Abstract
Background
Minimally invasive aortic surgery is growing in popularity among surgeons. Although many clinical reports have proven both the safety and efficacy from a surgical point of view, there are few data regarding its impact on patients’ quality of life and whether there is a difference between ministernotomy and minithoracotomy from the patient perspective.
Methods
This prospective, questionnaire-based, nonrandomized study included 189 patients who underwent aortic valve replacement via a minimally invasive incision between May 2014 and December 2020 and completed at least 1 year of follow-up. The study uses the RAND SF 36-Item Health Survey 1.0 to assess and compare health-related quality of life between ministernotomy and minithoracotomy.
Results
There was a statistically significant improvement in the minithoracotomy group with regard to physical functioning, role limitation due to a physical problem, and social functioning (79.69 ± 20.72, 75.28 ± 26.52, 87.91 ± 16.98) compared to the ministernotomy group (70.31 ± 22.88, 58.59 ± 31.17, 66.15 ± 27.32) with p values (0.0036, 0.0001, < 0.0001), respectively.
Conclusions
Both minimally invasive aortic valve incisions positively impacted patient quality of life. The minithoracotomy incision showed significant improvements in physical capacity and successful patient re-engagement in daily physical and social activities. This, in turn, positively improved their general health status compared to the 1-year preoperative status.
Trial registration: This study was approved by the Research Ethics Committee (REC) at the Faculty of Medicine, Ain Shams University, under the number code (FWA 000017585, FAMSU R 91 /2021).
Similar content being viewed by others
Background
The trend toward minimally invasive surgery has extended into cardiac surgery to achieve better results for patients with the same quality as conventional median sternotomy. Aortic valve surgery has advanced significantly due to the widespread adoption of more minor invasive procedures and new technologies. Indeed, an increasing number of surgeons are treating aortic valve problems with smaller chest incisions to lessen the invasiveness of the surgical procedure while also improving clinical and cosmetic outcomes [1].
Traditionally, postcardiac surgery results were measured with classic clinical outcomes such as event freedom and overall survival. From the physician perspective, these outcomes are critical, but they may have disregarded other patient-related outcomes. As a result, the term quality of life was coined by patients [2].
Quality of life has been applied explicitly to those life concerns that are most influenced by health or illness in matters linked to health care, hence the term health-related quality of life (HRQL) [3].
HRQL evolved from the broader notion of overall quality of life and is, by definition, more focused on the components of life quality that are influenced or can be influenced directly by one's health state. Side effects of disease and treatment, treatment satisfaction, physical functioning and wellness, social functioning and life satisfaction, and mental health, including emotional wellbeing and cognitive functioning, are all examples of these factors [3].
The 36-item Short Form (36) Health Survey is a patient-reported health survey with 36 questions. The SF-36 has been thoroughly validated and comprises eight scaled scores that are the weighted sums of the items in each component. Each scale is converted to a 0–100 scale, assuming that each question is equally weighted. The lower the score is, the greater the degree of disability. The higher the score is, the less severe the disability; for example, a score of zero corresponds to a maximum disability, while a score of 100 corresponds to no disability. The eight sections are vitality, physical function, body discomfort, general health perceptions, physical role function, emotional role function, social role function, and mental health [4, 5].
This study aims to use the SF 36 questionnaire to compare the HRQL between two approaches for minimally invasive aortic valve replacement in patients.
Methods
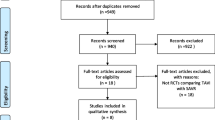
This prospective, questionnaire-based, nonrandomized study included all patients who underwent aortic valve replacement via a minimally invasive incision between May 2014 and December 2020.
Of the 260 previously reported patients [6], 189 were interviewed and completed the official validated Arabic version of the SF-36/RAND-36 questionnaire [7] Postoperative questionnaires were collected from those who completed at least 1 year of follow-up.
Retrospective data were collected from the registry and reanalyzed for the 189 patients who completed the questionnaire. These data included preoperative demographics, operative details, and the immediate postoperative course.
The ministernotomy group underwent a J-sternotomy from 1 cm above the angle of Luis to the 4th intercostal space. Cardiopulmonary bypass was achieved by means of central aorto-atrial cannulation. The minithoracotomy group underwent a right anterior thoracotomy via the 2nd or 3rd intercostal space. Cardiopulmonary bypass was achieved by peripheral femoral cannulation.
All surgical procedures were performed under moderate hypothermia 28–32 °C with antegrade cardioplegia.
This study was approved by the Research Ethics Committee (REC) at the Faculty of Medicine, Ain Shams University, under the number code (FWA 000017585, FAMSU R 91 /2021).
Statistical analysis
The scoring of the questionnaire followed the RAND 36-Item Health Survey 1.0. Precoded responses were given numeric values; the higher the value was, the more favorable the outcome. Numeric values range between 0 and 100, representing a percentage of the total possible score. Then, numeric values of the same scale are averaged together to create the final eight scale scores [8] Data are reported as the mean ± SD, and P values > 0.05, ≤ 0.05, and < 0.0001 were considered indicative of statistical nonsignificance, statistical significance, and high statistical significance, respectively.
Results
Both groups were comparable in terms of demographics, comorbidities, and preoperative echocardiographic data with no statistically significant differences between the groups (Table 1).
The ministernotomy group had more ill patients with NYHA classes III–IV (63 patients vs. 47 patients, p value 0.036), which was statistically significant (Table 1).
All 189 patients received mechanical valves as per the patients’ request and/or surgical preference. Other operative data, including total bypass and cross clamp times, are shown in Table 2, with significantly shorter times for the ministernotomy group (Table 2).
The postoperative course data are shown in Table 3
The questionnaire was completed by 189 patients, with 96 undergoing ministernotomy and the remaining 93 undergoing minithoracotomy.
Even though there was no statistically significant difference in how patients reported their general health status (P = 0.0532), the minithoracotomy group reported a statistically significant improvement in their health condition compared to a year prior (93.28 ± 11.74, 83.6 ± 22.6, P = 0.0003) (Table 4).
Physical functioning was significantly better for minithoracotomy than for ministernotomy (79.69 ± 20.72, 70.31 ± 22.88, P = 0.0036). In addition, the minithoracotomy group outperformed the ministernotomy group in regard to role limitation due to physical problems (75.28 ± 26.52, 58.59 ± 31.17, P = 0.0001) (Table 4).
In the minithoracotomy group, this was accompanied by a highly significant improvement in social functioning (87.91 ± 16.98, 66.15 ± 27.32, P 0.0001) (Table 4).
Other reported scales are shown in Table 4.
Discussion
Many studies have reported clinical outcomes of both minimally invasive approaches for aortic valve replacement with inconclusive and insufficient data to tip the balance in favor of one approach over the other [9].
From a surgeon’s perspective, ministernotomy patients had shorter clamp and total bypass times, and the procedure was less technically demanding with a shorter learning curve [10].
Ministernotomy is also associated with fewer pleural and pulmonary complications than minithoracotomy, with reduced pain perception. However, this is true only for the first 30 days post-hospital discharge, where recent data show pain scales to be the same after that time [11].
For several years, minimally invasive cardiac surgery outcomes have been reported as “hard” outcomes, such as mortality, complications, total bypass and cross-clamp times, and other technical aspects. Although these are very important from a clinician point of view, this disregards the patients’ perceptions of their life postsurgery, their physical capacity to perform daily activities, their ability to re-engage in sports they like, their emotional and psychological well-being and their overall social life [12].
Sicouri and colleagues compared the preoperative and postoperative quality of life for 24 consecutive patients who underwent minimally invasive aortic valve intervention at 1 and 3 months of follow-up. Similar to our report, they proved significant increases in their cohort’s functional physical capacity, energy, and general health after 3 months compared to the preoperative baseline [13].
Sternal stability is one of the important determinants in regaining postoperative physical activity. Unfortunately, many reports comparing ministernotomy to conventional sternotomy failed to show a significant difference in stability between the two “sternotomy” approaches [14].
Sternal integrity is crucial for faster respiratory recovery, early hospital discharge and physical functioning [15].
The physical functioning scale includes daily activity, including the ability to engage in vigorous activities such as running and weightlifting, to perform moderate activities or to carry groceries, to climb several flights of stairs, to walk several blocks, to bend, and to kneel, all of which are related to sternal stability. It was no surprise in our study that minithoracotomy patients outperformed ministernotomy patients, especially regarding weightlifting, bending and kneeling.
Compared to our previous report, where ministernotomy significantly outperformed minithoracotomy regarding postoperative pain, it seems that after 1 year, patients with minithoracotomy showed greater improvement than ministernotomy, yet the difference did not reach statistical significance ([6], Table 4). This is consistent with other reports of “no difference” in pain perception after 30 days and 1 year [11].
Emotional wellbeing includes postoperative anxiety, depression, and emotional stability. These have an impact on role limitations following cardiac surgery. Although the SF 36 has three scales that assess the “emotional wellbeing,” “the role limitation due to emotional problems,” and “social functioning,” it has no specific anxiety assessment tool like the Hospital Anxiety and Depression Scale (HADS).” However, both the work of Sicouri and colleagues and our work showed improvements in the anxiety scale score following minimally invasive aortic incisions; this was associated with better improvement in the minithoracotomy group [13]. Improvements in well-being mainly contributed to how the patients perceived their wounds; smaller hidden incisions with full sternal integrity were considered more aesthetically pleasing by the patients, especially female patients [16].
The safety and efficacy of minimally invasive aortic techniques have been proven, although there is insufficient data for a preference of one incision over the other, especially in terms of postoperative patient quality of life. More extensive studies are needed to conclude such a debate. Additionally, one must consider the quality of life post-TAVI as a highly competitive approach [17].
This study has the important limitation of lacking a preoperative questionnaire assessment to measure improvement from the preoperative period to the postoperative period, lacking randomization, being a single-center report, and lacking of a full sternotomy group as a control.
Conclusions
Minimally invasive aortic valve replacement is associated with improving patient quality of life. In addition, minithoracotomy is more closely associated with improved physical and social well-being and improved perception of general health and health change.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AVR:
-
Aortic valve replacement
- HRQL:
-
Health-related quality of life
- SF 36:
-
Short Form 36
- HADS:
-
Hospital Anxiety and Depression Scale
- TAVI:
-
Transcatheter aortic valve implantation
References
Nguyen TC, Terwelp MD, Thourani VH, Zhao Y, Ganim N, Hoffmann C, et al. Clinical trends in surgical, minimally invasive and transcatheter aortic valve replacement†. Eur J Cardiothorac Surg. 2017;51(6):1086–92.
Leidl R, Sintonen H, Abbühl B, Hoffmann C, von der Schulenburg J-M, König H-H. Do physicians accept quality of life and utility measurement? Eur J Health Econ (HEPAC). 2001;2(4):170–5.
Bergner M. Quality of life, health status, and clinical research. Med Care. 1989;27(3 Suppl):S148–56. https://doi.org/10.1097/00005650-198903001-00012.
-Item Short Form Survey from the RAND Medical Outcomes Study (Internet). RAND Corporation. (cited 2022 July 6). https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html
-Item Short form survey instrument (SF-36) (Internet). RAND Corporation. (cited 2022 July 6). https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/survey-instrument.html.
Mourad F, Abd Al Jawad M. Mini sternotomy and mini thoracotomy for aortic valve replacement: is there a difference?. Heart Surg Forum. 2021;24(5):E855-59. https://doi.org/10.1532/hsf.4029.
Rand Corporation (Internet). (cited 2022 July 6). https://www.rand.org/content/dam/rand/www/external/health/surveys_tools/mos/mos_core_36item_survey_arabic.pdf.
-Item Short Form Survey (SF-36) scoring instructions (Internet). RAND Corporation. (cited 2022 July 6). https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html.
Phan K, Xie A, Tsai YC, Black D, Di Eusanio M, Yan TD. Ministernotomy or minithoracotomy for minimally invasive aortic valve replacement: a Bayesian network meta-analysis. Ann Cardiothorac Surg. 2015;4(1):3–14. https://doi.org/10.3978/j.issn.2225-319X.2014.08.01.
Semsroth S, Matteucci Gothe R, Raith YR, de Brabandere K, Hanspeter E, Kilo J, et al. Comparison of two minimally invasive techniques and median sternotomy in aortic valve replacement. Ann Thorac Surg. 2017;104(3):877–83.
Bonacchi M, Dokollari A, Parise O, et al. Ministernotomy compared with right anterior minithoracotomy for aortic valve surgery. J Thorac Cardiovasc Surg. 2021;S0022-5223(21)00728-5. https://doi.org/10.1016/j.jtcvs.2021.03.125.
Rodríguez-Caulo EA, Guijarro-Contreras A, Otero-Forero J, et al. Quality of life, satisfaction and outcomes after ministernotomy versus full sternotomy isolated aortic valve replacement (QUALITY-AVR): study protocol for a randomised controlled trial. Trials. 2018;19(1):114. https://doi.org/10.1186/s13063-018-2486-x.
Sicouri S, Shah VN, Orlov CP, Buckley M, Dedeilia K, Plestis KA. Assessment of pain, anxiety and depression, and quality of life after minimally invasive aortic surgery. J Card Surg. 2021;36(3):886–93.
Detter C, Deuse T, Boehm DH, Reichenspurner H, Reichart B. Midterm results and quality of life after minimally invasive vs. conventional aortic valve replacement. Thorac Cardiovasc Surg. 2002;50(6):337–41.
Stoliński J, Musiał R, Plicner D, Fijorek K, Mędrzycki M, Andres J, et al. Respiratory functional status after conventional and minimally invasive aortic valve replacement surgery—a propensity score analysis. Pol J Cardio Thorac Surg. 2017;1:5–9.
Massetti M, Nataf P, Babatasi G, Khayat A. Cosmetic aspects in minimally invasive cardiac surgery. Eur J Cardio Thorac Surg. 1999;16(Supplement_2).
Murray MK, Hofmann E, De Rosa R, et al. Life beyond 5 Years after TAVI: Patients’ Perceived Health Status and Long-Term Outcome after Transcatheter Aortic Valve Implantation. J Interv Cardiol. 2019;2019:4292987. https://doi.org/10.1155/2019/4292987.
Acknowledgements
Not applicable
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors state that the study is self-funded.
Author information
Authors and Affiliations
Contributions
MA: Conception and design, editing of manuscript, data collection and analysis and revision of the manuscript. FM: Conception and design, editing of manuscript, data collection and analysis and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee (REC) at the Faculty of Medicine, Ain Shams University, under the number code (FWA 000017585, FAMSU R 91 /2021). Informed consent was obtained from all participants in this study.
Consent for publication
The study uses the official validated Arabic version of the 36-Item Short Form Survey (SF-36) developed at RAND as part of the Medical Outcomes Study. No changes were made to the recipient version, and no written permission was needed for the use of this health survey, as stated by the RAND corporation terms and conditions. https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/terms.html
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abd Al Jawad, M., Mourad, F. Measurement of health-related quality of life post aortic valve replacement via minimally invasive incisions. J Cardiothorac Surg 17, 208 (2022). https://doi.org/10.1186/s13019-022-01964-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-01964-x