Abstract
Background
The DeBakey classification divides Stanford acute type A aortic dissection (ATAAD) into DeBakey type I (D1) and type II (D2) according to the extent of acute aortic dissection (AAD). This retrospective study aimed to compare the early and late outcomes of D1-AAD and D2-AAD through a propensity score-matched analysis.
Methods
Between January 2009 and April 2020, 599 consecutive patients underwent ATAAD repair at our institution, and were dichotomized into D1 (n = 543; 90.7%) and D2 (n = 56; 9.3%) groups. Propensity scoring was performed with a 1:1 ratio, resulting in a matched cohort of 56 patients per group. The clinical features, postoperative complications, 5-year cumulative survival and freedom from reoperation rates were compared.
Results
In the overall cohort, the D1 group had a lower rate of preoperative shock and more aortic arch replacement with longer cardiopulmonary bypass time. The D1 group had a higher in-hospital mortality rate than the D2 group in overall (15.8% vs 5.4%; P = 0.036) and matched cohorts (19.6% vs 5.4%; P = 0.022). For patients that survived to discharge, the D1 and D2 groups demonstrated similar 5-year survival rates in overall (77.0% vs 85.2%; P = 0.378) and matched cohorts (79.1% vs 85.2%; P = 0.425). The 5-year freedom from reoperation rates for D1 and D2 groups were 80.0% and 97.1% in overall cohort (P = 0.011), and 93.6% and 97.1% in matched cohort (P = 0.474), respectively.
Conclusions
Patients with D1-AAD had a higher risk of in-hospital mortality than those with D2-AAD. However, for patients who survived to discharge, the 5-year survival rates were comparable between both groups.
Similar content being viewed by others
Introduction
Acute aortic dissection (AAD) is a cardiovascular emergency associated with high morbidity and mortality rates [1, 2]. The Stanford and DeBakey classifications are commonly used to determine the extent of the dissected aortic segment [3, 4]. Stanford acute type A aortic dissection (ATAAD) requires prompt surgical treatment for life-saving and accounts for 62%–67% of the entire AAD population according to the International Registry of Acute Aortic Dissection database [2, 5]. ATAAD can be divided into DeBakey type I (D1) and type II (D2) based on whether the dissected aorta is confined to the ascending portion only or extends to the aortic arch and descending aorta. In previous studies, D1-AAD was usually associated with inferior survival rates and a higher aortic reintervention probability compared to D2-AAD [6, 7]. However, disparities in regard to clinical presentation, preoperative condition, and aortic repair procedures commonly exist between patients with D1-AAD and D2-AAD owing to the different complexities of aortic anatomy and involved end-organs. Therefore, some bias among patient selection might have affected the reliability of previous outcome analyses. In the present study, we performed a retrospective propensity score-matched analysis of the database from an individual aortic surgery center and compared the individual characteristics and early and late outcomes of patients who underwent surgical repair for D1-AAD and D2-AAD.
Materials and methods
Patient enrollment and preoperative management
The study protocol was conducted by the approval of the Institutional Review Board of Chang Gung Medical Foundation (approval number 202001566B0). The requirement for informed consent was waived due to the retrospective nature of the study. A total of 599 consecutive adult patients underwent emergency ATAAD repair at this institution between January 2009 and April 2020. All patients were diagnosed via helical computed tomography in the emergency department, and the extent of aortic dissection was analyzed. The 599 included patients were dichotomized into D1 (n = 543; 90.7%) and D2 groups (n = 56; 9.3%) based on the DeBakey classification (Fig. 1). The annual cases of the overall cohort, D1, and D2 groups during the study period are illustrated in Fig. 2. When the diagnosis of ATAAD was confirmed, patients were emergently transferred to the operating room within 30 min. If patients presented with hypertension or tachycardia before surgery, their hemodynamics were stabilized with intravenous beta-blockers to maintain systolic blood pressure (SBP) < 120 mmHg and a heart rate of 60–70 bpm, according to the established guidelines [8]. If patients presented with shock status, medical resuscitation and surgical rescue procedures were applied according to the standardized protocols previously reported by this institute [9, 10].
ATAAD repair procedures and postoperative care
The technical aspects of aortic repair procedures were detailed in previous studies [11, 12]. Double artery cannulation using a combination of right axillary and femoral arterial access and the antegrade cerebral perfusion (ACP) strategy were preferably implemented for patients who presented with relatively stable preoperative condition. Otherwise, isolated femoral artery cannulation with retrograde cerebral perfusion (RCP) was preferred for patients with unstable hemodynamics. Following sternotomy, the right atrium or vena cava was cannulated and cardiopulmonary bypass (CPB) with deep hypothermia was initiated. In general, the dissected aorta was replaced with a Dacron prosthetic graft based on the location of the major entry tear and preoperative presentation. The tubular ascending aorta (AsAo) was routinely replaced with aortic valve resuspension, and the proximal anastomosis was usually performed first, followed by open distal anastomosis under circulatory arrest. All graft-aorta anastomoses were reinforced with Teflon felt. During circulatory arrest, the femoral arterial flow was temporarily suspended and selective ACP through the right axillary artery or RCP through the superior vena cava was performed. Concomitant aortic root replacement with a composite Valsalva graft was performed if the extent of aortic dissection involved the aortic root and was complicated with severe aortic regurgitation. After undergoing ATAAD repair, all patients were transferred to a specialized cardiovascular intensive care unit for further treatment and observation. The ventilator-weaning protocol was initiated at 12–24 h after surgery if unstable hemodynamics, persistent arrhythmia, signs of organ malperfusion, and active bleeding were not observed.
Statistical analyses
Statistical analyses were performed using SPSS for Windows (version 22.0; IBM Corp., Armonk, NY, USA). Data are presented as means ± standard deviation for numerical variables and as numbers and percentages for categorical variables. To compare the intergroup disparities between the D1 and D2 groups, we used the independent t-test for numerical variables and the chi-square or Fisher’s exact test for categorical variables, respectively. A propensity score–matched cohort with a 1:1 ratio was constructed to adjust for baseline differences and to reduce confounding variables. Propensity scores were calculated involving the following preoperative and operative variables with significant intergroup differences: age, sex, SBP, SBP < 90 mmHg, intubation, hemopericardium, cardiac tamponade, malperfusion, axillary artery cannulation, entry tear excision, isolated AsAo replacement, arch replacement, partial arch replacement, total arch replacement, CPB time, aortic clamp time, circulatory arrest time, ACP, and RCP. After a propensity score-matching, a matched cohort of 56 patients per group was created. A multivariate logistic regression analysis was performed to identify the independent risk factors of in-hospital mortality. The variables for the multivariate logistic regression analysis were selected from those with a P < 0.05 in the univariate logistic regression analysis. The Kaplan–Meier method was used to estimate the 5-year cumulative survival and freedom from aortic reoperation rates of the two groups, which were compared using the log-rank test. For all analyses, statistical significance was set at P < 0.05.
Results
Patient demographics
As illustrated in Table 1, the D1 group was comprised of younger patients and fewer female patients than in the D2 group. In terms of preoperative conditions, preoperative shock (SBP < 90 mmHg; 21.5% vs 37.5%; P = 0.007) and intubation (5.3% vs 14.3%; P = 0.008) occurred less frequently in the D1 group. As for clinical presentation, the D1 group had lower rates of hemopericardium (29.7% vs 66.1%; P < 0.001) and cardiac tamponade (10.5% vs 30.4%; P < 0.001), but a higher rate of preoperative malperfusion (17.1% vs 5.4%; P = 0.022). All preoperative factors with significant intergroup differences were homogenized after propensity score-matching.
Surgical information
Table 2 showed detailed information regarding surgical variables. The femoral artery was the most commonly used vascular access of cannulation for > 95% of patients in both groups. More patients in the D1 group underwent additional axillary artery cannulation (88.6% vs 76.8%; P = 0.011) and the ACP strategy (90.2% vs 76.8%; P = 0.002) than in the D2 group. A higher rate of aortic arch replacement was observed in the D1 group (33.9% vs 5.4%; P < 0.001); however, the D1 group had a lower rate of entry tear excision (71.8% vs 96.4%; P < 0.001) compared to the D2 group. In the D2 group, 3 patients underwent 1/3 arch replacement with the innominate artery reimplantation because isolated AsAo replacement cannot be performed securely; one patient had extensive calcification of AsAo and proximal aortic arch and 2 had aneurysmal dilatation at distal AsAo. The time spans of CPB, aortic cross-clamping, and circulatory arrest were generally longer in the D1 group. All intraoperative factors with significant intergroup differences were homogenized after propensity score-matching.
Postoperative complications
As Table 3 illustrates, the D1 group had a higher in-hospital mortality rate than the D2 group in the overall (15.8% vs 5.4%; P = 0.036) and propensity-matched cohorts (19.6% vs 5.4%; P = 0.022). In addition, postoperative malperfusion-related complications occurred more frequently in the D1 group before (24.3% vs 12.5%; P = 0.046) and after (30.4% vs 12.5%; P = 0.021) propensity-matching. A prolonged hospital stay in the D1 group was found in the overall cohort (25.6 ± 31.1 vs 19.0 ± 13.3 days; P = 0.004), but the statistical significance was not reached in the propensity-matched cohort (26.5 ± 26.5 vs 19.0 ± 13.3 days; P = 0.064).
Risk factors associated with in-hospital mortality
Table 4 shows the logistic regression analyses results for in-hospital mortality in patients undergoing ATAAD repair based on the overall and propensity-matched cohorts, respectively. Eight independent risk factors for in-hospital mortality were identified in the overall cohort: D1-AAD, preoperative estimated glomerular filtration rate, preoperative intubation, prolonged CPB, aortic cross-clamping, and circulatory arrest times, RCP, and intraoperative ECMO support. Three independent risk factors for in-hospital mortality were identified in the propensity-matched cohort: D1-AAD, preoperative intubation, and RCP.
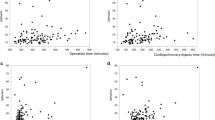
Cumulative 5-year survival and freedom from reoperation rates
Follow-up was completed for all patients with an average of 4.3 ± 3.4 years (median, 3.7; range, 0.1–11.8 years). As illustrated in Fig. 3, the 5-year cumulative survival rates for patients who survived to discharge were similar in D1 and D2 groups among the overall (77.0% vs 85.2%; P = 0.378) (Fig. 3a) and propensity-matched cohorts (79.1% vs 85.2%; P = 0.425) (Fig. 3b). In regard to the aspect of aortic reoperation, D1 group had a lower 5-year freedom from aortic reoperation rate compared to D2 group in the overall cohort (80.0% vs 97.1%; P = 0.011) (Fig. 4a). However, the freedom from aortic reoperation rates were similar for the two groups after propensity-matching (93.6% vs 97.1%; P = 0.474) (Fig. 4b).
Discussion
Patients with D1-AAD were associated with inferior outcomes compared to those with D2-AAD in the previous literature [6, 7, 13]. However, great differences in preoperative and operative characteristics between D1-AAD and D2-AAD commonly exist because of the nature of different vascular anatomy. In this study, propensity score-matching was conducted to reduce the potential bias caused by confounding factors. For 599 patients who underwent aortic repair for ATAAD during the study period, 543 and 56 patients were classified as the D1 and D2 groups, respectively. A matched cohort of 56 patients per group was created. Regarding preoperative condition, higher risks of shock and cardiac tamponade in the D2 group and a higher risk of organ malperfusion in the D1 group were observed before propensity-matching. Furthermore, a more aggressive aortic arch repair strategy with, however, a lower rate of entry tear resection was observed in the D1 group. The D1 group had a significantly higher in-hospital mortality rate than the D2 group, and D1-AAD represented an independent risk factor for in-hospital mortality either before or after propensity-matching. In contrast, for patients who survived to hospital discharge, the D1 and D2 groups revealed similar 5-year survival rates in both the overall and propensity-matched cohorts.
Although all preoperative and intraoperative factors were homogenized by propensity-matching, the D1 group had higher rates of in-hospital mortality and malperfusion-related complications, which were consistent with the results of the overall cohort. There are several interpretations to our findings. First, organ malperfusion observed in AAD is correlated with its complex anatomic interactions between the true lumen and false lumen along the dissected aorta. These anatomic interactions can be dynamic during aortic repair surgery and are potentially affected by the surgical procedure itself. The dissected aortic segment in D2-AAD is limited to the AsAo and, theoretically, no residual dissection exists after aortic repair surgery. In contrast, complications may arise from the residual dissected arch and descending thoracic aorta in D1-AAD, especially when entry tear resection is not achieved and the false lumen remains patent. Furthermore, a dissected branch vessel without preoperative malperfusion symptoms may not maintain adequate perfusion to the supplied organ during CPB and circulatory arrest, which render a different circulation pattern compared to the normal physiology. Second, in the D1 group, approximately 30% of patients had postoperative malperfusion-related complications and > 50% (10/17) of these complications were brain infarctions. In the present study, the ACP strategy was used for only 74.1% of patients in the propensity-matched cohort. As reported by Perreas et al., ACP during the ascending and aortic arch surgical procedures, including ATAAD repair, is associated with a decreased risk of all types of neurological complications and trends toward decreased 30-day and mid-term mortality rates in comparison with RCP [14]. Therefore, we suggest that this modality may be applied more aggressively to reduce cerebrovascular complications, especially among patients with D1-AAD. Furthermore, compared to D1-AAD, extensive manipulation of the aortic arch is usually unnecessary during aortic repair of D2-AAD. This conservative manipulation of the aortic arch may reduce the potential risks of iatrogenic injury to branch vessels and related complications. In addition, the second main cause of postoperative malperfusion was acute renal failure. At this institute, if acute renal failure develops after ATAAD surgery, the renal replacement therapy is promptly implemented to reduce the negative impact of fluid overload, metabolic acidosis, and electrolyte imbalance according to the Acute Kidney Injury Network criteria [15]. However, in several studies, the occurrence of acute renal failure after ATAAD surgery revealed a major end-organ malperfusion, which indicated inadequate systemic perfusion and was correlated with inferior early and late survival [16, 17]. Therefore, once acute renal failure develops, the patient should be cautiously re-evaluated for hemodynamic targets, cardiopulmonary function perseverance, and systemic organ perfusion. Finally, among patients with branch vessel dissection with residual false lumen patency, a more aggressive strategy may also be applied for detecting and treating postoperative malperfusion-related complications early.
As reported by Kohl et al., D1-AAD and D2-AAD yielded similar late survival rates for patients who survived to index hospitalization discharge [13]. Similar outcomes were observed in the present study; patients who survived to discharge in the D1 and D2 groups had comparable 5-year survival rates in both of the overall cohort and propensity-matched cohort. In contrast, the D2 group had a higher freedom from aortic reoperation rate in the overall cohort, but this advantage was attenuated in the propensity-matched cohort. We suggest that this finding is highly correlated with the homogenized aortic repair procedures and entry tear excision rates. As reported by Inoue and Kimura et al., residual primary entry tears and patent false lumen were significant risk factors for aortic reoperation [18, 19]. Among the overall cohort, even with aggressive aortic arch replacement, the entry tear excision rate was only 71.8% in the D1 group, which was significantly lower than that in the D2 group (96.4%). Therefore, in addition to aortic arch replacement, hybrid endovascular stent-graft implantation to seal the entry tears located at the descending thoracic aorta may also be considered to reduce the dissection-related reoperation risks in carefully selected D1-AAD patients [20].
Limitations
Several limitations to the present study should be clarified. First, as a retrospective and non-randomized control study, potential bias influencing the homogeneity of the D1 and D2 groups might have existed. However, with propensity score-matching, the intergroup heterogeneity was minimized. Furthermore, postoperative outcomes among the overall cohort and propensity-matched cohort were both well-presented and analyzed in this study. Second, because this crossed cohort spanned a period of nearly 12 years, the management regarding CPB and myocardial protection, as well as cerebral protection strategies and postoperative care protocols for treating ATAAD, may have evolved over time. Finally, despite the convincing early and late outcomes of the present study, an extended follow-up study should be conducted in the future to evaluate the long-term trends of D1-AAD and D2-AAD populations.
Conclusions
D1-AAD was associated with higher risks of in-hospital mortality and postoperative malperfusion-related complications than D2-AAD. However, for patients who survived to hospital discharge, the late survival rates were comparable between patients with D1-AAD and D2-AAD during a 5-year follow-up.
Availability of data and materials
The datasets generated and analyzed during the current study cannot be made publicly available for ethical and legal reasons. The Institutional Review Board of Chang Gung Medical Foundation must review any request to share data publicly in order to protect patients' privacy. Requests for data can be sent to the Institutional Review Board of Chang Gung Medical Foundation at irb1@cgmh.org.tw.
Abbreviations
- AAD:
-
Acute aortic dissection
- ACP:
-
Antegrade cerebral perfusion
- AsAo:
-
Ascending aorta
- ATAAD:
-
Acute type A aortic dissection
- CI:
-
Confidence interval
- CPB:
-
Cardiopulmonary bypass
- D1:
-
DeBakey type I
- D2:
-
DeBakey type II
- ECMO:
-
Extracorporeal membrane oxygenation
- ED:
-
Emergency department
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End-stage renal disease
- ICU:
-
Intensive care unit
- OR:
-
Operating room
- RCP:
-
Retrograde cerebral perfusion
- SBP:
-
Systolic blood pressure
References
Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol. 2015;66:350–8.
Bossone E, Gorla R, LaBounty TM, et al. Presenting systolic blood pressure and outcomes in patients with acute aortic dissection. J Am Coll Cardiol. 2018;71:1432–40.
DeBakey ME, McCollum CH, Crawford ES, et al. Dissection and dissecting aneurysms of the aorta: twenty-year follow-up of five hundred and twenty-seven patients treated surgically. Surgery. 1982;92:1118–34.
Daily PO, Trueblood HW, Stinson EB, et al. Management of acute aortic dissections. Ann Thorac Surg. 1970;10:237–47.
Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897–903.
Tsagakis K, Tossios P, Kamler M, et al. The DeBakey classification exactly reflects late outcome and re-intervention probability in acute aortic dissection with a slightly modified type II definition. Eur J Cardiothorac Surg. 2011;40:1078–84.
Dohle DS, El Beyrouti H, Brendel L, et al. Survival and reinterventions after isolated proximal aortic repair in acute type A aortic dissection. Interact Cardiovasc Thorac Surg. 2019;28:981–8.
Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010;121:e266-369.
Lin CY, Wu MY, Tseng CN, et al. Surgical rescues for critical hemopericardium complicated by acute type A aortic dissection: Emergent subxiphoid pericardiotomy or cardiopulmonary bypass first? PLoS ONE. 2020;15:e0229648.
Lin CY, Tseng CN, Lu CH, et al. Surgical results in acute type A aortic dissection with preoperative cardiopulmonary resuscitation: survival and neurological outcome. PLoS ONE. 2020;15:e0237989.
Lin CY, Tseng CN, Lee HA, et al. Double arterial cannulation strategy for acute type A aortic dissection repair: A 10-year single-institution experience. PLoS ONE. 2019;14:e0211900.
Lin CY, See LC, Tseng CN, et al. Surgical outcomes analysis in patients with uncomplicated acute type A aortic dissection: a 13-year institutional experience. Sci Rep. 2020;10:14883.
Kohl LP, Isselbacher EM, Majahalme N, et al. Comparison of outcomes in debakey type AI versus aii aortic dissection. Am J Cardiol. 2018;122:689–95.
Perreas K, Samanidis G, Thanopoulos A, et al. Antegrade or retrograde cerebral perfusion in ascending aorta and hemiarch surgery? A Propensity Matched Anal Ann Thorac Surg. 2016;101:146–52.
Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
Sansone F, Morgante A, Ceresa F, et al. Prognostic implications of acute renal failure after surgery for type A acute aortic dissection. Aorta (Stamford). 2015;3:91–7.
Tsai HS, Tsai FC, Chen YC, et al. Impact of acute kidney injury on one-year survival after surgery for aortic dissection. Ann Thorac Surg. 2012;94:1407–12.
Inoue Y, Minatoya K, Oda T, et al. Surgical outcomes for acute type A aortic dissection with aggressive primary entry resection. Eur J Cardiothorac Surg. 2016;50:567–73.
Kimura N, Itoh S, Yuri K, et al. Reoperation for enlargement of the distal aorta after initial surgery for acute type A aortic dissection. J Thorac Cardiovasc Surg. 2015;149:S91–8.
Inoue Y, Matsuda H, Omura A, et al. Comparative study of the frozen elephant trunk and classical elephant trunk techniques to supplement total arch replacement for acute type A aortic dissection. Eur J Cardiothorac Surg. 2019;56:579–86.
Author information
Authors and Affiliations
Contributions
C-YL conceived the study, participated in its design and coordination, and drafted the manuscript. CNT and FCT participated in the design of the study. THT and MYW helped with the drafting of the manuscript and statistical analyses. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted with the approval of the Institutional Review Board of Chang Gung Medical Foundation (approval number 202001566B0). The need for informed consent was waived due to the retrospective nature of this study.
Consent for publication
Not applicable.
Competing interests
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, CY., Tung, TH., Wu, MY. et al. Surgical outcomes of DeBakey type I and type II acute aortic dissection: a propensity score-matched analysis in 599 patients. J Cardiothorac Surg 16, 208 (2021). https://doi.org/10.1186/s13019-021-01594-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01594-9