Abstract
Background
The azygos lobe (AL) combined with partial anomalous pulmonary venous return (PAPVR) is comparatively uncommon as well as in radical surgery for right lung cancer.
Case presentation
We herein present an extremely rare case of lung cancer coexisting with AL and asymptomatic PAPVR, which was diagnosed with preoperative contrast three-dimensional reconstruction and received radical surgery by thoracoscopy. During the surgery, we preserved azygos vein successfully and found a split type of PAPVR in right upper pulmonary vein.
Conclusions
AL combined with PAPVR may cause confusion on the vascular separation and disconnection of the right pulmonary hilar. However, preoperative 3D reconstruction is more conducive to the correct performing of this type of surgery.
Similar content being viewed by others
Background
The azygos lobe (AL), caused by azygos vein (AV) migrating abnormally from thoracic wall to tracheobronchial angle, is a rare variantion in the right upper lobe (RUL) [1]. Partial anomalous pulmonary venous return (PAPVR) is a less uncommon congenital pulmonary venous anomaly that involves drainage of 1 to 3 pulmonary veins into the right-sided circulation [2]. The prevalence of the AL is 1.2% in CT scans while PAPVR is only 0.1–0.2% [3]. At present, there is no report on combination of such two type malformations as well as radical surgery for right lung cancer. Herein we present the case of lung cancer coexisting with AL and asymptomatic PAPVR, which was diagnosed by preoperative contrast three-dimensional reconstruction (3D- reconstruction) and the patient received radical surgery. During the surgery, we preserved AV successfully, and avoided massive hemorrhage. A split type of PAPVR, which is often confused with right middle pulmonary vein (RMV), was found in right upper pulmonary vein (RUV). Therefore, we have summarized prior experience regarding the aforementioned vascular malformations.
Case presentation
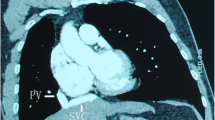
A 60-year-old male patient was admitted to our department due to incidental observation of a 10-mm partly solid nodule with spiculated sign and boundary unclear in RUL by annual physical CT scans (Fig. 1a). The tumour markers were elevated and malignant nodule was highly suspected, with squamous cell carcinoma antigen 1.70 ng/mL (reference 0–1.5 ng/mL), CYFRA21-1 3.99 ng/ml (reference 0–2.1 ng/mL). Pulmonary function tests were appropriate for lung resection; FVC 4.76L (Pred 131.4%), FEV1 3.89 L (Pred 97.4%) and the diffusion function (MVV) 164.97L/min (Pred 97.4%) without significant abnormalities of echocardiography. Contrast CT described abnormal courses of AV and separated the AL from RUL (Fig. 1b). Surprisingly, it is found that part of the pulmonary veins converged directly into the superior vena cava (Fig. 1c). Therefore, a preoperative 3D-reconstruction was performed which revealed AL combined a split type of PAPVR in RUV.
The RUV was divided into two branches with different diameters (Fig. 2). The thicker branch drained most of the anterior and atypical veins as well as part of the posterior veins (V1 + V3ac + V2b), which was identified as PAPVR with AV into the superior vena cava, while the other small branch (V2ac + V3b, represented by the below sRUV) drained into the left atrium at the proximal end of RMV.
Three-dimensional reconstruction of computed tomography. a Asterisk represents the dilated azygos vein(AV), the green part of the lung is azygos lobe (AL). b PAPVR, partial anomalous pulmonary venous return; sRUV, small branch of right upper pulmonary vein; RMV, right middle pulmonary vein, and the nodule in yellow
After the exclusion of distant metastasis, two-port thoracoscopic right upper lobectomy and mediastinal lymph node dissection were performed. During the surgery, the abnormally dilated AV connected to the superior vena cava, and crossed the apex of the lung from the ventral to the dorsal side (Fig. 3a). When the RUL was pulled down to the caudal side, the AL could be slipped out from the cavity consist of AV and pleuras smoothly (Fig. 3b). In the hilar, the thicker RUV branch draining into the superior vena cava was confirmed (Fig. 3c). After sutured the PAPVR of RUV by stapler, the pulmonary artery and bronchi of RUL were exposed as normal. For the hypoplastic of the fissure between the middle and upper lobe, we carefully separated sRUV, the veins of middle and lower lobe on mediastinal side. Under the premise of the RMV safety confirmed, the sRUV was ligated with silk thread and the fissure was separated by stapler. Shaped like a clover, the resected RUL combined AL was consistent with the 3D- reconstruction (Fig. 3f).
Intraoperative findings: a dilated azygos vein (AV) and azygos lobe (AL), b The cavity formed by invaginated parietal and visceral pleura with AV. c Partial anomalous pulmonary venous return (PAPVR) and AV drainage into superior vena cava. d, e The splited tppe of right upper pulmonary vein (RUV), sRUV, small branch of RUV; RMV, right middle pulmonary vein. f The resected right upper lobe combined AL shaped like a clove
The operation lasted 285 min with 50 ml blood loss. The postoperative course was uneventful. The drainage tube was removed on the Day 3 and the patient was discharged on the 10th postoperative day in good clinical condition. Pathological analysis showed lung adenocarcinoma without lymph nodes involved.
Discussion and conclusion
AL combined with PAPVR is a relatively rare variation in RUL, which is usually diagnosed incidentally on imaging in asymptomatic. The AL results from a failure of the normal migration of the AV from the thoracic wall to its usual position at the tracheobronchial angle, such that the fissure of the parietal and visceral pleura remain invaginated, which forming a cavity with the AV at its base [1, 4]. Furthermore, the potential cavity would not cause adhesion to the AL [5]. PAPVR is often associated with hypoplastic right lung and congenital heart disease, such as atrial septal defect, resulting in a left-to-right shunt. The patient’s clinical severity is determined by the degree of the left-to-right shunt [6]. Inadequate recognition of AL may easily injury AV leading to mass hemorrhage [4]. Lobectomy is the definitive treatment for lung cancer and PAPVR, and no hemodynamic problems occurred during and after the operation [7]. However, if PAPVR is located in different lobes and preserved wrongfully, inadequate resection may increase the left-to-right shunt flow and cause right-sided heart failure, increasing the risk of postoperative mortality [8].
In this case, AL was discovered accidentally with asymptomatic. To understand the variations of mediastinal vascular, we performed preoperative 3D reconstruction. The split RUV was found unexpectedly and partially as PAPVR. However the patient had no abnormalities of preoperative echocardiography without symptomatic, for the small degree of the left-to-right shunt. Intraoperatively, we found that the azygos fissure did not cause adhesions of AL. Hypoplastic of the fissure between the middle and upper lobe, the thicker branche of RUV identified as PAPVR may be misjudged as intact RUV, while the split small branche (sRUV) was confused with RMV (Fig. 3e), resulting in incomplete resection of RUV. Moreover, in this case, the PAPVR was mainly located in the RUV and lobectomy did not increase the flow of left-to-right shunt.
To sum up, if AL is detected prior to surgery, it should be aware that there may be other vascular variations. Therefore, contrast CT completion and vascular reconstruction might be a desirable option for AL surgery. The appearance of AL would not increase the difficulty in lobectomy, and AV could be preserved successfully. As for such vascular malformations as PAPVR, echocardiography should be performed to exclude congenital heart disease. Being familiar with anatomy of PAPVR is good for preventing accidental damage to the vessel, and especially when split type of RUV combined with hypoplasia fissure. Indeed, preoperative 3D reconstruction, which is safe and fast, is more conducive to the correct performing of this type surgery, for instance, the identification of small branch of RUV and preservation of RMV..
Availability of data and materials
Not applicable.
Abbreviations
- AL:
-
Azygos lobe
- AV:
-
Azygos vein
- PAPVR:
-
Partial anomalous pulmonary venous return
- RUL:
-
Right upper lobe
- RUV:
-
Right upper pulmonary vein
- RMV:
-
Right middle pulmonary vein
References
Bostanci K, Ozyurtkan MO, Polat MO, Batirel H, Lacin T, Yuksel M, Stamenovic D. Variations in pulmonary fissural anatomy: a medicolegal autopsy study of 256 cases. ANZ J Surg. 2020;90(4):608–11.
Ho ML, Bhalla S, Bierhals A, Gutierrez F. MDCT of partial anomalous pulmonary venous return (PAPVR) in adults. J Thorac Imaging. 2009;24(2):89–95.
Al-Mnayyis AA, Al-Alami Z, Altamimi N, Alawneh KZ, Aleshawi A. Azygos lobe: prevalence of an anatomical variant and its recognition among postgraduate physicians. Diagnostics. 2020;10(7):470.
Kauffman P, Wolosker N, de Campos JRM, Yazbek G, Jatene FB. Azygos lobe: a difficulty in video-assisted thoracic sympathectomy. Ann Thorac Surg. 2010;89(6):e57–9.
Arai H, Inui K, Kano K, Nishii T, Kaneko T, Mano H, Sasaki T, Masuda M. Lung cancer associated with an azygos lobe successfully treated with video-assisted thoracoscopic surgery. Asian J Endosc Surg. 2012;5(2):96–9.
Heineman DJ, van den Aardweg JG, Schreurs WH. A rare case of anomalous venous drainage of the right upper lobe. J Thorac Dis. 2015;7(10):E502–4.
Kawasaki H, Oshiro Y, Taira N, Furugen T, Ichi T, Yohena T, Kawabata T. Partial anomalous pulmonary venous connection coexisting with lung cancer: a case report and review of relevant cases from the literature. Ann Thorac Cardiovasc Surg. 2017;23(1):31–5.
Black MD, Shamji FM, Goldstein W, Sachs HJ. Pulmonary resection and contralateral anomalous venous drainage: a lethal combination. Ann Thorac Surg. 1992;53(4):689–91.
Acknowledgements
Not applicable.
Funding
This study was supported by the high-level hospital construction research project of Maoming People's Hospital, 2021 Maoming Science and Technology Special Fund Project (No. 2021186).
Author information
Authors and Affiliations
Contributions
(1) Information collection, analysis and writing: XS. (2) Surgical operation: ZL, JH. (3) Data collection: QH. (4) Imaging interpretation: NF. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Su, X., Huang, Q., Luo, Z. et al. A rare case of right upper lung cancer with azygos lobe and partial anomalous pulmonary venous return. J Cardiothorac Surg 17, 74 (2022). https://doi.org/10.1186/s13019-022-01823-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-01823-9