Abstract
Background
Postoperative vasoplegia with minimal responsiveness to vasopressors is common after cardiac surgery. Called cardiac vasoplegic syndrome (CVS), it is caused by multiple factors. Treating CVS involves a high dose of fluids and catecholamines, however high doses of catecholamines and fluids are associated with serious side effects. There is evidence that new therapeutic strategies can lead to a reduction in norepinephrine doses and mortality in CVS. Specifically, the use of non-adrenergic vasopressors such as methylene blue (MB) can be beneficial.
Methods
We retrospectively analyzed the electronic records of 8716 adult cardiac surgery patients from November 2008 to December 2016. Medication, hemodynamic and outcome parameter data were analyzed for CVS until discharge. We determined CVS according to the following parameters: a postoperative onset of ≤24 h, a reduced mean arterial pressure (MAP) of < 70 mmHg, a dose of norepinephrine ≥0.8 mg*h− 1 and a continuously increasing need for catecholamine, without ventricular dysfunction.
Results
We identified 513 patients with CVS. Perioperative risk factors were higher in patients treated with methylene blue (MB). Before MB administration patients had a significantly higher dose of norepinephrine, and MAP increased after MB administration. Norepinephrine could be reduced after MB administration and MAP remained stable at the same level even after the reduction of norepinephrine.
Conclusions
CVS patients have a severe systemic disease accompanied by significant operative stress and a high catecholamine requirement. The administration of MB in addition to standard treatment for CVS in the first 24 h was accompanied by an increase in MAP followed by a decrease in vasopressor requirement, indicating that early MB administration can be beneficial.
Similar content being viewed by others
Background
Postoperative hypotension is common in patients after cardiac surgery. The three major hemodynamic disorders after cardiac surgery are hypovolemia, vasoplegia and heart failure. These three disorders are responsible for episodes of hypotension that are associated with poor outcome. In particular, vasoplegia with minimal responsiveness to vasopressors such as norepinephrine, known as cardiac vasoplegic syndrome (CVS), is associated with increased mortality [1,2,3]. Observational studies report a CVS incidence of 5–50% in cardiac surgery with cardiopulmonary bypass (CPB) [1, 2, 4]. The routine treatment for CVS consists of administering fluids and catecholamines (e.g. norepinephrine) [2]. Catecholamines are associated with serious side effects such as increased myocardial oxygen consumption, the development of arrhythmias, or decreased renal and visceral blood flow [5]. Furthermore, the excessive administration of fluids is associated with side effects [6]. To prevent these side effects, an additional treatment to reduce catecholamine requirement is needed [7]. Observational studies report methylene blue (MB) as a therapeutic alternative or adjuvant to the classic vasoplegic syndrome therapies [1]. MB is a non-catecholaminergic agent already proven to cause a statistically significant increase in mean arterial pressure (MAP). This effect has led to no serious adverse events based on a meta-analysis of five randomized controlled trials [8]. Additionally, MB reduces catecholamine stress in critically ill patients. This effect is called decatecholaminisation and may improve survival in CVS [9, 10]. Currently, MB does not have any approved indications for CVS therapy. The purpose of this study is to determine the incidence of CPB-induced vasoplegic syndrome and to describe the practice of MB use at our cardiac surgery department. We hypothesized that MB administration in ICUs would reduce the risk of mortality in CVS patients.
Methods
This study was approved by the University of Regensburg’s ethics committee (AZ 15101–0046). Hemodynamic records of the intensive care unit (ICU) data management system (PDMS, Metavision®, Tel Aviv, Israel) were used for this study. All adult cardiac surgery patients from November 2008 to December 2016 were screened for CVS. Cardiac vasoplegic syndrome was defined by criteria shown in Table 1. Vasopressor medication (e.g., catecholamines, hydrocortisone and vasopressin) and outcome parameters were analyzed until discharge.
Patients with multiple MB administration, MB administration > 24 h (h) after ICU admission, pregnant patients, patients with sepsis or patients with insufficient or missing data were excluded. Perioperative data were obtained from sources including anesthesia records (Medlinq®, Hamburg, Germany), ICU (PDMS) data, as well as medical reports and quality management (QM) data from the hospital information system (SAP®, Walldorf, Germany). The period of observation ended upon patient discharge from the hospital. Collected data were standardized and anonymized.
MB administration was set as time 0 in the MB group. Haemodynamic parameters and medications were documented at − 3, − 2, − 1 h before MB administration and at 1, 2, 3, 4, 8, 12, 24, 48 and 72 h afterwards. For the non-MB group, time point 0 was defined as 6 h after ICU admission, corresponding to the mean time of MB administration after MB-group patient admission to the ICU.
Data were analysed with SPSS (IBM Corp., Armonk. USA, version 23) using Pearson’s chi-squared test or t-tests. A p-value of < 0.05 was considered statistically significant. All data in the text, tables and figures are given as percentages (%), mean and standard deviation (SD) or standard error of the mean (SEM).
Results
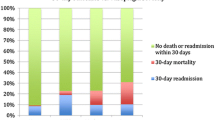
From November 2008 to December 2016, our department performed 8716 cardiopulmonary bypasses (CPB). According to the definition in Table 1, a total of 710 of these CPB patients, equating 8.15% of our study population, had vasoplegic syndrome (Fig. 1). We excluded 113 patients from further analysis due to insufficient or missing data. Of the remaining 597 patients with vasoplegic syndrome, we identified 84 as septic vasoplegic syndrome patients and therefore excluded them from further analysis. Five hundred thirteen remaining patients with complete data sets fulfilled our criteria for cardiac vasoplegic syndrome. This corresponded to 5.86% of all patients after cardiac surgery. Of these 513 patients, 311 (60.23%) received MB in the first 24 h after ICU admission (MB group). The remaining 202 patients had no MB administration (non-MB group, Table 2). Demographic and intraoperative data of the MB group and the non-MB group are shown in Tables 3 and 4. Compared to the non-MB group, patients in the MB group had markedly more comorbidities and perioperative complications, e.g., kidney failure, acute myocardial infarction, emergency operation, previous cardiac surgery events, and prolonged CBP-time, among others. The MB group patients had a norepinephrine mean continuous infusion rate of 1.2 ± 0.61 mg*h− 1 (mean ± SD) before MB administration. In the non-MB group the continuous infusion rate of norepinephrine was 0.64 ± 0.51 mg*h− 1 (mean ± SD). The continuous infusion rate of norepinephrine was significantly higher in the MB group compared to the non-MB group at time 0 (p < 0.05; Fig. 2). Mean arterial pressure (MAP) was significantly lower in the MB group before MB administration compared to the non-MB group (p < 0.05; Fig. 3). Additional vasopressors such as epinephrine, vasopressin and hydrocortisone were administered significantly more in the MB group (p < 0.001), as shown in Table 5. Extended hemodynamic monitoring was used significantly more in the MB group compared to non-MB group. Trans-oesophageal echocardiography was performed significantly more in the MB group (160 patients, 53%) compared to the non-MB group (51 patients, 25%; p < 0.001). A pulmonary artery catheter (PAC) was employed 182 times (61%) in the MB group and 38 times (19%) in the non-MB group (p < 0.001). Pulse contour cardiac output (PICCO) was only performed in the MB group (2%). Mean central venous saturation (ScvO2) in the MB group (66 ± 24%) was not significantly different compared to the non-MB group (65 ± 70%). Cardiac index (CI) was not significantly different between the MB (3.3 ± 1.0 L/min/m2) and non-MB (3.4 ± 1.0 L/min/m2) (mean ± SD) groups. MB was administered 6.4 ± 5.2 (mean ± SD) h after ICU admission, with a dose of 174 ± 56 mg (mean ± SD). This dose equates to approximately 2.0 mg*kg− 1 body weight. In 89% of all cases MB was administered continuously by infusion pump over 51 ± 28 min (mean ± SD) and in the remaining 11% of cases MB was given as a bolus. MAP increased significantly from 65 + 0.5 mmHg (mean ± SEM) at time point − 1 to 71 + 0.5 mmHg (mean ± SEM) at time point 2 (p < 0.05) after MB administration. Compared to time points − 3, − 2, − 1 and 0, MAP increased significantly in the MB group at time point 1 (p < 0.05) (Fig. 3). No difference in the MAP levels of the MB and non-MB groups was observed beyond time point 1 to the end of the observation period. The continuous norepinephrine infusion rate decreased from time point 1 while maintaining constant hemodynamic and MAP values. At all times, the continuous norepinephrine infusion rate of the non-MB group was significantly lower than that of the MB group. The 30-day mortality was significantly higher in the MB group compared to the non-MB group (p < 0.001). The rates of organ failure (p < 0.001) and number of ventilation days were also significantly higher (p < 0.001) in the MB group (Table 6).
Discussion
To the best of our knowledge, this retrospective study contains the highest number of CVS patients treated with MB of studies to date. Vasoplegic syndrome after cardiac surgery is an independent mortality factor in cardiac surgery patients [3], and CVS is caused by multiple factors [2, 11]. There are currently no standardized definition criteria for CVS [12]. For this reason, CVS incidence ranges from 5 to 50% in the literature [2, 4]. Van Vessem et al., for example, observed a vasoplegic syndrome incidence of 29% in their study [4]. Using the vasoplegia criteria shown in Table 1 and including septic patients, we identified a vasoplegic syndrome incidence rate of 8.15% (710 of 8716). Excluding sepsis as the cause of vasoplegic syndrome and excluding incomplete data sets, CVS incidence in our study population was 5.88% (513 of 8716). This incidence rate is comparable to findings from other studies investigating CVS [11, 13]. Typical risk factors (RF) for vasoplegic syndrome after CBP in these studies included CBP time, emergency operation, and previous myocardial infarction. We also identified these RF in our study (Tables 3 and 4) [2, 4, 11]. In addition to identifying possible RF, it is important to define CVS in order to facilitate early recognition and treatment. In our opinion, a combination of the most frequently used vasoplegia criteria from CVS studies offers a starting point to define CVS. These CVS criteria are: the need for increasing doses of vasopressors (> 0.15 μg*kg− 1*min− 1 norepinephrine), mean arterial pressure < 70 mmHg, a systemic vascular resistance index (SVRI) < 600 dyn*s*cm− 5*m− 2, and the exclusion of ventricular failure (CI > 2.5 L*min− 1) [14,15,16,17]. Patients who met all these criteria within 24 h post-CPB, whose vasoplegia was not caused by sepsis and who did not have hypovolemia, had non-septic CVS according to our extended definitions (Table 1).
The first positive hemodynamic effect of MB in cardiac surgery was reported 1996. In that study Andrade et al. reported using 1.5 mg*kg− 1 of MB in six patients with vasoplegic syndrome. After MB administration, SVRI increased from 868 to 1693 dyn*s*cm− 5*m− 2 [18]. It is supposed that MB’s vasoconstrictive effect is caused by two mechanisms: MB inhibits inducible NO synthase, thus reducing the vasodilating ligand, and MB binds competitively to the heme group of guanylate cyclase, thus additionally reducing the receptor binding site for vasodilation [1, 12, 19]. The result is catecholamine-independent vasoconstriction. The administration of MB can therefore reduce catecholamine requirement and catecholaminergic stress in critically ill patients. This therapeutic approach is known as decatecholaminisation [8]. But insufficient hemodynamic effects after MB administration have also been reported. MB’s variable vasoconstrictive effect may be explained by the non-standardized administration of MB; in these studies the time point of MB administration, dosage etc. differed considerably, thereby explaining the various reactions to MB [2, 5, 20, 21]. There are some side effects and complications associated with MB administration. These undesirable MB effects can be categorized into minor and severe complications. Classic minor side effects such as dizziness and nausea were not detectable in any of our patients, though these minor side effects may not have been apparent in our study as all patients were intubated and sedated during MB treatment. The administration of MB can also result in microcirculation disorders and local cutaneous necrosis [22]. Whether there is a beneficial or harmful MB effect on mesenteric perfusion in vasoplegic shock is still unclear [23]. The use of MB in glucose-6-phosphate dehydrogenase-deficient patients triggers severe hemolytic crisis in these patients and therefore must be avoided [24].The mean MB dose in our study was 2.0 mg*kg− 1, which corresponds to that of others studies and is described as a safe standard dose [25].In our study, a small group of twelve patients received an unintentionally higher dose of MB (4.5 mg*kg− 1 - 5.5 mg*kg− 1). Neither the standard dose group (< 2.0 mg*kg− 1) nor the maximum dose group (4.5 mg*kg− 1 - 5.5 mg*kg− 1) experienced any minor or serious side effects in our study.
A significant increase of 5 mmHg MAP after MB administration was detected in our study (Fig. 3), and MB administration was followed decreased vasopressor requirement (Fig. 2). These findings are comparable to those of other studies which describe the catecholamine-reducing effect of additional MB therapy in cardiac vasoplegic syndrome. Surprisingly, a reduction in mortality after MB administration in CVS was not identified in this study [13]; the mortality rate of the MB group was significantly higher compared to the non-MB group (18% vs. 5%, p < 0.001). These different findings are explained by our study design: the purpose of this study was to determine CVS incidence and to describe MB use in our cardiothoracic surgery department, therefore we conducted the study as a retrospective analysis. Because MB administration for severe CVS is an established treatment at our department, the two CVS groups we formed retrospectively (MB and non-MB) were not entirely comparable. When considering the noradrenaline dosage course and MAP course (Figs. 2 and 3) in the MB and non-MB groups, a lower vasopressor requirement and higher MAP in the non-MB group was detected. Typical risk factors for vasoplegic syndrome, such as comorbidities, long CBP time and emergency operation, were also significantly more frequent in the MB group (Tables 3 and 4). This indicates that patients in the MB group were at a greater risk of severe CVS compared to the non-MB group. Furthermore, we postulate that the non-MB group in our study had less vasoplegia. The incidence rates of 5–50% in the literature and the lack of a standard definition of vasoplegic syndrome confirm the thesis that there are several degrees of vasoplegia [1, 17, 26]. The MB group patients’ higher mortality rate can therefore be explained by their greater degree of illness compared to the non-MB group patients.
It is not only the severity but also the duration of vasoplegia which influences outcome. Gomes et al. demonstrated that a high mortality rate of 25% is associated with vasoplegic syndrome lasting > 36–48 h [20]. In our study with a mortality rate of 18%, MB was given early after ICU admission. After MB administration the need for norepinephrine decreased over the first hours to a level below 0.8 mg*h− 1 (Fig. 2). Within the first hour after MB administration, MAP increased in treated patients while vasopressor requirement decreased (Fig. 3).
Some studies have demonstrated that the use of MB in severe vasoplegic syndrome reduces the mortality rate from 44 to 21.2% [17, 27].The reduction of mortality in these studies is comparable to our study’s mortality rate of 18% in the MB group. Mehaffey et al. demonstrated that not only the administration itself but also the timing of MB administration is important in order to decrease mortality. Mehaffey’s study demonstrated that MB administration during operation reduced the incidence of postoperative renal failure and operative mortality when compared to ICU MB administration (10.4% vs. 28.6%) [13]. Other studies have also demonstrated that preoperative MB administration in patients with a high risk of vasoplegic syndrome during cardiac surgery can prevent CVS. In this study no vasoplegic syndrome in the MB-treated group was detected compared to 26% CVS in the non-MB group [25]. It is assumed that a therapeutic regime with MB as an “on-top” medication in high-risk patients is reasonable and can reduce mortality. In order to reduce CVS mortality, CVS therapy must follow the principles of therapy for sepsis: hit hard, hit early. Therefore, early administration of MB is beneficial [13, 17].
This study has some limitations. First of all, as there is no standard definition of vasoplegic syndrome, each study has different parameters for the study population. For example, Ozal et al. defined CVS mainly through surrogate parameters as MAP < 50 mmHg, cardiac index > 2.5 L*min− 1*m− 2, right atrial pressure < 5 mmHg, left atrial pressure < 10 mmHg and reduced SVR < 800 dyn*s− 1*cm− 5 throughout intravenous infusion of norepinephrine (≥ 0.5 μg*kg− 1*min− 1) [25]. In contrast, Weiner et al. defined CVS by a high dependency on the norepinephrine > 0.2 μg*kg− 1 min− 1 and vasopressin > 2 I.E.*h− 1 catecholamines [28]. Therefore, a comparison of the results of each study has to be done carefully. We use a combination of Ozal et al.’s and Weiner et al.’s parameters in our study: at the time of MB administration, vasoplegic patients showed a MAP > 60 mmHg, a norepinephrine dose of 1.2 +/− 0.6 mg*h− 1 and SVR > 800 dyn*s− 1*cm− 5. While our norepinephrine doses correlate with those defined in the other studies, MAPs and SVRs in our study were higher than in other studies [29]. This may be due to a timely therapeutic response to drops in blood pressure. A marked ramping up of norepinephrine in the first hours after admission (exaltation of 0.1 mg*h− 1 in at least 3 consecutive steps) is apparent in our study, which – in our view – characterizes the very unique clinical catecholamine refractory vasoplegic situation leading to MB administration. In our clinical practice, we use mg*h− 1 as the dosage designation. An additional dosage recalculation into the commonly used μg*kg− 1*min− 1 had no effect on the statistical statements.
Another limitation due to this study’s retrospective design is the lack of a perfect control group with the same severity of illness as the MB group. The retrospective analysis demonstrated that the non-MB group is not a true control. Tables 1 and 2 show that the MB group patients had a higher ASA classification, more emergency operations, increased norepinephrine doses before and after operation, and longer CPB and ischemia times. It is therefore not surprising that morbidity, mortality and organ failure in the MB group was higher than in the non-MB group.
Conclusions
Cardiac vasoplegia patients suffer from a severe systemic disease accompanied by operative stress and a high requirement of catecholamines. Additional MB administration to the standard treatment of CVS and over the first hours after admission to the ICU was accompanied by an increase in blood pressure followed by a decrease in vasopressor requirement. Early MB administration (during operation) in cardiac vasoplegic syndrome may be even more effective. A norepinephrine dose of 0.8 mg/h (0.15 μg*kg-1*min-1) followed by the need to ramp up the dose (≥ 0.1 mg*h-1) may serve as criteria for early MB administration. More prospective and randomized studies are necessary to further investigate the potential of MB administration on CVS after cardiac surgery.
Availability of data and materials
The datasets used and analyzed for this study are available from the corresponding author upon reasonable request.
Abbreviations
- CI:
-
Cardiac index
- CPB:
-
Cardiopulmonary bypass
- CVS:
-
Cardiac vasoplegic syndrome
- e.g.:
-
Exempli gratia / for example
- ICU:
-
Intensive care unit
- h:
-
Hour
- L/min/m2:
-
Liter per minute per square meter
- MAP:
-
Mean arterial pressure
- MB:
-
Methylene blue
- mmHg:
-
Millimeter quicksilver
- mg*h-1:
-
Milligram per hour
- mg*kg-1:
-
Milligram per kilogram
- PICCO:
-
Pulse contour cardiac output
- PAC:
-
Pulmonary arterial catheter / Swan-Ganz-catheter
- QM:
-
Quality management
- RF:
-
Risk factor
- ScvO2:
-
Central venous saturation
- SD:
-
Standard deviation
- SEM:
-
Standard error of the mean
- SVR:
-
Systemic vascular resistance
- SVRI:
-
Systemic vascular resistance index
References
Hosseinian L, Weiner M, Levin MA, Fischer GW. Methylene blue: magic bullet for Vasoplegia? Anesth Analg. 2016;122(1):194–201. https://doi.org/10.1213/ANE.0000000000001045.
Omar S, Zedan A, Nugent K. Cardiac vasoplegia syndrome: pathophysiology, risk factors and treatment. Am J Med Sci. 2015;349(1):80–8. https://doi.org/10.1097/MAJ.0000000000000341.
Fischer GW, Levin MA. Vasoplegia during cardiac surgery: current concepts and management. Semin Thorac Cardiovasc Surg. 2010;22(2):140–4. https://doi.org/10.1053/j.semtcvs.2010.09.007.
van Vessem ME, Palmen M, Couperus LE, Mertens B, Berendsen RR, Tops LF, et al. Incidence and predictors of vasoplegia after heart failure surgery. Eur J Cardiothorac Surg. 2017;51(3):532–8. https://doi.org/10.1093/ejcts/ezw316.
Gamper G, Havel C, Arrich J, Losert H, Pace NL, Müllner M, et al. Vasopressors for hypotensive shock. Cochrane Database Syst Rev. 2016;2:CD003709.
Hariyanto H, Yahya CQ, Widiastuti M, Wibowo P, Tampubolon OE. Fluids and sepsis: changing the paradigm of fluid therapy: a case report. J Med Case Rep. 2017;11(1):30. https://doi.org/10.1186/s13256-016-1191-1.
Hajjar LA, Vincent JL, Barbosa Gomes Galas FR, Rhodes A, Landoni G, Osawa EA, et al. vasopressin versus norepinephrine in patients with Vasoplegic shock after cardiac surgery: the VANCS randomized controlled trial. Anesthesiology. 2017;126(1):85–93. https://doi.org/10.1097/ALN.0000000000001434.
Pasin L, Umbrello M, Greco T, Zambon M, Pappalardo F, Crivellari M, et al. Methylene blue as a vasopressor: a meta-analysis of randomised trials. Crit Care Resusc. 2013;15(1):42–8.
Rudiger A, Singer M. Decatecholaminisation during sepsis. Crit Care. 2016;20(1):309. https://doi.org/10.1186/s13054-016-1488-x.
Belletti A, Benedetto U, Biondi-Zoccai G, Leggieri C, Silvani P, Angelini GD, et al. The effect of vasoactive drugs on mortality in patients with severe sepsis and septic shock. A network meta-analysis of randomized trials. J Crit Care. 2017;37:91–8. https://doi.org/10.1016/j.jcrc.2016.08.010.
Byrne JG, Leacche M, Paul S, Mihaljevic T, Rawn JD, Shernan SK, et al. Risk factors and outcomes for ‘vasoplegia syndrome’ following cardiac transplantation. Eur J Cardiothorac Surg. 2004;25(3):327–32. https://doi.org/10.1016/j.ejcts.2003.11.032.
Evora PRB, Alves Junior L, Ferreira CA, Menardi AC, Bassetto S, Rodrigues AJ, et al. Twenty years of vasoplegic syndrome treatment in heart surgery. Methylene blue revised. Rev Bras Cir Cardiovasc. 2015;30(1):84–92. https://doi.org/10.5935/1678-9741.20140115.
Mehaffey JH, Johnston LE, Hawkins RB, Charles EJ, Yarboro L, Kern JA, et al. Methylene blue for Vasoplegic syndrome after cardiac operation: early administration improves survival. Ann Thorac Surg. 2017;104(1):36–41. https://doi.org/10.1016/j.athoracsur.2017.02.057.
Argenziano M, Chen JM, Choudhri AF, Cullinane S, Garfein E, Weinberg AD, et al. Management of vasodilatory shock after cardiac surgery: identification of predisposing factors and use of a novel pressor agent. J Thorac Cardiovasc Surg. 1998;116(6):973–80. https://doi.org/10.1016/S0022-5223(98)70049-2.
Cremer J, Martin M, Redl H, Bahrami S, Abraham C, Graeter T, et al. Systemic inflammatory response syndrome after cardiac operations. Ann Thorac Surg. 1996;61(6):1714–20. https://doi.org/10.1016/0003-4975(96)00055-0.
Tsiouris A, Wilson L, Haddadin AS, Yun JJ, Mangi AA. Risk assessment and outcomes of vasoplegia after cardiac surgery. Gen Thorac Cardiovasc Surg. 2017;65(10):557–65. https://doi.org/10.1007/s11748-017-0789-6.
Levin MA, Lin H-M, Castillo JG, Adams DH, Reich DL, Fischer GW. Early on-cardiopulmonary bypass hypotension and other factors associated with vasoplegic syndrome. Circulation. 2009;120(17):1664–71. https://doi.org/10.1161/CIRCULATIONAHA.108.814533.
JCSd A, Batista Filho ML, PRB É, Tavares JR, Buffolo Ê, Ribeiro EE, et al. Utilização do azul de metileno no tratamento da síndrome vasoplégica após cirurgia cardíaca. Rev Bras Cir Cardiovasc. 1996;11:2.
Mayer B, Brunner F, Schmidt K. Novel actions of methylene blue. Eur Heart J. 1993;14(Suppl I):22–6.
Gomes WJ, Carvalho AC, Palma JH, Teles CA, Branco JN, Silas MG, et al. Vasoplegic syndrome after open heart surgery. J Cardiovasc Surg. 1998;39(5):619–23.
Manghelli J, Brown L, Tadros HB, Munfakh NA. A reminder of methylene Blue's effectiveness in treating Vasoplegic syndrome after on-pump cardiac surgery. Tex Heart Inst J. 2015;42(5):491–4. https://doi.org/10.14503/THIJ-14-4470.
Dumbarton TC, Gorman SK, Minor S, Loubani O, White F, Green R. Local cutaneous necrosis secondary to a prolonged peripheral infusion of methylene blue in vasodilatory shock. Ann Pharmacother. 2012;46(3):e6. https://doi.org/10.1345/aph.1Q560.
Al-Diery H, Phillips A, Evennett N, Pandanaboyana S, Gilham M, Windsor JA. The pathogenesis of nonocclusive mesenteric ischemia: implications for research and clinical practice. J Intensive Care Med. 2019;34(10):771–81. https://doi.org/10.1177/0885066618788827.
Youngster I, Arcavi L, Schechmaster R, Akayzen Y, Popliski H, Shimonov J, et al. Medications and glucose-6-phosphate dehydrogenase deficiency: an evidence-based review. Drug Saf. 2010;33(9):713–26. https://doi.org/10.2165/11536520-000000000-00000.
Ozal E, Kuralay E, Yildirim V, Kilic S, Bolcal C, Kücükarslan N, et al. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery. Ann Thorac Surg. 2005;79(5):1615–9. https://doi.org/10.1016/j.athoracsur.2004.10.038.
Levin RL, Degrange MA, Bruno GF, Del Mazo CD, Taborda DJ, Griotti JJ, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77(2):496–9. https://doi.org/10.1016/S0003-4975(03)01510-8.
Dagenais F, Mathieu P. Rescue therapy with methylene blue in systemic inflammatory response syndrome after cardiac surgery. Can J Cardiol. 2003;19(2):167–9.
Weiner MM, Lin H-M, Danforth D, Rao S, Hosseinian L, Fischer GW. Methylene blue is associated with poor outcomes in vasoplegic shock. J Cardiothorac Vasc Anesth. 2013;27(6):1233–8. https://doi.org/10.1053/j.jvca.2013.02.026.
Leyh RG, Kofidis T, Strüber M, Fischer S, Knobloch K, Wachsmann B, et al. Methylene blue: the drug of choice for catecholamine-refractory vasoplegia after cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2003;125(6):1426–31. https://doi.org/10.1016/S0022-5223(02)73284-4.
Acknowledgements
This research was supported in part by Provepharm SAS. We would like to thank Gabriele Bollwein and Marion Schindler for their assistance in performing the computations, and Dirk Lunz and Andre Bredthauer for greatly improving this manuscript with their valuable comments.
Submission declaration
The authors declare that they agree with and are responsible for the data presented in this study. This manuscript has not been published and is not under consideration for publication elsewhere.
Funding
This study was performed using departmental research funding. In addition, an unrelated grant was given to the Department of Anesthesiology, University Hospital Regensburg, by Provepharm SAS, 22 rue Marc Donadille, F-13013 Marseille, France. This grant is not associated with any influence on study design, performance or manuscript approval by the company. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Walter Petermichl, York A. Zausig and Bernhard M. Graf conceived of the idea presented here. Walter Petermichl, Michael Gruber, Ina Schoeller and Kwahle Allouch developed the theory and performed the computations. Walter Petermichl wrote the manuscript with support from York A. Zausig and Michael Gruber. York A. Zausig supervised the project. All authors discussed the results and contributed to the final manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the University of Regensburg before the start of data collection and was carried out under the ethics committee reference number AZ 15 101–0046.
Consent for publication
Not applicable.
Competing interests
WP, IS and KA declare no competing interests. This study was performed using departmental research funding. In addition, an unrelated grant was given to the Department of Anesthesiology (MG, BG, YZ), University Hospital Regensburg, by Provepharm SAS, 22 rue Marc Donadille, F-13013 Marseille, France. This grant is not associated with any influence on study design, performance or manuscript approval by the company.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Petermichl, W., Gruber, M., Schoeller, I. et al. The additional use of methylene blue has a decatecholaminisation effect on cardiac vasoplegic syndrome after cardiac surgery. J Cardiothorac Surg 16, 205 (2021). https://doi.org/10.1186/s13019-021-01579-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01579-8