Abstract
Background
Tracheal papillomatosis is a relatively rare condition with limited data on successful treatment modalities. To our knowledge, this is the first report to describe a papilloma arising from an accessory bronchus. Furthermore, this case report demonstrates successful treatment with clinical and patient-centered improvements after use of Spray Cryotherapy.
Case presentation
A 71-year-old woman presented with one year history of recurrent fevers and intermittent hemoptysis. Imaging and video bronchoscopy revealed an obstructing papilloma of an accessory tracheal bronchus to the right upper lobe. She was treated with debridement followed by multiple cryotherapy treatments resulting in complete clinical and radiographic resolution of her post-obstructive pneumonia.
Conclusions
This case report not only supports existing literature on the use of cryotherapy for airway diseases but also presents a unique form of obstructing papilloma confined to an accessory bronchus, the only report of its kind based on extensive literature review.
Similar content being viewed by others
Introduction
Tracheal papillomatosis is characterized by papillomatous growth of the bronchial epithelium associated with Human Papilloma Virus (HPV). Occurring in either the larynx or trachea, this is a relatively rare condition with bimodal expression in children and adults in their 5th–6th decade [1]. In the adult population, incidence is estimated at about 18 in 1 million and, though low, there is a risk for transformation to squamous cell carcinoma (2%) [1]. Symptoms of tracheal papillomatosis are largely non-specific, ranging from dyspnea to hemoptysis. Several treatment modalities have been suggested in the literature including probe-directed cryotherapy, CO2 laser ablation, interferon-a injection, and surgical excision 1,2,3,4]. In this case, cryotherapy was elected as the preferred treatment modality. Given the involvement of an accessory bronchus, surgical resection would have been complex requiring lobectomy and tracheoplasty to obtain an R0 resection. In contrast, cryotherapy is a well-tolerated lung sparing outpatient procedure that can preserve quality of life, especially in patients with aberrant anatomy or compromised lung function. We elected to use the novel approach of trufreeze® Spray Cryotherapy ablation technology (Steris, Mentor, OH, US). This method of cryotherapy differs from traditional probe application, where direct contact with the probe is required and tissue removal is often the result. Spray cryotherapy allows for even application of cryogen without requiring direct contact with the probe, resulting in evenly distributed tissue damage and cell death. The resulting even distribution of treatment is desirable in dysplastic tissue. Furthermore, this patient’s anatomy lent itself well to this treatment modality since the angulation of the video bronchoscope accommodates the flexible cryo-spray catheter, making the lesion easily accessible. This patient had an accessory tracheal bronchus, a congenital tracheobronchial anomaly defined by a bronchus that arises superior to the carina with reported incidence of 0.2% [6]. To our knowledge, this is the first report to describe a papilloma arising from an accessory bronchus.
Case report
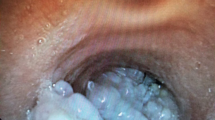
71-year-old lifelong nonsmoker with history of asthma and rheumatoid arthritis in good state of health presented to her pulmonologist with one year of cough, fevers, night sweats, and intermittent hemoptysis. She underwent CT scan of the chest which demonstrated a multiloculated density in the RUL (Figs. 1a and 2a). Diagnostic bronchoscopy revealed an obstructing mass extending into the tracheal lumen and involving an accessory bronchus to the RUL with no other airways involved. This mass was not apparent on her pre-operative imaging. The mass was extirpated with biopsy forceps which resulted in drainage of purulent material and subsequent visualization and patency of the accessory bronchus to the RUL. She completed a full course of oral antibiotics and one month later, she presented for scheduled surveillance bronchoscopy and cryotherapy. Residual papilloma within the accessory bronchus was noted and treated with cryotherapy using three five second treatments of liquid nitrogen (Fig. 3b). The patient had two subsequent treatments over the time span of 9 months, roughly three months between each treatment cycle, and has continued to undergo surveillance bronchoscopy. Now almost two years out from therapy, the patient has experienced complete resolution of her dyspnea and cough as a result of the cryotherapy treatments. She has maintained durable patency of her accessory bronchus evident on post treatment imaging (Figs. 1b and 2b) and surveillance bronchoscopy (Fig. 3c). Post treatment imaging also confirms resolution of post-obstructive atelectasis involving the right upper lobe. The unique presentation of an accessory bronchus in conjunction with papillomatous growth adds further complexity to the literature on this unique disease process.
Discussion
There have been several case reports describing success of various methods to treat recurrent respiratory papilloma as well as some retrospective studies. However, given the rarity of this condition, there have been no randomized control trials comparing efficacy of different treatment modalities. In our case, the degree of obstruction necessitated endoscopic excision followed by treating remaining tissue with cryotherapy to maintain patency of the airway. While cryotherapy was our treatment method of choice, there are several available options for ablating the remaining tissue endoscopically including laser ablation and electrocautery, but there is limited data comparing these modalities. Given the low risk for malignant transformation of airway papillomas, major lung resection with potential need for complex airway reconstruction may not be justified if effective, endoscopic treatment such as cryotherapy proves to be durable. The role of post treatment surveillance with outpatient bronchoscopy is well tolerated and repeat treatments could be offered as needed for local recurrence.
Regarding surgical management particularly in this patient, cryotherapy has provided a lung sparing treatment modality that otherwise would have necessitated upper lobectomy with partial tracheal resection and tracheoplasty to achieve negative margins. Use of cryotherapy is especially relevant in patients with compromised lung function who cannot tolerate lung resection. While our patient didn’t have compromised lung function at baseline, her unique anatomy made surgical excision more difficult, and cryotherapy offered a preferrable alternative.
There have been several articles published on adjuvant medical therapy, particularly bevacizumab, in patients with recurrent respiratory papillomatosis [7]. Research regarding intralesional or systemic application of these medications is ongoing, though promising preliminary results have been published 6,7,8]. Furthermore, a recent review article on biologic therapy for this disease remarked that Gardasil HPV vaccine not only acts as an adjuvant treatment modality, but also prevents this illness in a meaningful way that could reduce occurrence of this disease in most of the developing world [8]. Future investigation is needed, but our case report contributes to the growing body of data on successful treatment of tracheal papillomatosis and is the only publication we have identified referencing this disease process in a tracheal bronchus.
Availability of data and materials
Not applicable to this study.
References
Harris K, Chalhoub M. Tracheal papillomatosis: What do we know so far? Chron Respir Dis. 2011;8(4):233–5. https://doi.org/10.1177/1479972311416381.
Shai SE, Wang LL, Hung SC. Curing a patient of recurrent tracheal papillomatosis using laser ablation and adjuvant radiotherapy. Ann Thorac Surg. 2020;110(2):e91–3.
Best SR, Mohr M, Zur KB. Systemic bevacizumab for recurrent respiratory papillomatosis: a national survey. Laryngoscope. 2017;127(10):2225–9.
Rogers DJ, Ojha S, Maurer R, Hartnick CJ. Use of adjuvant intralesional bevacizumab for aggressive respiratory papillomatosis in children. JAMA Otolaryngol Head Neck Surg. 2013;139(5):496–501.
Ghaye B, Szapiro D, Fanchamps JM, Dondelinger RF. Congenital bronchial abnormalities revisited. RadioGraphics. 2001;21(1):105–19. https://doi.org/10.1148/radiographics.21.1.g01ja06105.
Benedict JJ, Derkay CS. Recurrent respiratory papillomatosis: a 2020 perspective. Laryngoscope Investig Otolaryngol. 2021;6(2):340–5. https://doi.org/10.1002/lio2.545.
Sidell DR, Balakrishnan K, Best SR, Zur K, Buckingham J, et al. Systemic bevacizumab for treatment of respiratory papillomatosis: international consensus statement. Laryngoscope. 2021;131(6):E1941–9. https://doi.org/10.1002/lary.29343.
Allen CT. Biologics for the treatment of recurrent respiratory papillomatosis. Otolaryngol Clin North Am. 2021;54(4):769–77. https://doi.org/10.1016/j.otc.2021.05.002.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
FS obtained the imaging and patient data and was also a major contributor to the manuscript. AA was the primary author of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable to this study.
Consent for publication
Consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Adams, A.E., Steiner, F.A. Use of cryotherapy to treat obstructing papilloma of an accessory tracheal bronchus: case report. J Cardiothorac Surg 17, 273 (2022). https://doi.org/10.1186/s13019-022-01977-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-01977-6