Abstract
Background
Delirium occurs frequently following cardiothoracic surgery, and infectious disease is an important risk factor for delirium. Surgery and cardiopulmonary bypass induce suppression of the immune response known as immunoparalysis. We aimed to investigate whether delirious patients had more pronounced immunoparalysis following cardiothoracic surgery than patients without delirium, to explain this delirium-infection association.
Methods
A prospective matched case–control study was performed in two university hospitals. Cytokine production (tumor necrosis factor (TNF)-α, interleukin (IL)-6, IL-8 and IL-10) of ex vivo lipopolysaccharide (LPS)-stimulated whole blood was analyzed in on-pump cardiothoracic surgery patients preoperatively, and at 5 timepoints up to 3 days after cardiothoracic surgery. Delirium was assessed by trained staff using two validated delirium scales and chart review.
Results
A total of 89 patients were screened of whom 14 delirious and 52 non-delirious patients were included. Ex vivo-stimulated production of TNF-α, IL-6, IL-8, and IL-10 was severely suppressed following cardiothoracic surgery compared to pre-surgery. Postoperative release of cytokines in non-delirious patients was attenuated by 84% [IQR: 13–93] for TNF-α, 95% [IQR: 78–98] for IL-6, and 69% [IQR: 55–81] for IL-10. The attenuation in ex vivo-stimulated production of these cytokines was not significantly different in patients with delirium compared to non-delirious patients (p > 0.10 for all cytokines).
Conclusions
The post-operative attenuation of ex vivo-stimulated production of pro- and anti-inflammatory cytokines was comparable between patients that developed delirium and those who remained delirium-free after on-pump cardiothoracic surgery. This finding suggests that immunoparalysis is not more common in cardiothoracic surgery patients with delirium compared to those without.
Similar content being viewed by others
Introduction
Delirium, characterized by an acute onset of inattention and other cognitive deficits, is a common postoperative complication in cardiothoracic surgery patients with an incidence of 10–20% [1]. Delirium is associated with multiple impaired outcomes, such as increased risk of dementia and prolonged admission with associated costs [2, 3]. Previous studies showed that various pro- and anti-inflammatory mediators may be associated with delirium [4,5,6], and these may also account for the development of immunoparalysis [7,8,9]. This suppression of the immune response has also been shown in other states to be associated with severe systemic inflammation, e.g. sepsis, and is associated with an increased susceptibility to secondary infections and morbidity [10]. Interestingly, patients with delirium appear to be prone to develop a secondary infection, but also an infectious disease is a risk factor for delirium [3]. The interplay between immunoparalysis and delirium has not been investigated previously.
Cardiothoracic surgery results in a systemic inflammatory response that could also lead to an innate immune response in the brain, called neuroinflammation [11] that may clinically express as delirium [12]. In addition, several studies have demonstrated that the use of cardiopulmonary bypass (CPB) disturbs the balance between pro- and anti-inflammatory responses, which may induce suppression of the immune responses postoperatively [8, 9, 13, 14].
Given the association between severe inflammation and the development of both delirium and immunoparalysis, we aimed to test the hypothesis that cardiac surgery-induced immunoparalysis is more pronounced in patients that develop delirium compared to those who do not.
Patients and methods
Study design and population
This multicenter, prospective, observational case–control study was performed in two University Medical Centers in the Netherlands: Radboud University Medical Center Nijmegen and University Medical Center Utrecht. The study was approved by the medical ethical committees in both centers and the need for informed consent was waived (study number 2012/297 and 12/471).
Eligible patients were aged 50 years or older, scheduled to undergo on-pump coronary artery bypass grafting (CABG) or single heart valve surgery, and delirium-free prior to the operation. Exclusion criteria were combined CABG with valve surgery for reason of group homogeneity, use of blood cardioplegia since this type of cardioplegia is associated with the development of postoperative neurological events [15], a pre-operative diagnosis consistent with immune suppression, inability to screen for delirium, pre-operative infection (determined by positive blood cultures or by administration of antibiotics), and a history of cognitive impairment or psychiatric illness for reason of group homogeneity. Dexamethasone was the only anti-inflammatory medication administrated to all patients during surgery as standard practice in both centers. Cefazolin was used for perioperative antibiotic prophylaxis.
Patients who developed delirium postoperatively were defined as ‘cases’ and patients who did not develop delirium served as ‘non-cases’. The group of cases was matched to non-cases for which propensity matching was used. Propensity scoring parameters were the following pre-operative and postoperative risk factors for delirium [3] gender, age, duration of surgery, extracorporeal circulation (ECC) time, aortic cross clamp (AOX) time, risk of death after cardiac surgery (European System for Cardiac Operative Risk Evaluation (EuroSCORE-II) and severity of illness score (Acute Physiology and Chronic Health Evaluation (APACHE)-II score).
Delirium diagnosis
Patients were assessed for delirium three times a day by trained nurses and researchers, using validated delirium assessment tools. In the Intensive Care Unit (ICU) the Confusion Assessment Method Intensive Care Unit (CAM-ICU) [16] was used, and on the cardiothoracic surgery ward the Delirium Observation Screening (DOS) scale [17] In order to increase the delirium detection rate, patients’ medical and nursing records were evaluated for delirium signs by the investigators and for delirium treatment. Delirium was defined as having a positive CAM-ICU assessment or a DOS score ≥ 3, use of haloperidol for no other reason than delirium treatment, or when there were typical signs of delirium registered without a positive delirium assessment.
Data collection and variables
Demographic and clinical data were obtained from electronic patient files. Blood was sampled from the central venous catheter, and if this was not possible, from an indwelling arterial catheter or by vena puncture at six time points: preoperatively, i.e. immediately after the induction of anesthesia, but prior to incision (T0), within one hour following post-operative ICU admission (T1), 6 h after ICU admission (T6), and 24 (T24), 48 (T48) and 72 h (T72) after cardiothoracic surgery.
Ex-vivo cytokine production
Immunoparalysis is characterized by attenuated cytokine production following ex vivo leukocyte stimulation with bacterial lipopolysaccharide (LPS) [7]. Lithium heparin (LH) anti-coagulated blood was obtained for ex vivo stimulation experiments, which were performed immediately after sampling. Leukocyte cytokine production capacity was determined by challenging whole blood from the patients with LPS ex vivo using an in-house developed system with prefilled tubes described in detail elsewhere [18]. Briefly, 0.5 mL of blood was added to tubes prefilled with 2 mL culture medium as negative control or 2 mL culture medium supplemented with Escherichia coli LPS (serotype O55:B5 (Sigma Aldrich, St Louis, MO, USA)), resulting in a final LPS concentration of 10 ng/mL. Cultures were incubated at 37 °C for 24 h, centrifuged, and supernatants were stored at − 80 °C until analysis. Concentrations of IL-6, IL-8, IL-10 and TNF-α, were determined batchwise by ELISA according to the manufacturer’s instructions (R&D systems, Minneapolis, MN, USA). Cytokine concentrations were normalized to monocyte counts since these cells are the main cytokine-producing cells in whole blood stimulation assays [19].
Statistical analysis
Demographic and patient characteristics were reported as means with standard deviation (SD), medians with interquartile range [IQR], or frequencies, depending on data distribution or occurrence. Accordingly, the Student’s t-test, Mann–Whitney U test, or Fischer’s exact test were used for group comparisons. Propensity scores were calculated using logistic regression analysis with ‘delirium’ or ‘no delirium’ as dependent variable and the delirium risk factors; age, APACHE-II score, AOX-time and EuroSCORE-II, as independent variables. Linear mixed effects models were used to study associations between the trajectory of log-transformed ex vivo cytokine concentrations and the occurrence of postoperative delirium. The time of sampling and the occurrence of delirium (yes/no) were analyzed as fixed effects, while subject ID was entered as random effect. Statistical significance was defined as a p value of < 0.05. Statistical analysis was performed using R, version 3.6.2 (http://www.R-project.org) software packages, and IBM SPSS Statistics 20 (IBM, NY, USA). Figures were created in GraphPad Prism 5.0 (Graphpad Software, San Diego, CA, USA).
Results
Patient characteristics
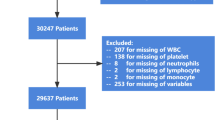
A total of 89 cardiothoracic surgery patients were screened of whom 18 (20%) developed delirium postoperatively. One non-delirious patient was excluded due to a postoperative cerebral infarction, twelve non-delirious and four delirious patients were excluded because of absent cytokine data. Subsequently 14 cases were matched with 52 non-delirious cases. Nine patients developed delirium within 24 h and five patients developed delirium within 72 h after surgery. No significant differences were found in demographic characteristics between delirious and non-delirious patients (Table 1). None of the participants were discharged on antipsychotic therapy.
Ex vivo cytokine production
Both groups showed a swift, profound and statistically significant attenuation of ex vivo-stimulated cytokine (TNF-α, IL-6, IL-8, and IL-10) production directly at ICU admission after surgery (Fig. 1). For all cytokines, the recovery of cytokine producing capacity started from 24 h onwards. However, TNF-α and IL-10 productions were still significantly suppressed 72 h after surgery compared to the first preoperative baseline measurement (− 44% [95% CI − 60 to − 21%], p < 0.001, and − 33% [95% CI − 51 to − 9%], p = 0.01, respectively).
Cytokine producing capacity in delirious and non-delirious patients, after whole blood ex vivo-stimulation with bacterial lipopolysaccharide. A Tumor necrosis factor-α (TNF-α). B Interleukin-6 (IL-6). C IL-8. D IL-10. Data are expressed as median concentration per 106 monocytes [interquartile range]. The blue dotted rectangles illustrate the duration of surgery. *p < 0.05; **p < 0.01; ***p < 0.001, NS: no significant change from baseline, according to linear mixed model analysis (LMM) with time of sampling and delirium occurrence as fixed variables, and subject ID as random effect. The p-values above each graph indicate no significant differences in the trajectories of ex vivo cytokine production between patients with and without postoperative delirium based on the LMM analysis, described above
Ex vivo-stimulated cytokine production pre- and postoperatively were not significantly different between delirious and non-delirious patients (difference between groups: TNF-α (p = 0.10), IL-6 (p = 0.42), IL-8.
(p = 0.13), and IL-10 (p = 0.87), Fig. 1).
Discussion
This study suggests that the extent of postoperative immunoparalysis is similar in patients that develop delirium, compared to those who do not. This indicates that immunoparalysis does not play an important role in the pathogenesis of delirium and presumably not in the development of secondary infections that are more frequently observed in patients suffering from delirium. In addition, our data confirms previous studies [14, 20,21,22,23] that the ex vivo-stimulated production of both pro-inflammatory (IL-6, IL-8 and TNF-α) and anti-inflammatory (IL-10) cytokines are severely suppressed following on-pump cardiothoracic surgery.
To our knowledge, it has not been studied previously to what extent ex vivo-stimulated cytokine production is attenuated in patients with and without delirium following cardiac surgery. Elevated plasma concentrations of TNF-α, IL-6 and IL-8 were reported to be associated with delirium [4,5,6, 24, 25]. In our study we did not analyze the in vivo plasma levels of pro- and anti-inflammatory cytokines since our aim was to determine whether or not immunoparalysis was more pronounced in patients with delirium after cardiothoracic surgery. Additionally, plasma concentrations of cytokines are not a sensitive hallmark of immunoparalysis [26].
This study has several limitations. First, although delirium was not diagnosed by an delirium expert such as a psychiatrist, neurologist or geriatrician, we used validated and frequently used delirium assessment tools for this purpose [16, 17], that were applied by trained (ICU) nurses and researchers. This was complemented by a detailed assessment of the medical and nursing files for notes on delirium and treatment with haloperidol in order not to miss any patients with delirium. Second is the relative small number of patients. However, with our standardized and robust methodology of ex vivo immunostimulation, combined with our matched case–control design, we were able to find a homogenous immune response with small margin of error between patients with and without delirium. Based on our data, we do not expect that a larger number of patients would likely change our results. Third, in the current study all patients were treated with dexamethasone per-operatively, while dexamethasone inhibits LPS-stimulated production of TNF-α, IL-6, IL-8 and IL-10 [27,28,29]. However, previous research demonstrated that immunoparalysis occurs after cardiothoracic surgery irrespective of corticosteroids use [14, 20,21,22,23]. Finally, the incidence of secondary infections after cardiac surgery is low [30, 31], and the power of this cohort was insufficient to analyze associations between delirium, secondary infections and immunoparalysis. This renders us unable to draw conclusions on whether or not immunoparalysis is involved in the pathogenesis of secondary infections that are more frequently observed in patients suffering from delirium. Alternatively, acute malnutrition, dehydration and aspiration pneumonia are common in delirious patients and may explain the increased susceptibility to secondary infections in delirium [32].
Conclusion
The time-course of ex vivo-stimulated production of pro- and anti-inflammatory cytokines was comparable between delirious and non-delirious patients in on-pump post cardiothoracic surgery patients. This finding indicates that immunoparalysis is not more pronounced in cardiothoracic surgery patients with delirium than in those without.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AOX:
-
Aortic cross clamp
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass grafting
- CAM-ICU:
-
Confusion Assessment Method Intensive Care Unit
- CPB:
-
Cardiopulmonary bypass
- DOS:
-
Delirium Observation Screening
- ECC:
-
Extracorporeal circulation
- EuroSCORE-II score:
-
European System for Cardiac Operative Risk Evaluation
- ICU:
-
Intensive Care Unit
- IL:
-
Interleukin
- IQR:
-
Interquartile range
- LPS:
-
Lipopolysaccharide
- LH:
-
Lithium heparin
- N/A:
-
Not applicable
- SD:
-
Standard deviation
- TNF:
-
Tumor necrosis factor
References
Sandiego CM, Gallezot JD, Pittman B, Nabulsi N, Lim K, Lin SF, et al. Imaging robust microglial activation after lipopolysaccharide administration in humans with PET. Proc Natl Acad Sci USA. 2015;112(40):12468–73.
van den Boogaard M, Schoonhoven L, Evers AW, van der Hoeven JG, van Achterberg T, Pickkers P. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. 2012;40(1):112–8.
Koster S, Hensens AG, Schuurmans MJ, van der Palen J. Risk factors of delirium after cardiac surgery: a systematic review. Eur J Cardiovasc Nurs. 2011;10(4):197–204.
van den Boogaard M, Kox M, Quinn KL, van Achterberg T, van der Hoeven JG, Schoonhoven L, et al. Biomarkers associated with delirium in critically ill patients and their relation with long-term subjective cognitive dysfunction; indications for different pathways governing delirium in inflamed and noninflamed patients. Crit Care. 2011;15(6):R297.
van Munster BC, Korevaar JC, Zwinderman AH, Levi M, Wiersinga WJ, De Rooij SE. Time-course of cytokines during delirium in elderly patients with hip fractures. J Am Geriatr Soc. 2008;56(9):1704–9.
de Rooij SE, van Munster BC, Korevaar JC, Levi M. Cytokines and acute phase response in delirium. J Psychosom Res. 2007;62(5):521–5.
Leentjens J, Kox M, Koch RM, Preijers F, Joosten LA, van der Hoeven JG, et al. Reversal of immunoparalysis in humans in vivo: a double-blind, placebo-controlled, randomized pilot study. Am J Respir Crit Care Med. 2012;186(9):838–45.
Gaudriot B, Uhel F, Gregoire M, Gacouin A, Biedermann S, Roisne A, et al. Immune dysfunction after cardiac surgery with cardiopulmonary bypass: beneficial effects of maintaining mechanical ventilation. Shock. 2015;44(3):228–33.
McBride WT, Armstrong MA, Crockard AD, McMurray TJ, Rea JM. Cytokine balance and immunosuppressive changes at cardiac surgery: contrasting response between patients and isolated CPB circuits. Br J Anaesth. 1995;75(6):724–33.
Hamers L, Kox M, Pickkers P. Sepsis-induced immunoparalysis: mechanisms, markers, and treatment options. Minerva Anestesiol. 2015;81(4):426–39.
Hovens IB, Schoemaker RG, van der Zee EA, Heineman E, Izaks GJ, van Leeuwen BL. Thinking through postoperative cognitive dysfunction: How to bridge the gap between clinical and pre-clinical perspectives. Brain Behav Immun. 2012;26(7):1169–79.
van Gool WA, van de Beek D, Eikelenboom P. Systemic infection and delirium: when cytokines and acetylcholine collide. Lancet. 2010;375(9716):773–5.
Cornell TT, Sun L, Hall MW, Gurney JG, Ashbrook MJ, Ohye RG, et al. Clinical implications and molecular mechanisms of immunoparalysis after cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2012;143(5):1160-6.e1.
Allen ML, Hoschtitzky JA, Peters MJ, Elliott M, Goldman A, James I, et al. Interleukin-10 and its role in clinical immunoparalysis following pediatric cardiac surgery. Crit Care Med. 2006;34(10):2658–65.
Martin TD, Craver JM, Gott JP, Weintraub WS, Ramsay J, Mora CT, et al. Prospective, randomized trial of retrograde warm blood cardioplegia: myocardial benefit and neurologic threat. Ann Thorac Surg. 1994;57(2):298–302 (discussion-4).
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001;29(7):1370–9.
Schuurmans MJ, Shortridge-Baggett LM, Duursma SA. The Delirium Observation Screening Scale: a screening instrument for delirium. Res Theory Nurs Pract. 2003;17(1):31–50.
Kox M, Vrouwenvelder MQ, Pompe JC, van der Hoeven JG, Pickkers P, Hoedemaekers CW. The effects of brain injury on heart rate variability and the innate immune response in critically ill patients. J Neurotrauma. 2012;29(5):747–55.
Dinarello CA. Interleukin-1 and interleukin-1 antagonism. Blood. 1991;77(8):1627–52.
Dehoux MS, Hernot S, Asehnoune K, Boutten A, Paquin S, Leçon-Malas V, et al. Cardiopulmonary bypass decreases cytokine production in lipopolysaccharide-stimulated whole blood cells: roles of interleukin-10 and the extracorporeal circuit. Crit Care Med. 2000;28(6):1721–7.
Börgermann J, Friedrich I, Flohé S, Spillner J, Majetschak M, Kuss O, et al. Tumor necrosis factor-alpha production in whole blood after cardiopulmonary bypass: downregulation caused by circulating cytokine-inhibitory activities. J Thorac Cardiovasc Surg. 2002;124(3):608–17.
de Jong PR, Schadenberg AW, van den Broek T, Beekman JM, van Wijk F, Coffer PJ, et al. STAT3 regulates monocyte TNF-alpha production in systemic inflammation caused by cardiac surgery with cardiopulmonary bypass. PLoS ONE. 2012;7(4):e35070.
Franke A, Lante W, Kollig E, Markewitz A. A comparison of monocyte counts and ex vivo and in vitro monocyte cytokine production after major surgical trauma. J Surg Res. 2009;154(1):91–8.
van Munster BC, Bisschop PH, Zwinderman AH, Korevaar JC, Endert E, Wiersinga WJ, et al. Cortisol, interleukins and S100B in delirium in the elderly. Brain Cogn. 2010;74(1):18–23.
Kazmierski J, Banys A, Latek J, Bourke J, Jaszewski R. Raised IL-2 and TNF-α concentrations are associated with postoperative delirium in patients undergoing coronary-artery bypass graft surgery. Int Psychogeriatr. 2014;26(5):845–55.
Leentjens J, Kox M, van der Hoeven JG, Netea MG, Pickkers P. Immunotherapy for the adjunctive treatment of sepsis: from immunosuppression to immunostimulation. Time for a paradigm change? Am J Respir Crit Care Med. 2013;187(12):1287–93.
Meng A, Wang B, Zhang X, Qi N, Liu D, Wu J. Additive Suppression of LPS-Induced IL-10 and TNF-α by Pre-treatment of Dexamethasone and SB203580 in a Murine Alveolar Macrophage Cell Line (MH-S). Inflammation. 2015;38(3):1260–6.
Bessler H, Mendel C, Straussberg R, Gurary N, Aloni D, Sirota L. Effects of dexamethasone on IL-1beta, IL-6, and TNF-alpha production by mononuclear cells of newborns and adults. Biol Neonate. 1999;75(4):225–33.
Giamarellos-Bourboulis EJ, Dimopoulou I, Kotanidou A, Livaditi O, Pelekanou A, Tsagarakis S, et al. Ex-vivo effect of dexamethasone on cytokine production from whole blood of septic patients: correlation with disease severity. Cytokine. 2010;49(1):89–94.
Chen LF, Arduino JM, Sheng S, Muhlbaier LH, Kanafani ZA, Harris AD, et al. Epidemiology and outcome of major postoperative infections following cardiac surgery: risk factors and impact of pathogen type. Am J Infect Control. 2012;40(10):963–8.
Robich MP, Sabik JF 3rd, Houghtaling PL, Kelava M, Gordon S, Blackstone EH, et al. Prolonged effect of postoperative infectious complications on survival after cardiac surgery. Ann Thorac Surg. 2015;99(5):1591–9.
Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc. 2017;65(5):1026–33.
Acknowledgements
The authors thank all ICU-nurses and physicians in the participating centers.
Funding
Dr. W.F. Abdo and this study were supported by a research grant from the Netherlands Organization for Health Research and Development (ZonMw Clinical Fellowship Grant 90715610). This funding agency had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
SC, AJCS, WM, WFA, PP, MvdB contributed to the design of the study. SC, EW, JG, MFL collected the data. APvT and SC analyzed the data and drafted the manuscript with MvdB, WFA and PP. All authors were involved in the editing of the manuscript, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the medical ethics committees in both centers (CMO Region Arnhem-Nijmegen 2012/297 and METC Utrecht 12/471) and the need for informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
CheheiliSobbi, S., Peters van Ton, A.M., Wesselink, E.M. et al. Case–control study on the interplay between immunoparalysis and delirium after cardiac surgery. J Cardiothorac Surg 16, 239 (2021). https://doi.org/10.1186/s13019-021-01627-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01627-3