Abstract
Background
Short-term and long-term comparative outcomes after percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) for multivessel coronary artery (MVCA) or left main coronary artery (LMCA) disease are highly debated.
Goals
We performed a meta-analysis to evaluate the difference between PCI and CABG for the treatment of patients with MVCA or LMCA in long-term follow-up.
Methods
Literatures were searched in PubMed, EMBASE and The Cochrane Library from January 1, 2000 to January 1, 2021, including RCTs and observational studies (OSs). The primary outcome was all-cause mortality at 10 years follow-up, and the secondary outcomes included cardiac mortality, repeated revascularization, myocardial infarction, and stroke.
Results
A total of 5 RCTs reporting data from 3013 participants and 4 OSs of 5608 participants were included for analysis. There was no significant difference between PCI and CABG in all-cause mortality (Odds Ratio (OR) 1.03 [95% confidence interval (CI) 0.89 to 1.19]), whereas PCI was associated with higher cardiac mortality (OR 0.76 [95% CI 0.65 to 0.90]) and repeated revascularization rate comparing to CABG (OR 1.77 [95% CI 1.08 to 2.89]; I2 = 94.61%). The difference between PCI and CABG in repeated revascularization in either RCTs or OSs, in myocardial infarction in either RCTs or OSs were not significant. In OSs, stroke rate in PCI group was lower than those in CABG, but not in RCTs. There was a significant increase of stroke rate in CABG comparing to PCI (OR 0.65 [95% CI 0.53 to 0.80]; I2 = 0.00%). No significant difference between PCI and CABG in myocardial infarction was not observed (OR 0.92 [95% CI 0.64 to 1.31]; I2 = 57.84%).
Conclusion
Evidence from our study and prior studies suggested the superiority of CABG over PCI in improving 5- but not 10-year survival among patients with MVCA. In the contrast, there was no significant difference between CABG and PCI for treating patients with LMCA in either 5- or 10-year survival rate. More long-term trials are needed to better define differences of outcome between 2 techniques.
Similar content being viewed by others
Introduction
In the past few decades, several randomized clinical trials (RCTs) have compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with multiple vessels coronary artery disease (MVCA) or left main coronary artery disease (LMCA), as CABG was associated with lower incidence of all-cause death than PCI for patients with LMCA or MVCA in 5-year follow-up [1,2,3,4]. However, conflicting results between short-term and long-term comparative outcomes were found in this field. Patients with LMCA treated by CABG did not demonstrate significant difference in the incidence of all-cause death than PCI in the 10-year data [5]. On the contrary, a newly revealed RCT failed to demonstrate the non-inferiority of fractional flow reserve-guided PCI comparing to CABG in 1-year follow-up, triggering a heated discussion with regard to the most optimal treatment between PCI and CABG in treating MVCA or LMCA [6].
The 2018 European Society of Cardiology/European Association for Cardio-Thoracic Surgery Guidelines on myocardial revascularization assigned a Class I recommendation (“is recommended”) to CABG to improve outcomes among patients with LMCA or MVCA [7]. However, the supporting evidences were studies with no more than 5 years follow-up. To our best knowledge, there has been no meta-analysis of long-term (10 years) follow-up performed to compare the safety and efficacy of PCI and CABG in treating MVCA or LMCA. In this study, we comprehensively collected data and evaluated the difference in both RCTs and observational studies (OSs) that have compared PCI and CABG for the treatment of patients with MVCA or LMCA in 10-year follow-up, providing further insights into the comparative advantages of both revascularization techniques.
Methods
All supporting data in this article are available. Literatures were comprehensively searched by 2 reviewers in PubMed, EMBASE, Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cochrane Methodology) from January 1, 2000, to January 1, 2021. Details of searching algorithm were listed in the Additional file 1. This study was directed by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines for RCTs [8], along with the Meta-Analysis of Observational Studies in Epidemiology for OSs [9], and was registered at PROSPERO, number CRD42021247485.
We included studies comparing outcomes between PCI and CABG in treating coronary artery disease (CAD) of either MVCA or LMCA in 10 years follow-up. RCTs, prospective and retrospective OSs were all taken into consideration. Detailed selection criteria for inclusion/exclusion were showed in the Additional file 1.
The risk of bias was evaluated by 2 independent reviewers. Cochrane risk of bias assessment was used to evaluate RCT’s publication bias of including selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias [10]. The quality of OSs was assessed by using the Newcastle-Ottawa Scale [11].
Titles and abstracts of all studies were collected by 2 authors from databases mentioned above. All eligible studies were screened based on the inclusion and exclusion standards in Additional file 1. Divergences were resolved by consensus. Following data were extracted: (1) study features: authors, study design, sample size and quality of studies; (2) baseline information of patients; (3) outcomes: the primary outcomes was all-cause mortality at 10 years follow-up; the secondary outcomes included cardiac mortality, repeated revascularization, myocardial infarction and stroke at 10 years follow-up. Due to the variable definitions of major adverse cardiac and cerebrovascular event (MACCE) in different studies, we did not use MACCE as a measure of outcomes in this study [4, 12].
The Comprehensive Meta-Analysis 3.0 (Biostat, Englewood, NJ) was used to perform the data analysis. Owing to the intrinsic differences between RCTs and OSs, separate analyses of these 2 types of study designs were conducted. Odds ratios (ORs) with 95% confidence interval (CI) were measured and pooled for each outcome. Thanks to the diverse clinical features and methodological differences, a random-effect model was utilized for analyses [13]. We used the Q test and the calculation of I2 for the assessment of heterogeneity between studies. Substantial heterogeneity would be considered if P < 0.05 or I2 ≥ 50%. Subgroup and sensitivity tests were performed to investigate the source of heterogeneity. Due to the heterogeneity between studies, subgroup and sensitivity tests were performed in the categorization based on lesion location of patient, s baseline (LMCA or MCA) or types of PCI used in the studies(DES or BMS). Difference between subgroups was assessed by z test, and 2-tailed P < 0.05 was regarded as statistically significant.
Results
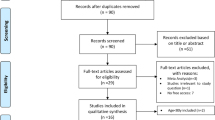
A total of 5 RCTs [5, 14,15,16,17] reporting data from 3013 participants and 4 OSs [18,19,20,21] of 5608 enrolled participants were included for analysis. A flowchart indicating selection strategy was showed in Fig. 1 and the baseline information of the participants was showed in Table 1. According to the Cochrane collaboration’s tool, the risk of bias in RCT was rated low (Additional file 1: Table S1). Owing to low comparability, 2 out of 4 studies were calculated as 6 by the Newcastle-Ottawa scale, while the rest studies were above 6 (Additional file 1: Table S2).
All-cause mortality
There was no significant difference between PCI and CABG in the incidence of all-cause mortality in RCTs {Odds Ratio (OR) 1.12 [95% confidence interval (CI) 0.95 to 1.33]; I2 = 0.00%} or cohort studies (OR 0.85 [95% CI 0.64 to 1.11]; I2 = 65.75%) or in total (OR 1.03 [95% CI 0.89–1.19]; I2 = 58.5%) (Fig. 2). And a statistical significance of OR was not observed between RCTs and OSs (P for interaction, 0.09). Due to the existence of heterogeneity, subgroup and sensitivity tests were performed in the categorization based on lesion location of patient’s baseline (LMCA or MCA) or types of stents used in the studies (DES or BMS). Significant difference between PCI and CABG in terms of LMCA (OR 0.93 [95% CI 0.72 to 1.19]) and MVCA (OR 0.99 [95% CI 0.83 to 1.19]), DES (OR 1.05 [95% CI 0.85 to 1.30]) and BMS (OR 0.83 [95% CI 0.24 to 2.83]) was not observed (Additional file 1: Tables S3 and S4).
Forest plot of OR of the composite of All-cause Mortality at follow-up for PCI vs. CABG (ASAN-MAIN ASAN Medical Center-Left MAIN Revascularization; CABG Coronary artery bypass graft; LE MANS Left main stenting trail; MASS-II Medicine, Angioplasty, or Surgery Study; MAIN-COMPARE Revascularization for unprotected left main coronary artery stenosis: Comparison of Percutaneous Coronary Angioplasty versus Surgical Revascularization; OSs Observational study; PCI Percutaneous coronary intervention; PRECOMBAT Premier of randomized comparison of bypass surgery; Angioplasty using sirolimus-eluting stent in patients with left main coronary artery disease; RCT Randomized controlled trial; SOS Stent or surgery; SYNTAX Synergy between percutaneous coronary intervention with TAXUS and cardiac surgery)
Cardiac mortality
There was a significant increase of cardiac morality rate in PCI comparing to CABG (OR 0.76 [95% CI 0.65 to 0.90]; I2 = 0.00%) (Fig. 3). Difference of cardiac morality between PCI and CABG in cardiac mortality in RCTs (OR 0.71 [95% CI 0.50 to 1.02]; I2 = 0.00%) was not observed, whereas PCI was associated with higher incidence in OSs (OR 0.78 [95% CI 0.65 to 0.94]; I2 = 0.00%). There was no significant difference in OR between RCTs and OSs (P for interaction, 0.66). Although statistic heterogeneity was not observed, subgroup studies were still performed to analyze potential clinical differences within studies. The results showed that there was no significant difference in cardiac mortality between PCI and CABG for LMCA (OR 0.90.95% CI 0.53 to 1.53). However, the difference in cardiac mortality between PCI and CABG for MVCA was statistically significant (OR 0.59 [95% CI 0.37 to 0.95]) (Additional file 1: Table S3).
Forest plot of OR of the composite of Cardiac Mortality at follow-up for PCI vs. CABG (ASAN-MAIN ASAN Medical Center-Left MAIN Revascularization; CABG Coronary artery bypass graft; LE MANS Left main stenting trail; MASS-II Medicine, Angioplasty, or Surgery Study; OSs Observational study; PCI Percutaneous coronary intervention; PRECOMBAT Premier of randomized comparison of bypass surgery; Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; RCT Randomized controlled trial; SOS Stent or surgery)
Repeated revascularization
PCI was associated with higher rate of repeated revascularization rate comparing to CABG (OR 1.77 [95% CI 1.08 to 2.89]; I2 = 94.61%) (Fig. 4). The rate of repeat revascularization between PCI and CABG was not significantly different in RCTs (OR 1.54 [95% CI 0.89 to 2.67] ; I2 = 67.9%) and OSs (OR 2.40 [95% CI 0.95 to 6.03] ; I2 = 97.1%). There was no significant difference in OR between RCTs and OSs (P for interaction, 0.42). Subgroup tests were performed owing to heterogeneity, showing that no substantial difference between LMCA (OR 1.38 [95%, 0.51 to 3.78]) and MVCA (OR 1.77 [95%, 0.62 to 5.07]) was detected (Additional file 1: Tables S3 and S4). In contrast to DES (OR 1.40 [95% CI 0.68 to 2.87]), BMS was associated with higher incidence of repeated revascularization than CABG in OSs (OR 4.16 [95% CI 3.07 to 5.64]).
Forest plot of OR of the composite of Repeated Revascularization at follow-up for PCI vs. CABG (ASAN-MAIN ASAN Medical Center-Left MAIN Revascularization; CABG Coronary artery bypass graft; LE MANS Left main stenting trail; MASS-II Medicine, Angioplasty, or Surgery Study; MAIN-COMPARE Revascularization for unprotected left main coronary artery stenosis: Comparison of Percutaneous Coronary Angioplasty versus Surgical Revascularization; OSs Observational study; PCI Percutaneous coronary intervention; PRECOMBAT Premier of randomized comparison of bypass surgery; Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; RCT Randomized controlled trial; SOS Stent or surgery)
Stroke
There was a significant increase of stroke rate in CABG comparing to PCI (OR 0.65 [95% CI 0.53 to 0.80]; I2 = 0.00%) (Fig. 5). In cohort studies, incidence of stroke in PCI group was lower than those in CABG (OR 0.64 [95% CI 0.51 to 0.80]; I2 = 0.00%), whereas no significant difference between PCI and CABG in RCT was observed (OR 0.77 [95% CI 0.44 to 1.37]; I = 0.00%). Difference of OR was not observed between RCTs and OSs (P for interaction, 0.54). In subgroup studies, there was not significant difference between LMCA (OR 0.78 [95% CI 0.29 to 2.12]) and MVCA (OR 0.77 [95% CI, 0.38 to 1.55]) (P = 1.00) (Additional file 1: Table S3) (Fig. 5).
Forest plot of OR of the composite of Stroke at follow-up for PCI vs. CABG (ASAN-MAIN ASAN Medical Center-Left MAIN Revascularization; CABG Coronary artery bypass graft; LE MANS Left main stenting trail; MASS-II Medicine, Angioplasty, or Surgery Study; OSs Observational study; PCI Percutaneous coronary intervention; PRECOMBAT Premier of Randomized Comparison of Bypass Surgery; Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; RCT Randomized controlled trial; SOS Stent or surgery)
Myocardial infarction
No significant difference between PCI and CABG in myocardial infarction in RCTs (OR 0.84 [95% CI, 0.49 to 1.44]; I2 = 58.30%) or cohort studies (OR, 0.99 [95% CI 0.61 to 1.59]; I2 = 68.02%), or in total (OR 0.92 [95% CI 0.64 to 1.31]; I2 = 57.84%) was not observed. Statistical difference of OR was not observed between RCTs and cohort studies (P for interaction, 0.67). Due to the existence of heterogeneity, subgroup tests were performed. Comparing to PCI, CABG was associated with higher rate of myocardial infarction in MVCA (OR 0.57 [95% CI 0.25 to 0.92]), while there was no significant difference between PCI and CABG in LMCA (OR 0.78 [95%, 0.29 to 2.12]). Significant difference was observed between LMCA and MVCA (P = 0.01) (Additional file 1: Table S4) (Fig. 6).
Forest plot of OR of the composite of Myocardial Infarction at follow-up for PCI vs. CABG (ASAN-MAIN ASAN Medical Center-Left MAIN Revascularization; CABG Coronary artery bypass graft; LE MANS Left main stenting trail; MASS-II Medicine, Angioplasty, or Surgery Study; OSs Observational study; PCI Percutaneous coronary intervention; PRECOMBAT Premier of randomized comparison of bypass surgery; Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; RCT Randomized controlled trial; SOS Stent or surgery)
Discussion
To our best knowledge, our study is the first meta-analysis to present 10-year comparative outcomes between PCI and CABG for treating patients with either LMCA or MVCA. We tried to overcome potential problems that might weaken the credibility of clinical evidence in previous studies. For example, in a meta-analysis of left main coronary artery, data from OSs and RCTs was pooled together without classification, leading to a less credible conclusion due to the internal difference between 2 types of studies [22]. For the same reason, unlike obscure definition of CAD in a meta-analysis involving 23 RCTs, we primarily focused on CAD with LMCA or MVCA, which is more clinical applicable [23].
In our study, after 10-year follow-up, there was no significant difference of all-cause mortality rate between PCI and CABG in treating MVCA or LMCA in both RCTs and OSs group, as well as in subgroups categorized by lesion locations or types of PCI. In our subgroup analysis of mortality, PCI was not associated with better outcome in either LMCA or MVCA subgroups. Previous publications showed that CABG had a mortality benefit over PCI among patients with MVCA, but not among patients with LMCA in both short-term and long-term follow-up studies [5, 24]. Combining the results from our study and prior studies, it showed that CABG improved 5-year survival but not 10-year survival among patients with MVCA. In the contrast, there was no significant difference between CABG and PCI for treating patients with LMCA in either 5-year or 10-year survival rate.
Different results between our studies and previous studies in terms of all-cause death rate could be explained by the discrepancy of patients’ lesion complexity in the 2 groups. For example, an included study showed that CABG group has higher rates of myocardial infarction history, left main plus triple-vessel disease and chronic total occlusion than PCI group [20]. The same situation appeared in another 2 included studies, as patients undergoing CABG were with higher clinical and anatomic risk factor profiles than those treated by PCI [18, 19]. Thus, the therapeutic effect of CABG might be underpowered due to the fact that the lesion of CAD among patients treated by CABG was often associated with higher-risk clinical and angiographic situation than that among those treated by PCI [15, 21]. Except Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trail and Left Main Stenting (LE MANS) trail, other included studies were lack of syntax score evaluation, especially in the observational studies, leading to a unquantifiable and unstandardized process for patients’ selection.
In addition, comparing to CABG, our results suggested that PCI was associated with higher incidence in cardiac mortality, but with lower incidence of cardiac death among patients with MVCA. These findings contradicted the common perception based on the evidence from 5-year data of SYNTAX trail [25]. Following reasons may play roles in the explanation of this contradiction. Firstly, after investigation for underlying reasons, we identified an included OS which only enrolled diabetic patients might affect the effect size of final result [21]. Except this study, only 20 ~ 30% candidates in the PCI and CABG group from other 2 included studies had diabetes. We did sensitivity test by excluding the study that primarily focused on diabetic patients [26]. After the exclusion of that study, we found that there was no difference between PCI and CABG in cardiac mortality, which was in line with previous findings. Secondly, the application of dual antiplatelet therapy after PCI was found to reduce the incidence of death and myocardial infarction in some measure, causing the equivalent cardiac death rate between PCI and CABG [27].
Our results in terms of lower incidence of stroke in PCI group at 10-year follow-up was consistent with previous findings from an individual patient data meta-analysis of 11 RCTs at 3.3-year follow-up, showing that CABG had a significantly higher stroke incidence at 5-year follow-up [28]. Multifactor were likely to contribute to the increased risk of stroke with CABG. The usage of on-pump and off-pump in surgical procedures, intra-operative hypoperfusion, strategies for post-operative bleeding control and post-operative atrial fibrillation might lead to higher stroke risk with surgery. However, in the latest revealed RCT comparing PCI to CABG, there were no obvious differences of stroke rate between 2 groups, as the usage of postoperative double-antiplatelet rates reached up to 45% which was higher or at least consistent with data from previous large RCTS [6]. In our subgroup study, we also found that BMS was associated with higher incidence of repeated revascularization than DES, which is in line with findings from previous publications [29, 30].
Limitation
Few limitations including the synthesis of heterogeneous trials in terms of variable study design and characteristics were detected. For this reason, we utilized random-effects model and heterogeneity test to reduce statistics bias. What’s more, there was one included RCTwith9.6 ± 0.85 years follow-up on average [14], and another included OS with candidates who were all diabetic and MVCA patients [21]. We performed sensitivity and subgroup analyses showing that all results remained robust when excluding these 2 studies. Besides, thanks to limited numbers of studies and data in this area, we were unable to perform meta-regression to find clinical predictors for better outcomes after treatment. SYNTAX score has been considered as an important predictor for higher survival rate as both 5-year individual data from 11 RCTs and 10-year data from SYNTAX trail confirmed that CAD patients with SYNTAX score ≥ 33 treated by CABG had lower mortality rate than PCI [5, 24]. However, only 2 included trails had SYNTAX score so that we were unable to further explore the impact of SYNTAX score on the patients’ outcome after treated by PCI or CABG.
Conclusion
Evidence from our study and prior studies suggested the superiority of CABG over PCI in improving 5- but not 10-year survival among patients with MVCA. In the contrast, there was no significant difference between CABG and PCI for treating patients with LMCA in either 5- or 10- years survival rate.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- BMS:
-
Bare metal stent
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- DES:
-
Drug-eluting stent
- LMCA:
-
Left main coronary artery
- MACCE:
-
Major adverse cardiac and cerebrovascular event
- MVCA:
-
Multivessel coronary artery
- OSs:
-
Observational studies
- RCT:
-
Randomized controlled trial
References
Mäkikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IBA, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016;388(10061):2743–52.
Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016;375(23):2223–35.
Park S-J, Kim Y-H, Park D-W, Yun S-C, Ahn J-M, Song HG, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364(18):1718–27.
Stone GW, Kappetein AP, Sabik JF, Pocock SJ, Morice M-C, Puskas J, et al. Five-year outcomes after PCI or CABG for left main coronary disease. N Engl J Med. 2019;381(19):1820–30.
Thuijs DJFM, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJ, et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet. 2019;394(10206):1325–34.
Fearon WF, Zimmermann FM, De Bruyne B, Piroth Z, van Straten AHM, Szekely L, et al. Fractional flow reserve–guided PCI as compared with coronary bypass surgery. N Engl J Med. 2022;386(2):128–37.
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: elaboration and explanation. BMJ (Online). 2015;349.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(7829):1–9.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Park S-J, Ahn J-M, Kim Y-H, Park D-W, Yun S-C, Lee J-Y, et al. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med. 2015;372(13):1204–12.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Buszman P, Wiernek S, Szymanski R, Bialkowska B, Buszman P, Fil W, et al. Percutaneous versus surgical revascularization for multivessel coronary artery disease: a single center 10 year follow-up of SOS trial patients. Catheter Cardiovasc Interv. 2009;74(3):420–6.
Park DW, Ahn JM, Park H, Yun SC, Kang DY, Lee PH, et al. Ten-year outcomes after drug-eluting stents versus coronary artery bypass grafting for left main coronary disease: extended follow-up of the PRECOMBAT trial. Circulation. 2020;141(18):1437–46.
Buszman PE, Buszman PP, Banasiewicz-Szkróbka I, Milewski KP, Zurakowski A, Orlik B, et al. Left main stenting in comparison with surgical revascularization: 10-year outcomes of the (left main coronary artery stenting) le MANS trial. JACC Cardiovasc Interv. 2016;9(4):318–27.
Hueb W, Lopes N, Gersh BJ, Soares PR, Ribeiro EE, Pereira AC, et al. Ten-year follow-up survival of the medicine, angioplasty, or surgery study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2010;122(10):949–57.
Park DW, Ahn JM, Yun SC, Yoon YH, Kang DY, Lee PH, et al. 10-Year outcomes of stents versus coronary artery bypass grafting for left main coronary artery disease. J Am Coll Cardiol. 2018;72(23):2813–22.
Park DW, Kim YH, Yun SC, Lee JY, Kim WJ, Kang SJ, et al. Long-term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 10-year results of bare-metal stents and 5-year results of drug-eluting stents from the ASANMAIN (ASAN Medical center left MAIN) reva. J Am Coll Cardiol. 2010;56(17):1366–75.
Yu XP, Li Y, He JQ, Jin ZN. Twelve-year outcomes after revascularization for ostial/shaft lesions in unprotected left main coronary artery. J Geriatr Cardiol. 2020;17(6):338–43.
Nyström T, Sartipy U, Franzén S, Eliasson B, Gudbjörnsdottir S, Miftaraj M, et al. PCI Versus CABG in patients with type 1 diabetes and multivessel disease. J Am Coll Cardiol. 2017;70(12):1441–51.
Khan MR, Kayani WT, Ahmad W, Hira RS, Virani SS, Hamzeh I, et al. Meta-analysis of comparison of 5-year outcomes of percutaneous coronary intervention versus coronary artery bypass grafting in patients with unprotected left main coronary artery in the era of drug-eluting stents. Am J Cardiol. 2017;120(9):1514–20.
Gaudino M, Hameed I, Farkouh ME, Rahouma M, Naik A, Robinson NB, et al. Overall and cause-specific mortality in randomized clinical trials comparing percutaneous interventions with coronary bypass surgery: a meta-analysis. JAMA Intern Med. 2020;180(12):1638–46.
Head SJ, Milojevic M, Daemen J, Ahn JM, Boersma E, Christiansen EH, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018;391(10124):939–48.
Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381(9867):629–38.
Farkouh ME, Domanski M, Sleeper LA, Siami FS, Dangas G, Mack M, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367(25):2375–84.
Duan HQ, Dong PS, Wang HL, Li ZJ, Du LJ, Zhao YW. Effect of prolonged dual anti-platelet therapy on reducing myocardial infarction rate after percutaneous coronary intervention. J Biol Regul Homeost Agents. 2015;29(1):213–9.
Head SJ, Milojevic M, Daemen J, Ahn JM, Boersma E, Christiansen EH, et al. Stroke rates following surgical versus percutaneous coronary revascularization. J Am Coll Cardiol. 2018;72(4):386–98.
Bønaa KH, Mannsverk J, Wiseth R, Aaberge L, Myreng Y, Nygård O, et al. Drug-eluting or bare-metal stents for coronary artery disease. N Engl J Med. 2016;375(13):1242–52.
Mahmoud AN, Shah NH, Elgendy IY, Agarwal N, Elgendy AY, Mentias A, et al. Safety and efficacy of second-generation drug-eluting stents compared with bare-metal stents: an updated meta-analysis and regression of 9 randomized clinical trials. Clin Cardiol. 2018;41(1):151–8.
Acknowledgements
None.
Funding
This work was supported by National Key Research and Development Program of China from the China National Center for Biotechnology Development, and the grant number was 2018YFC2002300. This work was also supported by two grants from Health Commission of Henan Province, and the grant numbers were 2018020244 and HGJ20190415 respectively.
Author information
Authors and Affiliations
Contributions
YZ designed this work. STF searched the articles. STF, LML, and JYF performed the data extraction and statistical analyses. STF and LML wrote this article. AQD, WLZ and FYH participated in the production of Figs. 1, 2, 3, 4, 5 and 6. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a meta-analysis and ethics approval and consent to participate are not required.
Consent for publication
This is a meta-analysis and consent for publication is not required.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplemental material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Feng, S., Li, M., Fei, J. et al. Ten-year outcomes after percutaneous coronary intervention versus coronary artery bypass grafting for multivessel or left main coronary artery disease: a systematic review and meta-analysis. J Cardiothorac Surg 18, 54 (2023). https://doi.org/10.1186/s13019-023-02101-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02101-y