Abstract
Background
Esophageal cancer has a poor prognosis. Surgery is the main treatment but involves a high risk of complications. Some surgical strategies have tried to eliminate complications. Our meta-analysis tried to find the benefits of single-lumen endotracheal tube intubation with carbon dioxide (CO2) inflation.
Methods
A systematic search of studies on esophagectomy and CO2 inflation was conducted using PubMed, Medline, and Scopus. The odds ratio of post-operative pulmonary complications and anastomosis leakage were the primary outcomes. The standardized mean difference (SMD) in post-operative hospitalization duration was the secondary outcome.
Results
The meta-analysis included four case-control studies with a total of 1503 patients. The analysis showed a lower odds ratio of pulmonary complications in the single-lumen endotracheal tube intubation in the CO2 inflation group (odds ratio: 0.756 [95% confidence interval, CI: 0.518 to 1.103]) compared to that in the double-lumen endotracheal tube intubation group, but anastomosis leakage did not improve (odds ratio: 1.056 [95% CI: 0.769 to 1.45])). The SMD in hospitalization duration did not show significant improvement. (SMD: -0.141[95% CI: − 0.248 to − 0.034]).
Conclusions
Single-lumen endotracheal tube intubation with CO2 inflation improved pulmonary complications and shortened the hospitalization duration. However, no benefit in anastomosis leakage was observed.
Similar content being viewed by others
Background
Esophageal cancer has poor overall survival because of delayed diagnosis. Surgery (esophagectomy) followed by chemoradiotherapy is the main treatment strategy. However, the surgical procedure will carry a high risk of morbidity such as pulmonary complications, anastomosis leakage, and long hospitalization duration.
Surgeons are interested in decreasing post-operative complications and have developed methods to improve outcomes. Some studies focused on the anesthesia method with single-lumen endotracheal tube intubation with artificial pneumothorax induced by carbon dioxide (CO2) inflation. The first published single lumen intubation compared double lumen intubation anethesia in esophagectomy is Ruixiang Zhang et. al. in Interactive Cardiovascular and Thoracic Surgery 2014 [1]. We knew single lumen intubation is benefit in minimal invasive esophagectomy to approach lymph nodes around left recurrent laryngeal nerve and some published studies adopted this surgical intervention [2]. However, some hospital did not familiar with this method. Some literature even suggested carbon dioxide insufflation is not necessary such as Fernando A Herbella et. al in Word Journal of Gastroenterology 2010 [3]. Although double lumen intubated for anethesia with one lung ventilation could get better surgical field, hoarsness, tracheal injury and lung injury induced by one lung ventilation may get worse result after operation. In current clinical practice, minimally invasive esophagectomy performed by single lumen intubation is a trend to get better exposure of left recurrent laryngeal nerve injury. However, it remains some debate between using carbon dioxide insufflation or not. Our meta-analysis tried to compare single-lumen endotracheal tube intubation anesthesia plus CO2 inflation with double-lumen endotracheal tube intubation.
We present the following article in accordance with the PRISMA reporting checklist.
Methods
Search strategy and inclusion criteria
PubMed, Medline, and Scopus were searched for studies with keywords including “artificial pneumothorax or CO2” and “esophagectomy or VATS.” A total 136 results were found. We excluded literature which were not written in English and were not human studies. We also excluded robotic surgery, case reports, and literature reviews. Studies on minimally invasive esophagectomy using single-lumen intubation with CO2 inflation were included.
All included studies were case control studies. All retrieved studies were required to include two treatment arms. One was CO2 inflation for induction of artificial pneumothorax and intubated with single-lumen endotracheal tube. The other was traditional one-lung ventilation by double-lumen endotracheal tube intubation. The target population included patients diagnosed with esophageal cancer.
Data extraction and quality assessment
Three reviewers critically read all the studies that were included in our analysis and extracted the data. We recorded the year, first author, number of treatment arms, and results concerning three different parameters, including pulmonary complications, anastomosis leakage, and hospitalization duration. The quality of enrolled studies was evaluated by the two reviewers using the Newcastle-Ottawa Scale. The scale includes three parts for the case control study, namely, “SELECTION” (4 items), “COMPARABILITY” (1 item), and “EXPOSURE” (3 items). Disagreements between reviewers were discussed by other authors and the corresponding author.
Data synthesis and analysis
The odds ratios (ORs) of post-operative pulmonary complications and anastomosis leakage in the single-lumen endotracheal tube intubation in the CO2 artificial pneumothorax group (SLET group) compared with those in the double-lumen endotracheal tube intubation group (DLET group) were the primary outcomes. The standardized mean difference (SMD) in post-operative hospitalization duration in SLET group compared with that in the control group comprised the secondary outcome. A random effects model was employed to pool individual SMDs and ORs. The heterogeneity was determined by I2 tests, in which values > 50% were regarded as obvious heterogeneity. Potential publication bias was examined by Egger’s test and Funnel plots. Statistical significance was defined as p-value < 0.05. All statistical analyses were performed using Comprehensive MetaAnalysis software, version 3 (Biostat, Englewood, NJ, USA).
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This article used published accessible literature without containing deeply personal, sensitive, or confidential information from participants. Therefore, institutional review board approval is not necessary.
Results
Study search and characteristics of included patients
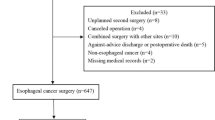
We searched the databases and retrieved 136 results. After reviewing their title, abstract, and keywords, 15 papers were selected for meticulous commentary by the reviewers. We excluded papers which did not meet our inclusion criteria (Fig. 1). Four studies were excluded because they were case series that did not compare CO2 inflation and traditional one-lung ventilation [4,5,6,7]. Two studies were excluded because one introduced a surgical technique with CO2 inflation in esophagectomy [8], and the other showed a video-assisted thoracoscopic surgical procedure [9]. One study was excluded because it was a case control study that compared different surgical positions [10]. One study was an editorial discussion [11]. One study discussed about differences in coagulation between DLET and SLET groups [12]. Two studies were literature reviews [13, 14]. Finally, four case control studies were included in this meta-analysis [1, 15,16,17].
The final quantitative analysis included 915 patients in the DLET group and 588 patients in the SLET group. The age ranges were from 53.91 to 76.9 years in the DLET group and 53.48 to 80 years in the SLET group. Patient characteristics, study methodology, and quality assessment of included trials are listed in Table 1. The detail of quality assessment of included trials is listed in Table 2.
Pooled odds ratio of pulmonary complication, anastomosis leakage, and SMDs in post-operative hospitalization duration
The pooled odds ratio for pulmonary complications in SLET group versus DLET group was 0.756 (95% confidence interval [CI]: 0.518 to 1.103) (Fig. 2a). If we excluded the study by Zhang [1] because all groups in the study used CO2 inflation, the pooled odds ratio was 0.775 (95% CI: 0.520 to 1.154) (Fig. 2b). The pooled odds ratio for anastomosis leakage in SLET group versus DLET group was 1.056 (95% CI: 0.769 to 1.451) (Fig. 3a). If we excluded the study by Zhang [1], the pooled odds ratio was 1.041 (95% CI: 0.753 to 1.439) (Fig. 3b). The standardized mean difference (SMD) concerning hospitalization duration in SLET group versus DLET group was − 0.141 (95% CI: − 0.248 to − 0.034) (Fig. 4a). If we excluded the study by Zhang [1], the SMD was − 0.136 (95% CI: − 0.248 to − 0.024) (Fig. 4b).
The Egger’s test revealed no significant publication bias concerning the overall odds ratio for pulmonary complications and anastomosis leakage (p = 0.348) and overall SMDs in hospitalization duration (p = 0.023). The funnel plots for log odds ratio for pulmonary complications and SMD in hospitalization duration are shown in Fig. 5a and b, respectively.
Discussion
Esophagectomy is a complicated surgery which leads to high post-operative complications, morbidity, and mortality. Although minimally invasive esophagectomy can decrease hospitalization duration, it is still associated with a high post-operative risk. Double-lumen intubation with one-lung ventilation to get better surgical field exposure is a widely used anesthesia strategy, but it increases the rate of acute lung injury and increases pulmonary complications. It is difficult to perform and maintain induction and intubation with this strategy [18]. Double lumen endotracheal tube intubation and one lung ventilation may provide better surgical working field. However, this procedure need perform under bronchoscope to set exact tube position which is higher cost than single lumen endotracheal tube intubation. One lung ventilation method also easily led to barotrauma of dependent lung and lung atelectasis in the working site. These problems will increase complication after procedure [19]. Owing to the difficult manipulation regarding ventilation setting, post-operative pulmonary complications occur frequently in procedures with an extended surgical duration, such as esophagectomy [20].
Some surgeons have tried to use CO2 inflation to induce artificial pneumothorax and prevent one-lung ventilation. Most of these studies were case control series comparing double-lumen endotracheal tube intubation with one-lung ventilation to single-lumen endotracheal tube intubation with two-lung ventilation and CO2 inflation. All of them showed similar results in DLET and SLET groups but failed to mention whether there were differences in the rate and severity of complications.
The present meta-analysis focuses on the pulmonary complications, anastomosis leakage, and hospitalization duration in the two groups. We included four papers related to double-lumen endotracheal tube intubation and single-lumen endotracheal tube intubation. One of these studies [1] used CO2 inflation in both groups, whereas the others used CO2 inflation in the SLET group alone.
Compared with the DLET group, we found fewer pulmonary complications and shorter hospitalization duration in the SLET group, but the difference was not significant. In the comparison of anastomosis leak, we did not see better results in the SLET group. In these studies, the SLET group maintained ventilation in both lungs and prevented one-lung ventilation, which causes oxidative stress, capillary shear stress, and reperfusion injury. This may lead to better results in terms of pulmonary complications and hospitalization duration. As pulmonary complications improved and systemic inflammation reactions decreased [21], anastomosis leakage should also improve. However, this was not observed in the present analysis. Different surgeons bias may lead to the strange results in anastomosis leakage.
There are several limitations to our meta-analysis. First, all the included papers were case control studies. Plenty of bias could be predicted in these studies and lacked detail pre-operative parameters for analysis. No randomized control trial or prospective study can be conducted into meta-analysis for better evidence. These problems will decrease the evidence level of the meta-analysis. Second, each study used different CO2 inflation strategies; one even used CO2 inflation in both comparison groups. Meta-analysis is focused on published literatures. If these literatures did not list these preoperative parameters, we could not perform analysis. We will add limitation in the discussion to talk about this problem. We also tried to request raw data by contact with authors, but no one responded. Without raw data, we could not know these patients’ characters before surgical intervention and bias will conduct into our analysis. Third, pulmonary complications are difficult to define clearly. We found that pulmonary complications included thorax infection, pulmonary infection, and pulmonary atelectasis in the study by Zhang [1]; respiratory complications in the study by Miao [14]; pneumonia, atelectasis, and ARDS in the study by Ninomiya [15]; and respiratory complications in the study by Shinsuke [17]. Each of them defined pulmonary complications differently, which may have increased the bias of the results.
Based on these limitations, future research involving esophagectomy under SLET should focus on a randomized control study and define protocols of CO2 inflation and criteria for pulmonary complications.
Conclusions
In this meta-analysis, single-lumen intubation anesthesia with artificial pneumothorax induced by CO2 inflation was observed to be a better option for minimally invasive esophagectomy. The odds ratio for pulmonary complications and SMDs in hospitalization duration decreased in this surgical setting. Therefore, our meta-analysis survey suggested that single-lumen intubation with CO2-induced artificial pneumothorax should be taken into consideration for minimally invasive esophagectomy.
Availability of data and materials
All data generated or analysed during this study are included in this published article (and its supplementary information files.)
Abbreviations
- VATS:
-
Video-assisted thoracoscopic surgery
- CI:
-
Confidence interval
- DLET:
-
Double-lumen endotracheal tube intubation
- SLET:
-
Single-lumen endotracheal tube intubation
- SMD:
-
Standardized mean difference
References
Zhang R, Liu S, Sun H, Liu X, Wang Z, Qin J, et al. The application of single-lumen endotracheal tube anaesthesia with artificial pneumothorax in thoracolaparoscopic oesophagectomy. Interact Cardiovasc Thorac Surg. 2014;19(2):308–10. https://doi.org/10.1093/icvts/ivu100.
Biere SSAY, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet. 2012;379(9829):1887–92. https://doi.org/10.1016/S0140-6736(12)60516-9.
Herbella FA, Patti MG. Minimally invasive esophagectomy. World J Gastroenterol. 2010;16(30):3811–5. https://doi.org/10.3748/wjg.v16.i30.3811.
Peden CJ, Prys-Roberts C. Capnothorax: implications for the anaesthetist. Anaesthesia. 1993;48(8):664–6. https://doi.org/10.1111/j.1365-2044.1993.tb07174.x.
Saikawa D, Okushiba S, Kawata M, Okubo T, Kitashiro S, Kawarada Y, et al. Efficacy and safety of artificial pneumothorax under two-lung ventilation in thoracoscopic esophagectomy for esophageal cancer in the prone position. Gen Thorac Cardiovasc Surg. 2014;62(3):163–70. https://doi.org/10.1007/s11748-013-0335-0.
Zhang Y, Duan R, Xiao X, Pan T. Minimally invasive esophagectomy with right bronchial occlusion under artificial pneumothorax. Dig Surg. 2015;32(2):77–81. https://doi.org/10.1159/000371747.
Bai Y, Zhou Y, Lu XH. Single-lumen tracheal ventilation for minimally invasive esophagectomy in patients with esophageal cancer. J Cancer Res Ther. 2016;12:C277–c80.
Mao T, Fang W, Gu Z, Guo X, Ji C, Chen W. Video-assisted thoracolaparoscopic esophagectomy: the experience of Shanghai chest hospital. J Thor Dis. 2013;5(6):906–9. https://doi.org/10.3978/j.issn.2072-1439.2013.12.14.
Gallego-Poveda J, Guerra NC, Carvalheiro C, Ferreira H, Sena A, Junqueira N, et al. Use of CO2 in video assisted thoracic surgery and single-lumen endotracheal tube-a new less invasive approach. J Thor Dis. 2017;9(4):903–6. https://doi.org/10.21037/jtd.2017.01.53.
Kaburagi T, Takeuchi H, Kawakubo H, Omori T, Ozawa S, Kitagawa Y. Clinical utility of a novel hybrid position combining the left lateral decubitus and prone positions during thoracoscopic esophagectomy. World J Surg. 2014;38(2):410–8. https://doi.org/10.1007/s00268-013-2258-4.
Takeuchi H, Kitagawa Y. Two-lung ventilation in the prone position: is it the standard anesthetic management for thoracoscopic esophagectomy? Gen Thorac Cardiovasc Surg. 2014;62(3):133–4. https://doi.org/10.1007/s11748-014-0373-2.
Mao QX, Guo W, Huang BQ, Yan H. Impact of artificial capnothorax on coagulation in patients during video-assisted thoracoscopic esophagectomy for squamous cell carcinoma. Surg Endosc. 2016;30(7):2766–72. https://doi.org/10.1007/s00464-015-4549-3.
Suda K, Nakauchi M, Inaba K, Ishida Y, Uyama I. Minimally invasive surgery for upper gastrointestinal cancer: our experience and review of the literature. World J Gastroenterol. 2016;22(19):4626–37. https://doi.org/10.3748/wjg.v22.i19.4626.
Lin M, Shen Y, Feng M, Tan L. Is two lung ventilation with artificial pneumothorax a better choice than one lung ventilation in minimally invasive esophagectomy? J Thor Dis. 2019;11(S5):S707–s12. https://doi.org/10.21037/jtd.2018.12.08.
Ninomiya I, Okamoto K, Fushida S, Oyama K, Kinoshita J, Takamura H, et al. Efficacy of CO2 insufflation during thoracoscopic esophagectomy in the left lateral position. Gen Thorac Cardiovasc Surg. 2017;65(10):587–93. https://doi.org/10.1007/s11748-017-0816-7.
Lin M, Shen Y, Wang H, Fang Y, Qian C, Xu S, et al. A comparison between two lung ventilation with CO2 artificial pneumothorax and one lung ventilation during thoracic phase of minimally invasive esophagectomy. J Thor Dis. 2018;10(3):1912–8. https://doi.org/10.21037/jtd.2018.01.150.
Nomura S, Tsujimoto H, Ishibashi Y, Fujishima S, Kouzu K, Harada M, et al. Efficacy of artificial pneumothorax under two-lung ventilation in video-assisted thoracoscopic surgery for esophageal cancer. Surg Endosc. 2020;34(12):5501–7. https://doi.org/10.1007/s00464-019-07347-z.
Blank RS, Colquhoun DA, Durieux ME, Kozower BD, McMurry TL, Bender SP, et al. Management of one-lung ventilation: impact of tidal volume on complications after thoracic surgery. Anesthesiology. 2016;124(6):1286–95. https://doi.org/10.1097/ALN.0000000000001100.
Cerfolio RJ, Bryant AS, Sheils TM, Bass CS, Bartolucci AA. Video-assisted thoracoscopic surgery using single-lumen endotracheal tube anesthesia. Chest. 2004;126(1):281–5. https://doi.org/10.1378/chest.126.1.281.
Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg. 2015;121(2):302–18. https://doi.org/10.1213/ANE.0000000000000808.
Zhang BJ, Tian HT, Li HO, Meng J. The effects of one-lung ventilation mode on lung function in elderly patients undergoing esophageal cancer surgery. Medicine. 2018;97(1):e9500. https://doi.org/10.1097/MD.0000000000009500.
Acknowledgements
We would like to thank Editage for providing language editing assistance.
Funding
None.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: CML. (II) Administrative support: YC, LCC, HIL, YHC, SHL. (III) Provision of study materials or patients: All authors. (IV) Collection and assembly of data: All authors. (V) Data analysis and interpretation: CML. (VI) Manuscript writing: KHC, HHL. (VII) Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This article used published accessible literature without containing deeply personal, sensitive or confidential information from participants. Therefore, institutional review board approval is not necessary.
Consent for publication
Not applicable.
Competing interests
All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chuang, KH., Lai, HH., Chen, Y. et al. Improvement of surgical complications using single-lumen endotracheal tube intubation and artificial carbon dioxide pneumothorax in esophagectomy: a meta-analysis. J Cardiothorac Surg 16, 100 (2021). https://doi.org/10.1186/s13019-021-01459-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01459-1