Abstract
Background
The overall survival (OS) remains unsatisfactory in patients with esophageal squamous cell carcinoma (ESCC) after extended esophagectomy with two-field lymphadenectomy. Therefore, this retrospective study aimed to identify the risk factors that contribute to the low survival of patients with pT1–3N0M0 ESCC.
Methods
Patients with pT1–3N0M0 ESCC who only underwent R0 esophagectomy with two-field lymphadenectomy in our department from January 2008 to December 2012 were retrospectively enrolled in this study and medical records were reviewed. Postoperative OS, disease-free survival (DFS), recurrence-free survival (RFS), and locoregional recurrence-free survival (LRFS) were analyzed sequentially.
Results
This study recruited a total of 488 patients, whose follow-up visits were completed at the end of December 2019. The five-year OS, DFS, RFS and LRFS rates were 62.1, 53.1, 58.3 and 65.6%, respectively. Multivariate Cox analysis identified patient age, site of the lesion, small mediastinal lymph nodes in CT imaging (SLNs in CT), dissected lymph nodes (LNs), and stage of esophageal malignancy as independent risk factors for OS of the patients. Of these factors, the site of the lesion, SLNs in CT and stage of the cancer were determined to be independent factors for DFS, RFS and LRFS. Based on all five factors, the recursive partitioning analysis (RPA) score system was developed to stratify the patients into low-, medium- and high-risk groups, which were found to possess significantly different rates of OS, DFS, RFS and LRFS (p < 0.001).
Conclusions
Several factors were associated with the survival of patients with pT1–3 N0M0 ESCC who underwent extended esophagectomy with two-field lymphadenectomy. These factors contributed to the RPA scoring system, which could stratify the risk of postoperative survival and may expedite the initiation of postoperative adjuvant therapy.
Similar content being viewed by others
Background
Esophageal cancer (EC) ranked seventh in terms of incidence and sixth in overall mortality in 2018 [1]. Esophageal squamous cell carcinoma (ESCC) is the predominant pathological type of EC worldwide [2]. The Ivor-Lewis subtotal esophagectomy with either two-field or three-field lymphadenectomy remains the current procedure of choice for resectable ESCC, but the postoperative prognosis remains unsatisfactory at only 50% for five-year overall survival (OS) in patients with pathologic negative lymph node (pN0) ESCC [3,4,5]. Postoperative recurrence, especially locoregional recurrence (LRR), has been shown to be relatively high in pN0 ESCC patients [6,7,8].
Moreover, the effectiveness of postoperative adjuvant chemo- and radiation therapy has not been established for the management of pN0 ESCC patients [8,9,10]. Previous studies have shown that several factors, such as age, tumor location, the number of dissected lymph nodes (LNs), pathological stage, and others were associated with the survival of ESCC patients after surgery [3,4,5,6,7,8,9,10,11,12,13,14]. A recursive partitioning analysis (RPA)-based system has been used to evaluate and predict the prognosis of EC patients after resection [15,16,17].
This retrospective study aimed to identify the factors associated with a survival benefit, and to further stratify the survival risk based on the RPA scores for patients with stage pN0 ESCC following two-field esophagectomy. These findings will help to determine the need for postoperative adjuvant therapy in these patients to improve OS.
Methods
Patients
All patients in this study completed a full course of follow-up visits in 2016 and were recruited for this second round of additional study. The inclusion criteria were described as follows: (1) patients underwent radical (R0) esophagectomy with two-field lymphadenectomy in our hospital between January 2008 and December 2012; (2) patients had a pathological diagnosis of ESCC; (3) patients were staged as pT1–3N0M0; (4) patients were not managed with either neoadjuvant or adjuvant therapy; (5) patients were not found to have a history of other malignancies; (6) the postoperative survival time was at least 3 months to minimize the impact of surgical complications on survival; and (7) patients had participated and were followed-up in our previous study [6]. The exclusion criteria were: (1) patients had non-ESCC at their pathological diagnosis; (2) patients underwent either R1 or R2 resection or three-field lymphadenectomy; (3) patients were pathologically staged as either pT4, pN+ or M1; (4) patients were managed with either pre- and/or post-operative adjuvant therapy; and (5) post-operative survival time was less than 3 months.
The study design and related ethical issues were approved by the Medical Ethics Committee of our hospital, and written informed consent was obtained from all patients enrolled in this study. Furthermore, the medical records of all patients were reviewed and information pertinent to the study was extracted from the records, including patient demographics, perioperative work-ups, detailed intraoperative information, and information related to postoperative management as well as long-term follow-ups.
Surgery
The left thoracic approach (Sweet procedure) was routinely chosen to gain access to the primary tumors located in the middle/lower thoracic segment of the esophagus. The right thoracic approach (Ivor Lewis procedure) was used to access the primary tumors located in the upper thoracic segment of the esophagus. Radical surgical resection consisted of transthoracic subtotal esophagectomy with abdominal and mediastinal lymphadenectomy. A gastric tube placed through the posterior mediastinal route was used as a substitute for the resected esophagus to restore the continuity of the alimentary tract. Two-field LN dissection included total mediastinal, perigastric, and celiac lymphadenectomy.
Follow-up
The first postoperative follow-up visits were scheduled for 1 month after the surgery. Thereafter, patients were sequentially followed every 3 months for the first 2 years, every 6 months for the next 3 years, and then every 12 months. The deadline for all follow-ups was December 1st, 2019. During the follow-up visits, patients were re-examined with chest computed tomography (CT) scans, and abdominal and cervical ultrasounds or CTs. When necessary, endoscopy, radionuclide bone imaging, or positron emission tomography (PET)/CT scans were also offered to the patients.
Statistical analysis
In this study, overall survival (OS) was defined as the period from the date of surgery to the date of death or last follow-up. Disease-free survival (DFS) was defined as the time from the date of surgery to the date of the first evidence of recurrence or death of any cause. Recurrence-free survival (RFS) was defined as the period from the date of surgery to the date of the first evidence of tumor recurrence. Locoregional recurrence-free survival (LRFS) was defined as the period from the date of surgery to the date of the first evidence of locoregional recurrence (LRR) of the malignancy. LRR was defined as neoplastic recurrence at the original cancer site or stoma area, or appearance of metastatic lymph nodes in the supraclavicular, mediastinum, or epigastrium regions. Relapses at other sites were defined as distant metastases (DM).
The survival rate was calculated using the Kaplan-Meier method, and comparisons between groups were performed with the log-rank test. A two-tailed p value < 0.05 was considered statistically significant. Multivariate Cox regression analyses were performed to identify prognostic factors for survival. All statistical analyses were conducted using SPSS 22.0 software (IBM Corp, Armonk, NY, USA).
Results
Patient demographics
A total of 488 patients with pT1–3N0M0 thoracic ESCC were enrolled in this study. The median age was 62 years (range: 34–86 years) and the ratio of males to females was 1.64:1. Preoperative imaging determined that the median tumor size was 4 cm (range: 1–10 cm) and mediastinal small LNs (transverse section diameter < 1 cm) were visualized in 115 patients (defined as “SLNs in CT” below). Intraoperatively, two-field lymphadenectomy was used to dissect out local LNs (defined as “dissected LNs” below) and the median number removed was 10 (range: 1–27; Table 1).
Outcomes
Among 488 patients, 226 had a recurrence of their cancer for an overall recurrence rate of 46.3%. The recurrence developed locally in 182 patients, and the LRR rate was 37.3%. Moreover, 213 (43.6%) patients died during the follow-up period, of which 173 (35.5%) were the result of tumor progression and 40 (8.2%) were due to non-cancer-related causes. Finally, 36 patients were lost to follow-up before the deadline of December 1st, 2019, which gave a follow-up rate of 92.6%.
Survival analysis
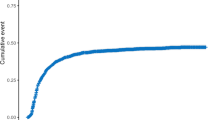
At the follow-ups for 1, 2, 3, 4, 5 and 8 years, the rates of OS obtained were 93.2, 82.2, 73.0, 66.8, 62.1 and 56.5%, and the rates of DFS were 83.4, 73.8, 63.7, 59.0, 53.1 and 46.3%, respectively (Fig. 1). Moreover, at the follow-ups for 1, 3, 5 and 8 years, the rates of RFS were 85.7, 68.0, 58.3 and 51.8%, and the rates of LRFS were 87.5, 73.3, 65.6 and 59.9%, respectively (Table 2).
Univariate analysis showed that site of the lesion, SLNs in CT, and pT stage were associated with OS, DFS, RFS and LRFS (p < 0.05); however, associations with patient age and dissected LNs were only established for OS, not for other survival parameters. Gender, size of the tumor, and histopathological differentiation of ESCC were not associated with OS, DFS, RFS or LRFS (p > 0.05; Table 2). Multivariate Cox analysis revealed that, patient age, the site of the lesion, SLNs in CT, dissected LNs and pT stage were independent factors for OS (Tables 3); the site of the lesion, SLNs in CT, and pT stage were independent factors for DFS, RFS and LRFS (Tables 4).
Recursive partitioning analysis scores
A recursive partitioning analysis (RPA) model was used to predict the survival of ESCC patients in previous studies [15,16,17]. Based on the five independent prognostic factors for OS in our study, risk levels were further stratified as 0, 1 and 2 in accordance with the Cox analysis. The total RPA score was calculated for each patient using the following factors: gender (female = 0, male = 1), site of the lesion (lower or middle segment = 0, upper segment = 1), SLNs in CT (no = 0, yes = 1), dissected LNs (≤ 12 = 0, > 12 = 1) and pT stage (pT1 = 0, pT2 = 1, pT3 = 2).
Once with RPA scores were determined, the patients were first assigned into six groups with scores of 0 (18 patients), 1 (58 patients), 2 (135 patients), 3 (154 patients), 4 (97 patients) and 5 (26 patients). Patients were then further classified according to risk level: low-risk group (RPA score: 0–1, 76 cases), medium-risk group (RPA score: 2, 135 cases), and high-risk group (RPA score: 3–5, 277 cases). The rates of OS, DFS, RFS and LRFS were significantly different among all three groups (p < 0.001; Fig. 2 and Table 5).
Discussion
The optimal surgical technique for the curative treatment of patients with pN0 esophageal cancer has remained controversial. Currently, the procedures of choice include R0 esophagectomy with two-field lymphadenectomy based on evidence of early submucosal infiltration and early-stage lymphatic dissemination of the cancer, both of which pose challenges for the long-term outcomes of the surgery.
Two studies have already shown that the five-year OS rates were 51.2% for pT1–3N0M0 [3] and 52.9% for stage pN0 [4] ESCC patients who underwent two-field surgery without neoadjuvant or adjuvant chemoradiation therapies. Moreover, another study based on 2588 patients with pT1–3N0M0 EC [18] further reported that the postoperative five- and 10-year OS rates were 67.1 and 57.6%, respectively, and the cause-specific survival (CSS) rates were 80.8 and 77.7%, respectively. In this retrospective study, 488 pT1–3N0M0 ESCC patients underwent R0 esophagectomy with two-field lymphadenectomy in the absence of either preoperative neoadjuvant or postoperative adjuvant therapy. At 3, 5 and 8 years following the surgery, the OS rates were 73.0, 62.1 and 56.5%, and the DFS rates were 63.7, 53.1 and 46.3%, respectively.
Taken together, even with the slight variation in five-year OS rates among the different studies, the OS remains at approximately 50% for radical esophagectomy coupled with two-field lymphadenectomy without significant improvement for different patient populations or different surgical teams. Chen et al. [19] reported that three-field lymphadenectomy results in five and 10-year OS rates of 71.3 and 57%, respectively, for pT1-4aN0M0 ESCC patients, which were significantly improved compared to the two-field procedure, indicating early lymphatic dissemination might not be confined to regional LN surrounding the lesion. However, Shao et al. [20] showed that the OS was not different between two-field and three-field LN dissection for pN0 ESCC patients. Taken together, the use of three-field LN dissection to potentially improve OS should be further investigated.
To better understand the risk factors associated with the OS of ESCC patients after two-field lymphadenectomy, survival analyses with univariate as well as multivariate Cox regression models were used in the current study. The results indicated that pT1–3N0M0 ESCC patients who presented with neoplasms in the upper-thoracic segment had the worst OS and DFS in comparison to patients with tumors in the middle or lower thoracic segments. Although this was similar to previous studies of EC patients who were mainly operated on through the left thoracic approach [5, 21], it was also contrary to several studies that have demonstrated that the site of the lesion is not associated with prognosis for ESCC patients who are operated on using the right thoracic approach [3, 4, 19, 22]. Therefore, additional studies are required to investigate and validate the true influence that the site of the lesion has on the OS of patients.
Prospectively, preoperative CT assessments may allow for the visualization of potential LN metastases, which can help to determine the surgical approach and procedure that will result in the best long-term prognosis for the patient. Because the surgical method used in this study was the Sweet procedure, this might have led to insufficient mediastinal LN dissection and subsequent potentiation of metastasis of SLNs. As such, the present study identified SLNs in CT prior to surgery as an independent risk factor associated with OS and DFS.
Several studies have suggested that OS was not significantly impacted in patients with middle or lower thoracic EC who underwent a Sweet or Ivor Lewis esophagectomy [23,24,25,26,27], while the study from Ma Q et al. [26] showed that the three- and five-year rates of CSS and OS were better for the pN0 ESCC patients with left transthoracic approaches (eg. Sweet) compared to those with right transthoracic approaches (eg. Ivor Lewis), indicating that the location of cancer impacts the long-term survival of patients.
The pT stage was another important independent factor for OS and DFS in our study as well as other studies. The studies by either Xie et al. [22] and Gao et al. [18] reported that the five-year OS rates were 75.1 and 77.8% for pT1, 50.4 and 54.2% for pT2, and 37.0 and 34% for pT3 ESCC patients with pN0 after two-field surgery, respectively. Chen et al. [19] reported that the five- and 10-year OS rates were 83.8 and 71.9% for pT1N0M0, 78.8 and 67.4% for pT2N0M0, 67.8 and 51.1% for pT3N0M0 ESCC patients after three-field surgery, respectively. Our results also showed that the pT stage was associated with RFS and LRFS, suggesting that early diagnosis and surgical interventions are important for the long-term prognosis of EC patients.
Two-field lymphadenectomy was chosen as the routine procedure for the surgical management of ESCC, and numerous studies have already shown that the number of dissected LNs can influence the long-term mortality of ECSS patients. Xie et al. [22] reported that the five-year OS rates for dissected LN numbers of 0–14, 15–19, 20–24, and ≥ 25 in pT1–3N0M0 ESCC patients were 28.5, 47.7, 56.4 and 60.4% after surgery, respectively. Yang et al. had demonstrated the five-year OS rates for pN0 ESCC patients with dissected LN numbers of < 6, 6–9, 10–17, and ≥ 18 were 40.8, 50.6, 55.9 and 71.4%, respectively [28]. However, Altorki et al. reported that only over 40 LNs dissected could produce significantly better OS rates, compared with less than 16 LNs dissected [13]. A single study [29] has aggressively claimed that the number of dissected LNs is not associated with the OS of pN0 EC patients. Our study found that the five-year OS rates for patients with dissected LNs < 12 and ≥ 12 were 58.5 and 70.2%, respectively. While these data are similar to some of the previous studies, it also suggests that the optimal number of dissected LNs to improve long-term outcomes should be further investigated.
In our study, patient age was associated with OS but not with DFS for pT1–3N0M0 ESCC patients. Chen et al. [19] also showed that the five-year OS rate for pN0 ESCC patients was 76.5% for those younger than 60 years of age and 63.3% for those 60 years of age or older. Other studies [4, 25, 29] have also shown age as an independent factor for OS in ESCC patients.
Recently, nomogram and RPA scores have been used to predict the survival of ESCC patients following surgery and to stratify postoperative patients into varying risk groups. Many studies from various clinic groups have reported their methods to establish nomograms to classify the risk level of the ESCC patient. Zheng et al. [15] selected five independent predictors of OS (gender, age, dissected LNs, pT, and pN status) to evaluate clinical nomograms in ESCC patients after surgery. Yu et al. [16] used the LN metastatic ratio and adjuvant therapy to construct their nomogram and RPA to classify patients with IIB-III ESCC. Ni et al. [17] attempted to include patient age, pTMN stage, and management modalities to classify ESCC. Duan et al. [30] used five independent prognostic variables to build the nomograms to predict DFS and OS of ESCC patients undergoing postoperative chemo and radiation therapy. This prognostic nomogram provided an individualized risk estimate of survival in patients after esophagectomy followed by postoperative chemoradiation therapy. Deng et al. [24] used eight independent risk factors to build the nomogram to predict the OS of patients with pT1N+/T2-4aN0–3, M0 ESCC after surgery. The prognostic efficacy of the nomogram in the training and validation cohorts was significantly greater than that of the American Joint Committee on Cancer (AJCC) staging system.
We classified pT1–3N0M0 ESCC patients into three classes (low, middle, and high risk) according to the RPA scores; the OS, DFS, RFS and LRFS were significantly different among the three classes. For the low-risk group, the five-year OS was > 90% and the recurrence rate was very low. Therefore, postoperative adjuvant therapy is not needed. For the middle-risk group, the five-year OS was approximately 65% and postoperative adjuvant therapy should be considered. For the high-risk group, the five-year OS was approximately 50% and postoperative adjuvant therapy should be strongly recommended. Several studies have shown the value of postoperative adjuvant therapy in pN0 EC patients [18, 19, 31, 32]; however, the adverse effects related to postoperative adjuvant therapy are a considerable hurdle for patients to undertake therapy. Therefore, it may be more reasonable to select postoperative adjuvant therapy based on the likelihood of postoperative survival and/or recurrence in ESCC patients.
Several pitfalls can be found in our study. Firstly, this retrospective case-matched study was conducted with patients from a single-center. Therefore, the possibility of selection bias could not be entirely excluded despite the use of the multivariate analysis. Secondly, most of the patients in our study underwent the left thoracic approach for R0 esophagectomy and two-field lymphadenectomy with a median number of 10 dissected LNs. As such, the data and subsequent conclusions might only be suitable for similar patients. Thirdly, the details of recurrence and salvage therapy were not shown in this study. Salvage therapy might impact the OS of our patients.
Conclusions
In this study, the site of the lesion, SLNs in CT before surgery, and pT stage were established as the independent risk factors that negatively impact OS, DFS, RFS and LRFS, while the age of the patient and the number of dissected LNs were additional risk factors for the OS in pT1–3N0M0 ESCC patients after two-field surgery alone. With these risk factors, a practice-oriented method was proposed with RPA scores, which stratifies the postoperative patients into three degrees of risk: low, medium, and high. This stratification provides guidance regarding the importance of postoperative adjuvant therapy to improve OS.
Availability of data and materials
The dataset(s) supporting the conclusions of this article is (are) included within the article.
Abbreviations
- CSS:
-
Cause-specific survival
- CT:
-
Computed tomography
- DFS:
-
Disease-free survival
- DM:
-
Distant metastases
- EC:
-
Esophageal cancer
- ESCC:
-
Esophageal squamous cell carcinoma
- LN(s):
-
Lymph nodes
- LRFS:
-
Locoregional recurrence-free survival
- LRR:
-
Locoregional recurrence
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- RPA:
-
Recursive partitioning analysis
- SLNs:
-
Small lymph node
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Blot WJ, Tarone RE. Esophageal cancer. In: Thun MJ, Linet MS, Cerhan JR, Haiman CA, Schottenfeld D, editors. Cancer epidemiology and prevention. 4th ed. New York: Oxford University Press; 2017; 2018. p. 579–92.
Wu H, Liu C, Xu M, Guo M, Xu S, Xie M. Prognostic value of the number of negative lymph nodes in esophageal carcinoma without lymphatic metastasis. Thorac Cancer. 2018;9(9):1129–35. https://doi.org/10.1111/1759-7714.12796.
Zhang H, Shang X, Zhu X, Tang P, Chen C, Jiang H, et al. Impact of the number of lymph node examined on the prognosis of esophageal squamous cell carcinoma. Chin J Dig Surg. 2018;17:817–24.
Wang Y, Wang L, Yang Q, Li J, Qi Z, He M, et al. Factors on prognosis in patients of stage pT3N0M0 thoracic esophageal squamous cell carcinoma after two-field esophagectomy. J Cancer Res Ther. 2015;11(Suppl 1):C16–23.
Wang Y, Dong S, Ming H, Jing L, Yang J, Zhan Q, et al. Analysis of risk factors of recurrence of pT1-3N0M0 esophageal squamous cell carcinoma after two-field esophagectomy. Chin J Radiat Oncol. 2018;27:145–9.
Guo XF, Mao T, Gu ZT, Ji CY, Fang WT, Chen WH. Clinical study on postoperative recurrence in patients with pN0 esophageal squamous cell carcinoma. J Cardiothorac Surg. 2014;9(1):150. https://doi.org/10.1186/s13019-014-0150-4.
Liu X, Zhang W, Yu S, Xiao Z, Zhou Z, He J. Pattern of failure after radical surgery among patients with stage T2-3N0M0 esophageal squamous cell carcinoma-potential value of postoperative radiotherapy. Chin J Radiat Oncol. 2015;24:19–24.
Shridhar R, Weber J, Hoffe SE, Almhanna K, Karl R, Meredith K. Adjuvant radiation therapy and lymphadenectomy in esophageal cancer: a SEER database analysis. J Gastrointest Surg. 2013;17(8):1339–45. https://doi.org/10.1007/s11605-013-2192-7.
Chen SB, Weng HR, Wang G, Liu DT, Li H, Zhang H, et al. The impact of adjuvant radiotherapy on radically resected T3 esophageal squamous cell carcinoma. J Cancer Res Clin Oncol. 2016;142(1):277–86. https://doi.org/10.1007/s00432-015-2041-z.
Gockel I, Niebisch S, Campbell LK, Sgourakis G, Junginger T. Prognostic scoring system predictive of survival after surgical resection of esophageal carcinoma. Thorac Cardiovasc Surg. 2013;61(6):470–8. https://doi.org/10.1055/s-0032-1331843.
Stiles BM, Christos P, Port JL, Lee PC, Paul S, Saunders J, et al. Predictors of survival in patients with persistent nodal metastases after preoperative chemotherapy for esophageal cancer. J Thorac Cardiovasc Surg. 2010;139(2):387–94. https://doi.org/10.1016/j.jtcvs.2009.10.003.
Altorki NK, Zhou XK, Stiles B, Port JL, Paul S, Lee PC, et al. Total number of resected lymph nodes predicts survival in esophageal cancer. Ann Surg. 2008;248(2):221–6. https://doi.org/10.1097/SLA.0b013e31817bbe59.
Chen YJ, Schultheiss TE, Wong JY, Kernstine KH. Impact of the number of resected and involved lymph nodes on esophageal cancer survival. J Surg Oncol. 2009;100(2):127–32. https://doi.org/10.1002/jso.21312.
Zheng Y, Fu S, He T, Yan Q, Di W, Wang J. Predicting prognosis in resected esophageal squamous cell carcinoma using a clinical nomogram and recursive partitioning analysis. Eur J Surg Oncol. 2018;44(8):1199–204. https://doi.org/10.1016/j.ejso.2018.04.011.
Yu S, Zhang W, Ni W, Xiao Z, Wang X, Zhou Z, et al. Nomogram and recursive partitioning analysis to predict overall survival in patients with stage IIB-III thoracic esophageal squamous cell carcinoma after esophagectomy. Oncotarget. 2016;7(34):55211–21. https://doi.org/10.18632/oncotarget.10904.
Ni W, Chen J, Xiao Z, Yu S, Zhang W, Zhou Z, et al. Adjuvant radiotherapy for stage pN1M0 esophageal squamous cell carcinoma: results from a Chinese two-center study. Thorac Cancer. 2019;10(6):1431–40. https://doi.org/10.1111/1759-7714.13088.
Gao HJ, Shang XB, Gong L, Zhang HD, Ren P, Shi GD, et al. Adjuvant radiotherapy for patients with pathologic node-negative esophageal carcinoma: a population based propensity matching analysis. Thorac Cancer. 2020;11(2):243–52. https://doi.org/10.1111/1759-7714.13235.
Chen X, Chen J, Zheng X, Chen Y, Lin Y, Zheng Q, et al. Prognostic factors in patients with thoracic esophageal carcinoma staged pT1-4aN0M0 undergone esophagectomy with three-field lymphadenectomy. Ann Transl Med. 2015;3:282.
Shao L, Ye T, Ma L, Lin D, Hu H, Sun Y, et al. Three-field versus two-field lymph node dissection for thoracic esophageal squamous cell carcinoma: a propensity score-matched comparison. J Thorac Dis. 2018;10(5):2924–32. https://doi.org/10.21037/jtd.2018.05.69.
Zhang HL, Liu RL, Shi YT, Wang ZC, Wang BH, Li YJ, et al. Analysis of the survival in patients after surgical resection of thoracic esophageal cancer. Zhonghua Zhong Liu Za Zhi. 2009;31:541–5.
Xie M, Mei X, Tian L, Liu C, Sun X, Zhang Z, et al. The prognostic value of the number of negative lymph nodes in esophageal carcinoma without lymphatic metastasis after esophagectomy. Chin J Thorac Cardiovasc Surg. 2014;30:221–4.
Yang D, Mao YS, He J, Gao SG, Sun KL, Mu JW, et al. Long-term survival of the middle and lower thoracic esophageal cancer patients after surgical treatment through left or right thoracic approach. J Thorac Dis. 2018;10(5):2648–55. https://doi.org/10.21037/jtd.2018.04.45.
Feng Y, Wu N, Yan S, Wang X, Yang Y. Comparison of Ivor Lewis esophagectomy and sweet esophagectomy for the treatment of middle-lower esophageal squamous cell carcinoma. J Thorac Dis. 2019;11(8):3584–92. https://doi.org/10.21037/jtd.2019.07.68.
Wang J, Wei N, Jiang N, Lu Y, Zhang X. Comparison of Ivor-Lewis versus sweet procedure for middle and lower thoracic esophageal squamous cell carcinoma: a STROBE compliant study. Medicine. 2019;98(6):e14416. https://doi.org/10.1097/MD.0000000000014416.
Ma Q, Liu W, Long H, Rong T, Zhang L, Lin Y, et al. Right versus left transthoracic approach for lymph node-negative esophageal squamous cell carcinoma. J Cardiothorac Surg. 2015;10(1):123. https://doi.org/10.1186/s13019-015-0328-4.
Ma J, Zhan C, Wang L, Jiang W, Zhang Y, Shi Y, et al. The sweet approach is still worthwhile in modern esophagectomy. Ann Thorac Surg. 2014;97(5):1728–33. https://doi.org/10.1016/j.athoracsur.2014.01.034.
Yang HX, Xu Y, Fu JH, Wang JY, Lin P, Rong TH. An evaluation of the number of lymph nodes examined and survival for node-negative esophageal carcinoma: data from China. Ann Surg Oncol. 2010;17(7):1901–11. https://doi.org/10.1245/s10434-010-0948-9.
Hsu PK, Huang CS, Wang BY, Wu YC, Chou TY, Hsu WH. The prognostic value of the number of negative lymph nodes in esophageal cancer patients after transthoracic resection. Ann Thorac Surg. 2013;96(3):995–1001. https://doi.org/10.1016/j.athoracsur.2013.04.098.
Duan J, Deng T, Ying G, Huang D, Zhang H, Zhou L, et al. Prognostic nomogram for previously untreated patients with esophageal squamous cell carcinoma after esophagectomy followed by adjuvant chemotherapy. Jpn J Clin Oncol. 2016;46(4):336–43. https://doi.org/10.1093/jjco/hyv206.
Deng W, Yang J, Ni W, Li C, Chang X, Han W, et al. Postoperative radiotherapy in pathological T2-3N0M0 thoracic esophageal squamous cell carcinoma: interim report of a prospective, phase III, randomized controlled study. Oncologist. 2020;25(4):e701–8. https://doi.org/10.1634/theoncologist.2019-0276.
Deng W, Zhang W, Yang J, Ni W, Yu S, Li C, et al. Nomogram to predict overall survival for thoracic esophageal squamous cell carcinoma patients after radical esophagectomy. Ann Surg Oncol. 2019;26(9):2890–8. https://doi.org/10.1245/s10434-019-07393-w.
Acknowledgments
None
Funding
None
Author information
Authors and Affiliations
Contributions
(I) Conception and Q4 design: Zhan Qi, Ming He and Yuxiang Wang. (II) Administrative support: Zhan Qi, Ming He and Yuxiang Wang. (III) Provision of study materials or patients: Zhan Qi, Yuanping Hu, Rong Qiu, Ming He and Yuxiang Wang. (IV) Collection and assembly of data: Zhan Qi, Yuanping Hu, Rong Qiu, Juan Li, Yuekao Li. (V) Data analysis and interpretation: Zhan Qi,Yuanping Hu, Rong Qiui, Ming He and Yuxiang Wang. (VI) Manuscript writing: All authors. (VII) Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Medical Ethics Committee of our hospital(2017MEC063), and written informed consent was obtained from all patients enrolled in this study.
Consent for publication
Written informed consent was obtained from all patients enrolled in this study.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qi, Z., Hu, Y., Qiu, R. et al. Survival risk prediction model for patients with pT1–3 N0M0 esophageal squamous cell carcinoma after R0 esophagectomy with two-field lymphadenectomy for therapeutic purposes. J Cardiothorac Surg 16, 121 (2021). https://doi.org/10.1186/s13019-021-01503-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01503-0