Abstract
Background
The efficacy of off-pump coronary endarterectomy (CE) has been proven in patients with diffuse coronary artery disease (DCAD). However, the clinical benefits of of-pump CE stratified by different target vessels remain controversial. This retrospective study assessed the effect of the territory and number of CE on short- and long-term outcomes of DCAD.
Methods
From January 2012 to December 2014, 246 patients undergoing off-pump coronary artery bypass grafting (OPCABG) + CE were included. The patients were grouped by the territory and number of CE. The primary endpoints were postoperative acute myocardial infarction (PMI) and long-term major adverse cardiovascular and cerebrovascular events (MACCE).
Results
Sixty-five patients (26.42%) were in the left anterior descending branch (LAD) group (CE on LAD), 134(54.47%) in the right coronary artery (RCA) group (CE on RCA), and 47(19.10%) in the multi-vessels group. PMI in the LAD group, RCA group, and multi-vessels group were 3.08%, 6.72%, and 14.89%, respectively (P = 0.08). Multi-vessels CE (OR = 9.042, 95%CI 2.198–37.193, P = 0.002), CE-plaque length ≥ 3 cm (OR = 6.247, 95%CI 2.162–18.052, P < 0.001), and type 2 diabetes mellitus (2DM) (OR = 4.072, 95%CI 1.598–10.374, P = 0.003) were independent risk factors of PMI. The long-term (mean 76 months) MACCE in the LAD group, RCA group, and multi-vessels group were 13.85%, 17.91%, and 10.64%, respectively (P = 0.552). Cox analysis indicated that PMI (HR = 7.113, 95%CI 3.129–16.171, P < 0.001) and Age ≥ 65 years (HR = 2.488, 95%CI 1.214–5.099, P = 0.013) increased the risk of long-term MACCE.
Conclusions
Multi-vessel CE and CE-plaque length ≥ 3 cm significantly increased risk of PMI after OPCABG + CE, but the territory and number of CE did not affect long-term MACCE.
Similar content being viewed by others
Background
Coronary endarterectomy (CE) has been a proven surgical technique for complete myocardial revascularization in diffuse coronary artery disease (DCAD) [1, 2]. Although increasing advances in surgical techniques and aggressive antithrombotic therapy, many cardiac surgeons avoided performing CE during Coronary artery bypass grafting (CABG) due to life-threatening postoperative myocardial infarction (PMI). In recent years, patients needed to CABG are often accompanied by more complex coronary artery lesions with multi-comorbidities because of increasing improvement in the percutaneous coronary intervention [3, 4]. So, CE is still a necessary surgical technique in selected cases. Many studies have focused on the safety and efficacy of CE with different techniques (off-pump vs on-pump, open-CE vs closed-CE) [5, 6]. However, the clinical benefits of CE stratified by territory and number of target vessels remain controversial. In this retrospective study, we investigated the effect of the territory and number of CE on short- and long-term outcomes in patients undergoing off-pump CABG + closed CE.
Methods
Patients and grouping
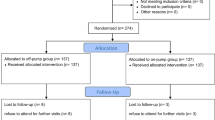
Between January 2012 and December 2014, 271 patients with DCAD who received off-pump CABG + CE were included in this study. Exclusion criteria included (1) Presence of one- or double-vessel disease; (2)SYNTAX score ≤ 23; (3) Urgent or emergent CABG; (4) Being concomitant valvular or aortic surgery; (5) Urgent switching from off-pump to on-pump CABG.
Referring to the exclusion criteria, a total of 246 patients were included in this retrospective study. According to the territory and number of CE, patients were divided into LAD group (CE on left anterior descending artery n = 65), RCA group (CE on the right coronary artery, n = 134), and Multi-vessels group [at least CE on two of LAD, RCA and left circumflex artery (LCX), n = 47].
The study was carried out following the Ethical Guideline of the Committee on Human Experimentation of our institution, and informed consent was obtained from the patients about the experimentation (Ethics approval number 2021050X).
Surgical procedure
Off-pump CABG + CE was performed with a standard procedural protocol involving general anesthesia, median sternotomy, systemic heparinization with activated clotting time (ACT) > 300 s, and harvesting of the left internal mammary artery (LIMA) and saphenous vein (SV). LIMA was always anastomosed to LAD. The sequential SV graft was performed by proximal anastomosis to the ascending aorta firstly, and then distal anastomosis to LCX and RCA in succession. For selected patients with indications, the bilateral internal mammary arteries were used with a composite “Y” graft (LIMA in situ and RIMA grafted to LIMA) [7].
The CE was performed by as follow indications: (1) Coronary angiography indicating diffuse lesions with length > 2 cm, luminal diameter < 1 mm in the main coronary artery; (2) intraoperative inspection finding no suitable anastomotic location in the middle-distal of the coronary artery with a wide blood supply territory. The atherosclerotic plaque was removed using the closed-CE technique. The closed-CE was performed with the following steps: (1) Coronary knife to make a 5–8 mm arteriotomy at the anastomotic site; (2) Potts scissors to peel intimal plaque from adventitia on both sides of incision; (3) Pull plaque using forceps with the help of the reaction force form heart contracts. The distal end of the plaque needed to be completely peeled. The proximal end of plaque was peeled 3–5 mm and then cut off sharply to avoid competitive flow. A satisfactory standard of closed-CE was that the distal end of plaque was present of a translucent and rat-tail shape with blood back-flow via arteriotomy. If the distal end of plaque was not peeled completely, open-CE with extended arteriotomy and vein patch angioplasty was performed. The diameter of all target vessels for bypass grafting should be ≥ 1.5 mm referring to 1.5 mm coronary probe during operation. The postoperative antithrombotic strategy included (1) Unfractionated heparin to maintain ACT > 180 s from 3 h after surgery to extubation if bleeding < 300 ml in the first 3 h after surgery; (2) Low molecular heparin to bridge-therapy for 3 days after extubation; (3) Dual antiplatelet therapy at 6–24 h after surgery and continuing for one year; (4) One antiplatelet continuing for life.
End-points
The primary end-points were PMI and long-term major adverse cardiovascular and cerebrovascular events (MACCE). MACCE included MI, death, redo revascularization, and stroke. The PMI was defined by (1) Postoperative cTnI more than 10 times the 99th percentile of the upper limit of normal reference value with normal preoperative cTnI value; (2) Ongoing evidence of myocardial ischemia including new pathology Q wave formation, coronary angiography confirming the presence of new coronary or grafts occlusion, imaging evidence of new viable myocardium loss or local wall motion abnormalities consistent with ischemic etiology [8].
The secondary end-points included death in hospital, duration of mechanical ventilation, and ICU stays, mechanical circulation support, and long-term survival. Follow-up was mainly performed by outpatient and telephone interviews, and ended in February 2021. All patients received guideline-directed medical therapy (GDMT) after surgery [9].
Statistical analysis
Statistical analysis was performed using an extensively admissive software program SAS software (version 9.4; SAS Institute Inc., Cary, NC, USA). Data were presented as means ± standard deviation (SD) or median with interquartile range for continuous variables and as frequencies and percentages for categorical variables. The ANOVA test was used to address non-paired samples for the comparison of normally distributed parameters and the Wilcoxon rank-sum test for the comparison of non-parametric variables. The Chi-squared test and Fisher's exact test were applied for the comparison of categorical variables. The multivariate logistic regression analysis was performed to calculate odds ratio (OR) and 95% confidence interval (CI) for identifying the risk factors of PMI. Kaplan–Meier survival analysis was performed for long-term survival. Cox proportional hazards model was used for identifying risk factors of long-term MACCE. Differences were considered statistically significant only when the p-value was < 0.05.
Results
Baseline characteristics
A total of 246 patients with mean age (61.30 ± 8.47) years and 78.86% male were studied. Sixty-five patients (26.42%) were in the LAD group, 134 (54.47%) in the RCA group, and 47 (19.10%) in the multi-vessels group. The characteristic distribution of other demographics, cardiac function parameters, comorbidities in three groups was summarized in Table 1.
Surgical characteristics and short-term outcomes
There was no difference in the number of graft anastomosis and LIMA grafting in the three groups. Mortality in hospital and PMI in all patients was 2.85% and 7.32%, respectively. Incidence of PMI in LAD group, RCA group, and multi-vessels group were 3.08%, 6.72%, and 14.89%, respectively, P = 0.08. The duration of mechanical ventilation, ICU stays, and mechanical circulation support was no different in the three groups. The details were shown in Table 2. The multivariate logistic regression analysis (Fig. 1) indicated that multi-vessels CE (OR = 9.042, 95%CI 2.198–37.193, P = 0.002), CE-plaque length ≥ 3 cm (OR = 6.247, 95%CI 2.162–18.052, P < 0.001), and 2DM (OR = 4.072, 95%CI 1.598–10.374, P = 0.003) were independent risk factors of PMI.
The multivariate logistic regression analysis for risk factors of PMI after off-pump CABG + CE. BMI, body mass index; CABG, coronary artery bypass grafting; CE, coronary endarterectomy; DM, diabetes mellitus; LAD, left anterior descending artery; PMI, postoperative myocardial infarction; RCA, right coronary artery
Long-term outcomes
Follow-up was completed in 97% of patients. The median duration of follow-up was 79 (73, 86) months. The cumulative incidence of MACCE in the LAD group, RCA group, and multi-vessels group were 13.85%, 17.91%, and 10.64%, respectively (P = 0.522). The stroke rate in the LAD group was higher than in other groups (6.15% vs 0.75% vs 0%, P = 0.034). But repeat revascularization after angiography was no significant difference in the three groups. The long-term outcomes were summarized in Table 3.
Kaplan–Meier survival analysis (Fig. 2) indicated that the 8-year cumulative survival rate in the three groups was no different, log-rank P = 0.145. The COX regression analysis (Fig. 3) indicated that PMI (HR = 7.113, 95%CI 3.129–16.171, P < 0.001) and Age ≥ 65 years (HR = 2.488, 95%CI 1.214–5.099, P = 0.013) were independent risk factors of long-term MACCE.
Discussion
This study investigated the effect of the number and territory of CE on clinical outcomes in patients undergoing off-pump CABG + CE. The main findings included that multi-vessels CE, CE-plaque length ≥ 3 cm, and 2DM were independent risk factors of PMI; long-term MACCE and survival were similar irrespective of the territory and number of CE.
In recent years, advancements in antithrombotic agents, surgical techniques, and perioperative care management maybe reduce the risk of morbidity and mortality in DCAD patients [10]. The incidence of PMI was 7.32% in this study, which was lower than that in a previous study [11]. In this study, we adopted a more radical antithrombotic strategy, namely dual antiplatelet + heparin in three days after surgery. But bleeding risk (requiring transfusion) was not significantly increased compared with previous studies [12].
Acute thrombosis is the most common cause resulting in PMI due to CE breaking the structural and functional integrity of coronary endothelium [13]. This study indicated that the more extensive CE (multivessel CE and CE-plaque length ≥ 3 cm) was performed, the more risk of PMI occurred, irrespective of the territory of CE. For patients undergone extensive CE, based on aggressive antithrombotic therapy, maintaining high blood perfusion of graft and coronary maybe reduce the risk of PMI after CE. In our previous study, prophylactic use of IABP during intraoperative remarkably reduced PMI in patients who suffered from extensive CE [14].
Furthermore, 2DM was also an independent risk factor of PMI. The main reason was that 2DM promoted a rapidly progress of coronary atherosclerosis [15]. Unfortunately, the prediabetes was also associated with a smaller coronary size and diffuse coronary narrowing [16]. So, the patients with coronary artery disease and 2DM have smaller-caliber vessels with more severe, extensive-diffuse atherosclerotic lesions. And previous studies indicated that the coronary artery caliber was the strongest predictors of perioperative mortality [17, 18]. Clinical management of DCAD complicated with 2DM should be strengthened for improving outcomes [19].
CE mainly affects early outcomes due to the high risk of thrombosis. Our results showed long-term outcomes were similar in terms of MACCE and survival in the three groups, although the incidence of stroke in the LAD group was significantly higher than the other two groups, which may be related to the high rate of preoperative history of stroke in the LAD group. So, regardless of the number and territory of CE, complete removing plaques at the distal of anastomosis site and complete revascularization were critical to maintain good run-off and improve long-term prognosis.
Mature CE technique is the guarantee of complete removing plaques. Surgical techniques treating DCAD include off-pump or on-pump open-CE and closed-CE. Previous studies indicated that the operative mortality was not statistically different between the on-pump CABG + CE versus off-pump CABG + CE groups or between open-CE versus closed-CE [5, 6]. In this study, the off-pump closed CE technique was used in the majority of patients. The key points of off-pump closed CE technique include (1) Mature atherosclerotic plaques, (2) Incision closing to distal segment of the plaque, and (3) gently pulling out plaque with help of counterforce from heart contraction.
Moreover, reendothelialization after CE also reduces the risk of long-term restenosis and thrombosis. Evidence from the animal model and human angiographic study has shown that neointima circumferentially covered the endarterectomies lumen [20, 21]. In a porcine coronary endothelial injury model, intimal regeneration has been observed at 35 days after coronary artery injury [22]. GDMT has also played an important role in improving long-term outcomes. Our results indicated that although 2DM was one of the risk factors causing PMI, it did not impact long-term MACCE.
Limitations
Several limitations should be considered. First, the retrospective study was susceptible to inherent bias. Second, patients in the multi-vessels CE group were small. Multi-vessels CE was an independent risk factor causing PMI, but PMI was no difference between groups. Further study should enroll in more patients to testify these results. Third, coronary angiography was not routine follow-up content, coronary artery computed tomographic angiography will be needed to access graft patency in the different territory after CE.
Conclusions
Whole removing coronary plaque in run-off and complete revascularization were critical to improving long-term outcomes in patients received off-pump CABG + closed CE, regardless of territory and number of CE. Multi-vessels CE and CE-plaque length ≥ 3 cm were independent risk factors causing PMI. The territory and number of CE did not affect long-term clinical outcomes.
Availability of data and materials
The datasets used are available from the corresponding author on reasonable request.
Abbreviations
- ACT:
-
Activated clotting time
- CABG:
-
Coronary artery bypass grafting
- CE:
-
Coronary endarterectomy
- DCAD:
-
Diffuse coronary artery disease
- DM:
-
Diabetes mellitus
- LAD:
-
Left anterior descending artery
- LCX:
-
Left circumflex artery
- LIMA:
-
Left internal mammary artery
- GDMT:
-
Guideline-directed medical therapy
- MACCE:
-
Major adverse cardiovascular and cerebrovascular events
- PMI:
-
Postoperative acute myocardial infarction
- RCA:
-
Right coronary artery
- SV:
-
Saphenous vein
References
Costa M, Betero AL, Okamoto J, Schafranski M, Reis ESD, Gomes RZ. Coronary endarterectomy: a case control study and evaluation of early patency rate of endarterectomized arteries. Braz J Cardiovasc Surg. 2020;35:9–15.
Janiec M, Ragnarsson S, Nozohoor S. Long-term outcome after coronary endarterectomy adjunct to coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2019;29:22–7.
Kappetein AP, van Mieghem NM, Head SJ. Revascularization options: coronary artery bypass surgery and percutaneous coronary intervention. Heart Fail Clin. 2016;12:135–9.
Head SJ, Davierwala PM, Serruys PW, Redwood SR, Colombo A, Mack MJ, et al. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: final five-year follow-up of the SYNTAX trial. Eur Heart J. 2014;35:2821–30.
Lee JH, Lim C, Kim JS, Park KH. Early and mid-term results of coronary endarterectomy: influence of cardiopulmonary bypass and surgical techniques. Cardiol J. 2017;24:242–9.
Soylu E, Harling L, Ashrafian H, Athanasiou T. Does coronary endarterectomy technique affect surgical outcome when combined with coronary artery bypass grafting? Interact Cardiovasc Thorac Surg. 2014;19:848–55.
Gu CX, Yang JF, Zhang HC, Wei H, Li LK. Off-pump coronary artery bypass grafting using a bilateral internal mammary artery Y graft. J Geriatr Cardiol. 2012;9:247–51.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138:e618–51.
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016;68:1082–115.
Eikelboom R, Amir T, Gupta S, Whitlock RP. Optimal medical therapy after coronary artery bypass grafting: a primer for surgeons. Curr Opin Cardiol. 2021;36:609–15.
Nardi P, Russo M, Saitto G, Bovio E, Vacirca SR, Bassano C, et al. Coronary endarterectomy: an old tool for patients currently operated on with coronary artery bypass grafting. Long-term results, risk factor analysis. Kardiochir Torakochirurgia Pol. 2018;15:219–26.
Yan H, Tiemuerniyazi X, Song Y, Xu F, Feng W. Comparison of dual antiplatelet therapies after coronary endarterectomy combined with coronary artery bypass grafting: a cohort study. J Cardiothorac Surg. 2020;15:155.
Uchimuro T, Fukui T, Mihara W, Takanashi S. Acute thrombosis after endarterectomy of stented left anterior descending artery. Interact Cardiovasc Thorac Surg. 2009;8:663–5.
Wu Z, Liu C, Fang Y, Wei H, Gu C. Intraoperative intra-aortic balloon pump improves 30-day outcomes of patients undergoing extensive coronary endarterectomy. J Cardiothorac Surg. 2020;15:223.
Naito R, Miyauchi K. Coronary artery disease and type 2 diabetes mellitus. Int Heart J. 2017;58:475–80.
Ertan C, Ozeke O, Gul M, Aras D, Topaloglu S, Kisacik HL, et al. Association of prediabetes with diffuse coronary narrowing and small-vessel disease. J Cardiol. 2014;63:29–34.
Zhou FF, Liu YH, Ge PC, Chen ZH, Ding XQ, Liu JY, et al. Coronary artery diameter is inversely associated with the severity of coronary lesions in patients undergoing coronary angiography. Cell Physiol Biochem. 2017;43:1247–57.
Fisher LD, Kennedy JW, Davis KB, Maynard C, Fritz JK, Kaiser G, et al. Association of sex, physical size, and operative mortality after coronary artery bypass in the Coronary Artery Surgery Study (CASS). J Thorac Cardiovasc Surg. 1982;84:334–41.
Arnold SV, Bhatt DL, Barsness GW, Beatty AL, Deedwania PC, Inzucchi SE, et al. Clinical management of stable coronary artery disease in patients with type 2 diabetes mellitus: a scientific statement from the American heart association. Circulation. 2020;141:e779–806.
Liang M, Liang A, Wang Y, Jiang J, Cheng J. Smooth muscle cells from the anastomosed artery are the major precursors for neointima formation in both artery and vein grafts. Basic Res Cardiol. 2014;109:431.
Okada T, Minato N, Kanemoto SY, Zempo N, Saiga K, Namikawa K, et al. Intimal regeneration after coronary endarterectomy and onlay grafting in coronary artery bypass grafting. Gen Thorac Cardiovasc Surg. 2019;67:677–83.
Shi Y, O’Brien JE, Fard A, Mannion JD, Wang D, Zalewski A. Adventitial myofibroblasts contribute to neointimal formation in injured porcine coronary arteries. Circulation. 1996;94:1655–64.
Acknowledgements
We thank all the participating colleagues and nurses for their assistance in building of case data.
Funding
This study was funded by National Natural Science Foundation of China [Grant numbers 82070483]; Scientific Research Common Program of Beijing Municipal Commission of Education [Grant numbers KM202110025014]; Beijing Hospitals Authority Clinical medicine Development of special funding support [Grant numbers XMLX202107].
Author information
Authors and Affiliations
Contributions
CG, HL and CL designed the study and revised the article; Ying Fang, HW, ZW and WS carried out the study including collecting data, follow-up and data processing; YF wrote the article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent for participate
Ethics approval for this study was obtained from the ethics review committee for human studies of Beijing Anzhen Hospital, Capital Medical University. The written informed consent was obtained from the patients in this study.
Consent for publication
This paper has been reviewed and approved by all the co-authors, and has not been submitted to any other journals for consideration for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fang, Y., Wei, H., Wu, Z. et al. Short and long-term outcomes after off-pump coronary endarterectomy stratified by different target vessels. J Cardiothorac Surg 17, 339 (2022). https://doi.org/10.1186/s13019-022-02089-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-02089-x