Abstract
Objectives
Esophageal squamous cell carcinoma with pulmonary metastasis has a poor prognosis, and the only treatment modality is systemic therapy such as chemotherapy. Previous studies showed that pulmonary metastasectomy may provide benefits and has been suggested in selected patients with colorectal cancer, renal cancer, and sarcoma. However, there were few literatures evaluating the impact and treatment outcome of pulmonary metastasectomy in esophageal squamous cell carcinoma patients with isolated lung metastases. Therefore, we conducted this study.
Methods
We retrospectively reviewed our patients with esophageal squamous cell carcinoma with pulmonary metastasis. Patients with extrapulmonary metastasis were excluded. We categorized them into two groups - the pulmonary resection group and the systemic treatment only group. We compared the overall survival and progression-free survival between groups, and also analyzed the surgical modality, which includes single or multiple port surgery.
Results
The analysis included 44 esophageal squamous cell carcinoma patients with lung metastasis. Among these 44 patients, 14 patients have received pulmonary metastasectomy, and 30 patients received systemic treatment only. Patients who received pulmonary metastasectomy had significantly better overall survival (p < 0.0001) and progression-free survival (p = 0.038) than those who received only systemic treatment. The one-year overall survival and progression-free survival were 100% and 48% in patients receiving pulmonary metastatectomy, and 49% and 33% in patients receiving only systemic treatment. Among 14 patients receiving pulmonary metastatectomy, 10 patients underwent single port surgery. There were no postoperative complications in these 14 patients.
Conclusion
Esophageal squamous cell carcinoma patients with lung metastasis who can receive pulmonary metastasectomy have better prognosis, and some patients can achieve long-term survival. Our findings suggest that aggressive pulmonary metastasectomy is suggested in esophageal squamous cell carcinoma patients with if no contraindication.
Visual Abstract
Key question: How about the role of pulmonary metastasectomy in esophageal squamous cell carcinoma patients with isolated lung metastasis?
Key findings
Patients who received pulmonary metastasectomy had better overall survival and progression-free survival than those who received only systemic treatment.
Take Home Message
Esophageal cancer with isolated pulmonary metastasis can be treated aggressively with pulmonary metastasectomy if no contraindication.
Similar content being viewed by others
Introduction
Esophageal cancer usually has a poor prognosis, especially in patients who develop pulmonary metastasis. However, some studies showed that pulmonary metastasectomy can benefit selected patients. [1,2,3,4,5,6,7,8] In other cancers, such as colon cancer, sarcoma or head and neck cancer, pulmonary metastasectomy may provide obvious survival benefit.[4] Yotsukura Masaya et al. published a study about head and neck cancer with pulmonary metastasis which also provide survival benefit. [9] Thoracoscopic surgery may also benefit these patients as it is associated with less complications and easier recovery after surgery. Single port thoracoscopic surgery is a well-developed approach; however, currently, literature is sparse on the benefits of metastasectomy in patients diagnosed with esophageal cancer with pulmonary metastasis. We hypothesized that pulmonary metastasectomy would benefit these patients and reviewed our surgical outcomes.
Materials and methods
Patient population
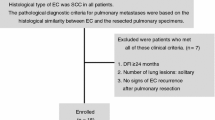
Patients diagnosed with esophageal cancer and pulmonary metastasis who received pulmonary metastasectomy from January 2014 to July 2020 at Kaohsiung Chang Gung Memorial Hospital, were reviewed retrospectively. We also reviewed the patients diagnosed with pulmonary metastasis without pulmonary resection in the same period and excluded those with extrapulmonary metastasis. All patients diagnosed with esophageal cancer were evaluated by a multidisciplinary team which included a thoracic surgeon, a medical oncologist, a radiation oncologist, a radiologist, and a gastroenterologist. Pre-treatment evaluation included the following procedures: a panendoscopy, contrast-enhanced chest computer tomography (CT), and endoscopic ultrasound and positron emission tomography/computed tomography (PET-CT) scan. The tumor node metastasis stage (TNM) was determined according to the 7th American Joint Committee on Cancer (AJCC) staging system. We excluded patients who refused treatment or were treated by radiotherapy alone. All patients received curative intent treatment, which included concurrent chemoradiotherapy and/or esophagectomy. This study was approved by the institutional review board of Chang Gung Memorial Hospital.
Thoracoscopic surgery
The patients received thoracoscopic surgery from two different surgeons. All patients underwent double lumen intubation with one lung ventilation, while pulmonary metastasectomy was performed. We used the same operative room setting for all patients, including team members and surgical devices.
Overall survival and progression free survival
These two outcomes were used to compare the results between single port surgery and multiple port surgery. We analyzed the result between the pulmonary metastasectomy group and systemic treatment group. Overall survival is defined as the period from initial diagnosis of pulmonary metastasis to the last contact date. If a patient was dead (regardless of the cause of death), we defined it as an event. If a patient was alive, we defined it as censored. Progression-free survival is defined as the period from initial diagnosis date of pulmonary metastasis to the date of disease progression or death. If the contrast-enhanced CT showed disease progression, we defined it as an event. If it showed stability or regression, we defined it as censored.
Statistical analysis
Statistical analysis was performed with the MedCalc Statistical Software version 19.4.0 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2020). A χ2 test or Fisher’s exact test were used to compare data between the two groups. For survival outcomes, the Kaplan–Meier method was used for univariate analysis, and the difference between survival curves was analyzed by a log-rank test. In a forward fashion, parameters were entered into a Cox regression model to analyze their relative prognostic importance. For all analyses, two-sided tests of significance were used with p < 0.05 considered significant.
Results
Patient characteristics
The baseline characteristics of these 44 patients were described in Table 1. Among these 44 patients, 14 patients have received pulmonary metastasectomies, and the other 30 patients only received systemic therapy. The mean age of these 14 patients receiving pulmonary metastasectomies was 60.3 years, and the median age was 61 years (range, 47–68 years). There were no significant difference between two groups in age, tumor grade, primary tumor location, performance status, and lung metastasis number.
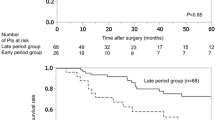
Overall survival and progression free survival
The association between clinical parameters with overall survival and progression-free survival were shown in Table 2. Patients with better performance status have superior overall survival and progression-free survival. Tumor grade also has an impact in progression-free survival with p value of 0.019. Pulmonary metastasectomy (resection) has significant impact in both overall survival (Fig. 1 A) and progression-free survival (Fig. 1B) with p values of < 0.0001 and 0.038. One-year overall survival between pulmonary metastasectomy group and systemic treatment group is 100% and 49.1%. One year progression free survival between pulmonary metastasectomy group and systemic treatment group is 48.0% and 33.3%. Furthermore, we found that metastatic Tumor numbers did not have impact in overall survival and progression free survival.
We also analyzed the multiple variables of survival with Cox proportional-hazards regression model in forward fashion. The result is listed in Table 3. The overall survival and progression-free survival decreased? by tumor grade of 2.86 (p = 0.0238) and 2.7968 (p = 0.0212). The overall survival increased with resection by 0.0781 (p = 0.0006). However, progression-free survival only decreased by resection of 0.3625 (p = 0.0402).
Thoracoscopic surgery
A total of 15 thoracoscopic procedures were performed in these 14 patients receiving pulmonary metastasectomies. One patient received thoracoscopic surgery twice, as pulmonary recurrence occurred after the first surgery. We tried to compare multiple port thoracoscopic surgery with single port thoracoscopic surgery in these 15 procedures. Pre-operative tumor grade showed differences in the two groups (p = 0.03). Other parameters such as tumor pathology, clinical TNM classification, and primary tumor location did not show significant differences. Surgery-related parameters, such as post -operative hospital stay, subjective pain scores, complications such as pneumonia or wound infection, curative resection, and surgery before treatment, did not show significant differences in the two groups (see Table 4).
Discussion
In this study, we analyzed thoracoscopic pulmonary metastasectomy results in patients with esophageal cancer. Single or multiple port thoracoscopic pulmonary metastasectomy did not demonstrate differences in surgical outcomes and complications. Average hospital stay was a little shorter in multiple port surgery because some single port surgeries were performed bilaterally. We did not find any differences in patients’ subjective pain ratings as well.
Previous some studies have shown that pulmonary metastasectomy may has a survival benefit in selected patients in esophageal cancer. [1,2,3, 5, 6, 8].
However, some literatures showed that pulmonary metastasectomy performed in patients with multiple pulmonary metastasis, did not show benefit in patients with esophageal cancer[1, 10]. However, in our series, pulmonary resection demonstrated a significant benefit in overall survival and progression-free survival. The one-year overall survival and progression-free survival were 100% and 48% in patients receiving pulmonary metastatectomy, and 49% and 33% in patients receiving only systemic treatment. Although, there is a selection bias, some patients with esophageal cancer could achieve long term survival in aggressive pulmonary resection even though pulmonary metastasis developed. In our opinion, pulmonary metastasectomy may provide precise tissue diagnosis and critical information to direct early decision-making for further palliative treatment such as chemotherapy, which could prolong overall and progression-free survival. Besides, pulmonary metastasectomy may reduce tumor burden dramatically in selected patients which may also benefit the overall survival and progression-free survival. Previous studies[11,12,13] have shown that patients with larger tumor burden may have worse efficiency of chemotherapy.
There are several limitations in our study. The limited number of patients in the pulmonary metastasectomy group could lead to selection bias. Future studies can enroll patients from other medical centers to reduce this. Large database case-controlled study with propensity score match may have better evidence to conduct this conclusion of “pulmonary resection have benefit for lung metastasis in patients with esophageal cancer.”
In conclusion, some patients with esophageal cancer could achieve long term survival in aggressive pulmonary resection even though pulmonary metastasis developed.
Data Availability
All data generated or analyzed during this study are included in this published article.
References
Hiyoshi Y, Morita M, Kawano H, Otsu H, Ando K, Ito S, Miyamoto Y, Sakamoto Y, Saeki H, Oki E, et al. Clinical significance of surgical resection for the recurrence of esophageal cancer after radical esophagectomy. Ann Surg Oncol. 2015;22:240–6.
Shiono S, Kawamura M, Sato T, Nakagawa K, Nakajima J, Yoshino I, Ikeda N, Horio H, Akiyama H, Kobayashi K. Disease-free interval length correlates to prognosis of patients who underwent metastasectomy for esophageal lung metastases. J Thorac Oncol. 2008;3:1046–9.
Kobayashi N, Kohno T, Haruta S, Fujimori S, Shinohara H, Ueno M, Udagawa H. Pulmonary metastasectomy secondary to esophageal carcinoma: Long-term survival and prognostic factors. Ann Surg Oncol. 2014;21(Suppl 3):365–9.
Petrella F, Diotti C, Rimessi A, Spaggiari L. Pulmonary metastasectomy: An overview. J Thorac disease. 2017;9:1291–8.
Chen F, Sato K, Sakai H, Miyahara R, Bando T, Okubo K, Hirata T, Date H. Pulmonary resection for metastasis from esophageal carcinoma. Interact Cardiovasc Thorac Surg. 2008;7:809–12.
Kanamori J, Aokage K, Hishida T, Yoshida J, Tsuboi M, Fujita T, Nagino M, Daiko H. The role of pulmonary resection in tumors metastatic from esophageal carcinoma. Jpn J Clin Oncol. 2017;47:25–31.
Schizas D, Lazaridis II, Moris D, Mastoraki A, Lazaridis LD, Tsilimigras DI, Charalampakis N, Liakakos T. The role of surgical treatment in isolated organ recurrence of esophageal cancer-a systematic review of the literature. World J Surg Oncol. 2018;16:55.
Kozu Y, Oh S, Takamochi K, Suzuki K. Surgical outcomes of pulmonary metastases from esophageal carcinoma diagnosed by both pathological and clinical criteria. Surg Today. 2015;45:1127–33.
Yotsukura M, Kinoshita T, Kohno M, Asakura K, Kamiyama I, Emoto K, Hayashi Y, Ohtsuka T. Survival predictors after resection of lung metastases of head or neck cancers. 2015.
Takemura M, Sakurai K, Takii M, Yoshida K. Metachronous pulmonary metastasis after radical esophagectomy for esophageal cancer: Prognosis and outcome. J Cardiothorac Surg. 2012;7:103–3.
Wang HM, Wang CH, Chen JS, Chang HK, Kiu MC, Liaw CC, Ng KT, Lai GM. Cisplatin and 5-fluorouracil as neoadjuvant chemotherapy: Predicting response in head and neck squamous cell cancer. J Formos Med Assoc. 1995;94:87–94.
Martinez A, Infante JR, Quiros J, Rayo JI, Serrano J, Moreno M, Jimenez P, Cobo A, Baena A, Baseline. (18)f-fdg pet/ct quantitative parameters as prognostic factors in esophageal squamous cell cancer. Rev Esp Med Nucl Imagen Mol (Engl Ed). 2022;41:164–70.
Li SH, Rau KM, Lu HI, Wang YM, Tien WY, Liang JL, Lin WC. Pre-treatment maximal oesophageal wall thickness is independently associated with response to chemoradiotherapy in patients with t3-4 oesophageal squamous cell carcinoma. Eur J Cardiothorac Surg. 2012;42:958–64.
Acknowledgements
We would like to thank Editage for providing language editing assistance.
Funding
This work was supported in part by grants from the National Science Council, Taiwan (MOST 111-2314-B-182A-030-) and Chang Gung Memorial Hospital (CORPG8M0341, CMRPG8M0901, and CMRPG8K1291-3).
Author information
Authors and Affiliations
Contributions
Conceptualization: Chien-Ming Lo. Data curation: Chien-Ming Lo. Formal Analysis: Chien-Ming Lo. Funding acquisition: Kai-Hao Chuang. Investigation: Kai-Hao Chuang. Methodology: Hsing-Hua Lai. Project administration: Chien-Ming Lo. Resources: Yu Chen, Li-Chun Chen. Software: Chien-Ming Lo. Supervision: Hung-I Lu. Validation: Yen-Hao Chen. Visualization: Chien-Ming Lo. Writing – original draft: Chien-Ming Lo. Writing – review & editing: Shau-Hsuan Li.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Institutional Review Board of Chang Gung Memorial Hospital. In the retrospective design, the requirement of informed consent was waived and the study protocol was approved by the Ethics Committee of Chang Gung Memorial Hospital (Institutional Review Board number:202100077B0). IRB NO.: 202100077B0.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lo, CM., Chuang, KH., Lai, HH. et al. Long-term survival after pulmonary metastasectomy in patients with esophageal squamous cell carcinoma with lung metastasis. J Cardiothorac Surg 17, 267 (2022). https://doi.org/10.1186/s13019-022-02017-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-02017-z