgery has been influenced by the trend towards minimally invasive approaches while preserving excellent patient outcomes. Minimally invasive direct coronary artery bypass grafting (MIDCAB) provides off-pump surgical revascularization of the left anterior descending artery (LAD) with the use of left internal mammary artery graft (LIMA) through a left anterior short thoracotomy. It has kept its popularity throughout the last two decades owing to the lower risk of complications associated with the use of extracorporeal circulation, as well as to the added benefit of its minimally invasive and less traumatic surgical approach [1].
Among a wide scale of factors influencing the outcomes of coronary surgery, tobacco smoking plays an important role. The impact of the smoking status on the outcomes of conventional bypass surgery has been extensively researched, exhibiting an association with an increased risk of several postoperative complications, which include pulmonary and wound healing complications, in-hospital and long-term mortality, renal impairment, strokes, and a longer post-operative stay in the ICU [2,3,4,5,6], Arabaci et al. [6] was able to prove better pulmonary functions in non-smokers post-operatively compared to smokers. Furthermore, evidence suggests that preoperative smoking cessation at least one month before coronary surgery is also associated with better post-operative outcomes [7]. These include a lesser need for inotropic support postoperatively, and a lower rate of pulmonary, neurological, and wound healing complications [8, 9]. However, none of the previous studies have assessed this in the setting of minimally invasive coronary surgery. Therefore, we aimed to analyze the impact of smoking status on the short- and long-term postoperative outcomes in patients undergoing MIDCAB at our institution.
Methods
This was a retrospective observational cohort study of all patients undergoing MIDCAB at our institution between 2006 and 2020. The perioperative data were collected from patient in-hospital records and manually entered into tables. Long-term data on mortality were provided by the Institute of Health Information and Statistics of the Czech Republic, which is an official institution of the Czech Ministry of Health. The closing date for long-term survival analysis was 30th of December 2020. While the observed long-term outcomes were taken only from the compulsory national registry, we considered the long-term follow-up 100% complete.
Patients were divided into three groups: non-smokers, ex-smokers and smokers. Non-smokers were the patients who had never smoked on a regular basis. Ex-smokers had stopped smoking at least one month prior to surgery. Smokers were the patients who were actively smoking until the surgery or had stopped smoking less than one month prior. The groups were afterwards compared in terms of preoperative cohort characteristics, perioperative outcomes and long-term survival rates.
Pulmonary complications were analysed separately as well as a composite outcome including pneumothorax, respiratory infection, respiratory dysfunction (defined as hypoxemia in arterial blood gas analyses), subcutaneous emphysema and exacerbation of chronic obstructive pulmonary disease (COPD). Urgent surgery was defined in accordance with EuroSCORE II as a case where the patient was either not electively admitted for surgery, required an intervention or surgery at the time of admission, or could not be sent home for medical reasons [10]. Hybrid revascularization was defined as a combined approach in the treatment of multi-vessel coronary disease composed of surgical revascularization of LAD, and percutaneous intervention of other affected coronary vessels, regardless of the timing. However, in certain cases where PCI was not feasible for the other affected coronary vessels, palliative revascularization of the LAD using isolated MIDCAB was performed.
Surgical technique
Patients were prepared in a supine position. The left chest was elevated approximately to an angle of 20 to 30 degrees. Induction of general anaesthesia was performed conventionally. A double-lumen endotracheal intubation or blocker was routinely used to maintain a single-lung ventilation. The skin incision was eight to twelve centimetres long and was located along the fourth or fifth intercostal space (in men under the left nipple and in women in the skin fold under the left breast). LIMA was harvested under direct vision. The anastomosis of LIMA to LAD was constructed on the beating heart using standard off-pump techniques [11]. Chest drainage was introduced and the thoracotomy was closed.
Statistical analysis
All the calculations were conducted through NCSS 2019 Statistical Software (2019, Kaysville, Utah, USA). The presented data are shown as categorical or continuous variables. The categorical variables are expressed as numbers and percentages. The continuous data are expressed as medians and interquartile ranges as long as we were unable to prove normal value distribution in most of the variables. The influence of smoking status on the outcomes was tested by Pearson’s Chi-square test for categorical variables, and Kruskal–Wallis nonparametric analysis of variance with post-hoc Dunn‘s test with Bonferroni modification for continuous variables. In all performed tests, a p value of ≤ 0.05 was considered statistically significant.
In statistically significant results, we afterwards performed a multivariate analysis in order to clarify the influence of smoking status on our findings and to detect confounding variables. We utilized the multiple regression analysis for continuous variables and the logistic regression for categorical data. The comparisons were primarily adjusted for all preoperative variables, thereafter the algorithm provided a reduced model with a limited number of input covariates with the best predictability. Hereby the models with the highest predictability are presented. The quality of statistical models was assessed by the coefficient of determination (Model R2) and p value of the analysis of deviance.
In the ex-smokers group, we attempted to find a potential cut-off time interval before surgery for smoking cessation to achieve its maximum benefit, with respect to the prevalence of the composite of postoperative pulmonary complications. The group was further divided into two subgroups based on the interval between smoking cessation and surgery and compared. The analyses were performed for the cut-off values of 6, 12, 24, 36, 60, 120, 180 and 240 months interval.
The long-term all-cause postoperative mortality and the composite of cardiac and cerebrovascular mortality were tested by Kaplan–Meier analysis and compared by the log-rank test. The potential influence of preoperative covariates on the long-term all-cause mortality was assessed by the multivariate Cox proportional hazard analysis. Primarily, all preoperative covariates were included in the model and, thereafter, a reduced model with selected number of covariates with the best predictability was provided.
Results
Throughout the study period, 541 patients underwent MIDCAB at our institution. The cohort included 135 (25%) active smokers, 183 (34%) ex-smokers and 223 (41%) non-smokers. The study groups differed in several preoperative covariates (see Table 1). The smokers presented for surgery at younger age, more frequently with a history of myocardial infarction, peripheral artery disease, and COPD. They had the lowest level of creatinine and EuroSCORE II value, and they were found to be least symptomatic with regard to chest pains. The smallest proportion of females was found in the smokers group. The ex-smokers presented also very often with a history of myocardial infarction and peripheral artery disease. They had the highest prevalence of previous percutaneous coronary intervention and had the highest prevalence of diabetes of the three groups. Non-smokers had the smallest body surface area and the highest ejection fraction of the left ventricle.
Smokers had the highest incidence of indications for urgent revascularization. Subcutaneous emphysema, exacerbation of COPD, and the composite of pulmonary complications were mostly seen in the smokers group. On the margin of statistical significance, we observed also higher incidence of pneumothorax, respiratory dysfunction, and neurological complications in this group. Ex-smokers underwent MIDCAB as a part of a hybrid procedure most frequently. Non-smokers had the longest hospital stay and the highest incidence of wound healing complications. Only four patients died in the short-term postoperatively, which did not provide enough substrate for further statistical evaluation of this outcome. For the complete list of perioperative outcomes see Table 2.
According to the multivariate logistic regression, active smoking was determined to be a risk factor for the need of urgent revascularization (see Fig. 1) together with the history of myocardial infarction, chest pain at rest, and treated dyslipidemia (as a protective factor). Active smoking was the most significant risk factor for the composite of postoperative pulmonary complications, followed by COPD and body mass index (see Fig. 2). A similar trend was observed with the incidence of subcutaneous emphysema, where the significant risk factors were active smoking and the presence of COPD (see Additional file 1: Figure S1). Subcutaneous emphysema was in some cases concurrent with pneumothorax but often independent of other pulmonary pathologies. Ex-smokers were no longer associated with a significantly higher risk of the abovementioned complications. We were unable to define a cut-off interval before surgery for the best benefit of preoperative smoking cessation with regard to the prevalence of the composite of postoperative pulmonary complications (see Additional file 1: Table S1). Hybrid treatment (p = 0.08), the length of hospital stay (p = 0.58), and the risk of wound healing complications (p = 0.17) were not influenced by the active smoking but by other preoperative covariates (see Additional file 1: Figs. S2–4).
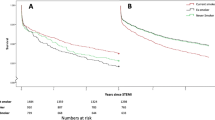
Over the median follow-up of five years (up to 15 years), the all-cause postoperative mortality (see Fig. 3), as well as the composite of cardiac and cerebrovascular mortality only (p = 0.44, see Additional file 1: Figs. S5–6) were comparable among the study groups. The preoperative smoking status did not have any influence on the postoperative mortality in the long-term. This was rather influenced by the patient’s age, the systolic function of the left ventricle, the severity of coronary artery disease and other covariates (see Fig. 4).
Multivariate Cox regression analysis for the long-term all-cause postoperative survival. Model R2 = 0.2811; Analysis of deviance for the whole model—p < 0.0001. CI: confidence interval; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association classification of dyspnea; PAD: peripheral artery disease
Discussion
Despite the abundant evidence in the pertinent literature on the impact of tobacco smoking on the short- and long-term outcomes of bypass surgery, studies regarding the outcomes of MIDCAB are lacking. In our retrospective study we found active smokers to present for MIDCAB at a younger age compared to non-smokers and ex-smokers. This coincides with the findings from previous studies performed on standard CABG [8, 12, 13]. Similarly to Al-Sarraf et al. [8], we also found that smokers were more likely to present for an urgent revascularization. Hypothetically, the long-term active smoking could lead to an accelerated formation of unstable atherosclerotic coronary plaques, consequently causing an acute coronary syndrome. As we expected, active smokers presented most frequently with a history of an atherosclerotic disorder (represented by peripheral arterial disease and myocardial infarction) in concordance with other studies [8, 12]. This may be attributed to the underlying pathomechanisms leading to accelerated atherosclerosis and hypertension [14,15,16] in smokers. Our multi-variate analysis yielded that treated hyperlipidemia was an independent protective factor against the need for an urgent revascularization. This corresponds to the findings of a previous study by Ji et al. [12] where treated hyperlipidemia was an independent protective factor against the need for an urgent revascularization. It might be due to the fact that an early diagnosed and treated hyperlipidemia reduces the risk of development of an acute coronary syndrome, as shown also by Alpe et al. [17] who studied the effect of preoperative administration of statins on cardiac surgery.
Our multi-variate analysis found active smokers to have the highest rate of post-operative pulmonary complications. This association was not found in ex-smokers which chimes with other studies [12, 13, 18,19,20]. It may be attributed to the ciliary dysfunction that arises in chronic smokers [21, 22]. Although we were unable to identify a cut-off time interval before surgery for smoking cessation to achieve its maximum benefit, Warner et al. [18] found that ex-smokers with a smoking cessation period greater than 6 months had a similar rate of postoperative pulmonary complications to non-smokers, and recommended a minimum period of 8 weeks of smoking cessation before undergoing coronary surgery to maximize the possible benefit. Other studies suggest that smoking cessation as early as possible regardless of the interval prior to surgery should be strongly recommended [7]. This is supported by the evidence that suggests a substantial microscopic enhancement in lung functions only weeks after smoking cessation and complete recovery after 6 months [23].
Although statistically insignificant, we found that non-smokers had that highest rate of conversions to sternotomies. However, this was not associated with the smoking status but was rather of a technical nature. Of the total 14 conversions accounted for in our study, 7 were due to injury of the LIMA during harvesting, 5 were due to suboptimal patient anatomy (extreme obesity; LIMA or LAD inaccessible through a thoracotomy), and 2 were due to injury to the right ventricle during the procedure.
Nonsmokers were most frequently associated with wound healing complications. However, this relationship was not found to be valid after the multivariate analysis. This was rather caused by the highest proportion of female patients being in the non-smokers group, as supported by previous evidence [24].
We did not find a correlation between the smoking status and the long-term post-operative mortality, accounting for either the all-cause mortality or only the composite of cardiac and cerebrovascular mortality. This is in contrast to other studies which found an increased rate of all-cause mortality in smokers, mainly attributable to cardiovascular causes [21]. He et al. [25] previously described even an increased 30-day and in-hospital post-operative mortality in smokers after cardiac surgery. This absence of mortality difference in our cohort might be due to constant improvement in perioperative care and reduction of mortality from respiratory causes. Our multivariate analysis yielded a few independent risk factors for long-term mortality, which included age, severe coronary artery disease, reduced ejection fraction, severity of heart failure and peripheral artery disease, similarly to another study performed by Domburg et al. [20]
Limitations
This study was a retrospective observational trial, which may influence its generalizability. A low perioperative mortality rate did not allow us to further elaborate on this topic. This study focused on the early clinical outcomes and the long-term survival. We were unable to investigate the long-term risk of coronary re-interventions as we did not have access to these data for General Data Protection Regulation (GDPR) reasons. We did not have the information on the eventual postoperative smoking cessation that could also influence the long-term outcomes.
Conclusions
Active smokers represent a specific cohort of patients undergoing coronary surgery. They present for MIDCAB at a younger age and with a more advanced atherosclerotic disorder. Tobacco smoking is associated with a greater need for an urgent surgery and is also the most significant risk factor for postoperative pulmonary complications. Long-term postoperative survival was not affected by the preoperative smoking status in our study, but was rather influenced by the patient’s age, left ventricular ejection fraction, severity of coronary artery disease and heart failure, and by the presence of peripheral artery disease.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Long-term data on mortality were provided by the Institute of Health Information and Statistics of the Czech Republic (https://www.uzis.cz/), which is an official institution of the Czech Ministry of Health.
Abbreviations
- MIDCAB:
-
Minimally invasive direct coronary artery bypass grafting
- LAD:
-
Left anterior descending artery
- LIMA:
-
Left internal mammary artery graft
- COPD:
-
Chronic obstructive pulmonary disease
References
Calafiore AM, Giammarco GD, Teodori G, Bosco G, D’Annunzio E, Barsotti A, et al. Left anterior descending coronary artery grafting via left anterior small thoracotomy without cardiopulmonary bypass. Ann Thorac Surg. 1996;61(6):1658–63 (discussion 1664-1665).
Ji Q, Zhao H, Mei Y, Shi Y, Ma R, Ding W. Impact of smoking on early clinical outcomes in patients undergoing coronary artery bypass grafting surgery. J Cardiothorac Surg. 2015;6(10):16.
Jones R, Nyawo B, Jamieson S, Clark S. Current smoking predicts increased operative mortality and morbidity after cardiac surgery in the elderly. Interact Cardiovasc Thorac Surg. 2011;12(3):449–53.
Sharif-Kashani B, Shahabi P, Mandegar MH, Saliminejad L, Bikdeli B, Behzadnia N, et al. Smoking and wound complications after coronary artery bypass grafting. J Surg Res. 2016;200(2):743–8.
Balachandran S, Lee A, Denehy L, Lin KY, Royse A, Royse C, et al. Risk factors for sternal complications after cardiac operations: a systematic review. Ann Thorac Surg. 2016;102(6):2109–17.
Arabaci U, Akdur H, Yiğit Z. Effects of smoking on pulmonary functions and arterial blood gases following coronary artery surgery in Turkish patients. Jpn Heart J. 2003;44(1):61–72.
Sepehripour AH, Lo TT, McCormack DJ, Shipolini AR. Is there benefit in smoking cessation prior to cardiac surgery? Interact Cardiovasc Thorac Surg. 2012;15(4):726–32.
Al-Sarraf N, Thalib L, Hughes A, Tolan M, Young V, McGovern E. Effect of smoking on short-term outcome of patients undergoing coronary artery bypass surgery. Ann Thorac Surg. 2008;86(2):517–23.
Ngaage DL, Martins E, Orkell E, Griffin S, Cale ARJ, Cowen ME, et al. The impact of the duration of mechanical ventilation on the respiratory outcome in smokers undergoing cardiac surgery. Cardiovasc Surg Lond Engl. 2002;10(4):345–50.
Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio Thorac Surg. 1999;15(6):816–22 (discussion 822-823).
Mastering Off-Pump. Total Arterial Coronary Artery Bypass Grafting: A step-by-step approach. [Internet]. [cited 2021 Dec 11]. Available from: https://scholar.google.com/citations?view_op=view_citation&hl=it&user=HQqpPVgAAAAJ&citation_for_view=HQqpPVgAAAAJ:Tyk-4Ss8FVUC
Ji Q, Zhao H, Mei Y, Shi Y, Ma R, Ding W. Impact of smoking on early clinical outcomes in patients undergoing coronary artery bypass grafting surgery. J Cardiothorac Surg. 2015;10:1–7.
Benedetto U, Albanese A, Kattach H, Ruggiero D, De Robertis F, Amrani M, et al. Smoking cessation before coronary artery bypass grafting improves operative outcomes. J Thorac Cardiovasc Surg. 2014;148(2):468–74.
Howard G, Wagenknecht LE, Burke GL, Diez-Roux A, Evans GW, McGovern P, et al. Cigarette smoking and progression of atherosclerosis: the Atherosclerosis Risk in Communities (ARIC) study. JAMA. 1998;279(2):119–24.
Dochi M, Sakata K, Oishi M, Tanaka K, Kobayashi E, Suwazono Y. Smoking as an independent risk factor for hypertension: a 14-year longitudinal study in male Japanese workers. Tohoku J Exp Med. 2009;217(1):37–43.
Gu L, Pandey V, Geenen DL, Chowdhury SAK, Piano MR. Cigarette smoke-induced left ventricular remodelling is associated with activation of mitogen-activated protein kinases. Eur J Heart Fail. 2008;10(11):1057–64.
Howard-Alpe G, Foex P, Biccard B. Cardiovascular protection by anti-inflammatory statin therapy. Best Pract Res Clin Anaesthesiol. 2008;1(22):111–33.
Warner MA, Offord KP, Warner ME, Lennon RL, Conover MA, Jansson-Schumacher U. Role of preoperative cessation of smoking and other factors in postoperative pulmonary complications: a blinded prospective study of coronary artery bypass patients. Mayo Clin Proc. 1989;64(6):609–16.
Bayfield NGR, Pannekoek A, Tian DH. Preoperative cigarette smoking and short-term morbidity and mortality after cardiac surgery: a meta-analysis. Heart Asia. 2018;10(2): e011069.
van Domburg RT, op Reimer WS, Hoeks SE, Kappetein AP, Bogers AJJC. Three life-years gained from smoking cessation after coronary artery bypass surgery: a 30-year follow-up study. Am Heart J. 2008;156(3):473–6.
Papathanasiou A, Milionis H, Toumpoulis I, Kalantzi K, Katsouras C, Pappas K, et al. Smoking cessation is associated with reduced long-term mortality and the need for repeat interventions after coronary artery bypass grafting. Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Card Rehabil Exerc Physiol. 2007;14(3):448–50.
Smith PM, Burgess E. Smoking cessation initiated during hospital stay for patients with coronary artery disease: a randomized controlled trial. CMAJ Can Med Assoc J J Assoc Medicale Can. 2009;180(13):1297–303.
Sköld CM, Hed J, Eklund A. Smoking cessation rapidly reduces cell recovery in bronchoalveolar lavage fluid, while alveolar macrophage fluorescence remains high. Chest. 1992;101(4):989–95.
Gofus J, Vobornik M, Sorm Z, Dergel M, Karalko M, Harrer J, et al. Female sex as a risk factor in minimally invasive direct coronary artery bypass grafting. Scand Cardiovasc J SCJ. 2019;53(3):141–7.
He GW, Acuff TE, Ryan WH, Mack MJ. Risk factors for operative mortality in elderly patients undergoing internal mammary artery grafting. Ann Thorac Surg. 1994;57(6):1453–60 (discussion 1460-1461).
Acknowledgements
Not applicable
Funding
The work was supported by institutional programme Progres Q40/04.
Author information
Authors and Affiliations
Contributions
YS—Writing—original draft, Investigation. JG—Project administration, Investigation, Data curation, Writing—original draft. JH—Investigation, Supervision. ZŠ—Data curation, Investigation, Writing—review & editing (R&E). MV—Investigation. EČ—Methodology, Formal analysis, Writing—review & editing (R&E). PS—Investigation. JV—Supervision, Validation, Writing R&E. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the local ethics committee (Ethics Committee at the University Hospital Hradec Kralove, 23 September 2021, Reference number 202109 P12). Individual patient informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Figures and Table.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shahin, Y., Gofus, J., Harrer, J. et al. Impact of smoking on the outcomes of minimally invasive direct coronary artery bypass. J Cardiothorac Surg 18, 43 (2023). https://doi.org/10.1186/s13019-023-02104-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02104-9