Abstract
Background
One lung ventilation (OLV) is the technique used during lung resection surgery in order to facilitate optimal surgical conditions. OLV may result in hypoxemia due to the shunt created. Several techniques are used to overcome the hypoxemia, one of which is continuous positive airway pressure (CPAP) to the non-dependent lung. Another technique is ventilating the non-dependent lung with a minimal volume, thus creating differential lung ventilation (DLV). In this study we compared the efficacy of CPAP to DLV during video assisted thoracoscopic lung resection.
Patients and method
This is a prospective study of 30 adult patients undergoing elective video assisted thoracoscopic lung lobectomy. Each patient was ventilated in four modes: two lung ventilation, OLV, OLV + CPAP and OLV + DLV. Fifteen patients were ventilated with CPAP first and DLV next, and the other 15 were ventilated with DLV first and then CPAP. Five minutes separated each mode, during which the non-dependent lung was open to room air. We measured the patient’s arterial blood gas during each mode of ventilation. The surgeons, who were blinded to the ventilation technique, were asked to assess the surgical conditions at each stage.
Results
Oxygenation during OLV+ CPAP was significantly lower that OLV + DLV (p = 0.018). There were insignificant alterations of pH, PCO2 and HCO3 during the different ventilating modes. The surgeons’ assessments of interference in the field exposure between OLV + CPAP or OLV + DLV was found to be insignificant (p = 0.073).
Conclusions
During OLV, DLV is superior to CPAP in improving patient’s oxygenation, and may be used where CPAP failed.
Trial registration
ClinicalTrials.gov NCT03563612. Registered 9 June 2018, retrospectively (due to clerical error).
Similar content being viewed by others
Introduction
During lung resection surgery, optimal surgical access is attained when the operated lung is deflated and its movements are avoided. This is achieved by one lung ventilation (OLV) [1]. Ventilation of one lung creates a trans-pulmonary shunt through the non-ventilated lung and causes hypoxemia [2, 3]. Both mechanical factors, such as gravitation and pressure by the surgeon, and the physiological response, mainly hypoxic pulmonary vasoconstriction, decrease the shunt [4, 5]. The hypoxemia is usually not severe; however, in some cases, life threatening hypoxemia occurs that responds poorly to corrective maneuvers [6]. Applying positive end expiratory pressure (PEEP) to the dependent lung and ventilating with 100% oxygen, are initial steps. In case there is no improvement in oxygenation, additional techniques are used. One technique is insufflating oxygen with a constant pressure to the non-dependent lung, called continuous positive airway pressure (CPAP). Another option is to ventilate the non-dependent lung with a minimal volume and rate, creating differential lung ventilation (DLV). Both techniques may impair exposure to the operated area to some extent.
The purpose of this study is to compare ventilation modalities during OLV, which may improve oxygenation with minimal impairment of the surgical field conditions. In this study, the non-dependent lung was ventilated alternately, in crossover fashion, by CPAP and by a portable ventilator with low rate and pressure in a DLV technique [7,8,9]. We anticipated that a low ventilation rate and pressure would produce the least interference with the surgeon’s exposure and, at the same time, improve oxygenation.
Patients and methods
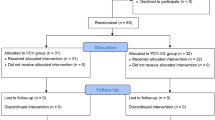
This is a prospective randomized controlled crossover study of adult patients scheduled to have video-assisted thoracoscopic surgery (VATS) of lung lobectomy under general anesthesia. The study was approved by the institution local Ethic Committee and registered (ClinicalTrials.gov NCT03563612). The patients had a detailed explanation of the study before the surgery by one of the anesthesiologists who took part in this study, and signed an inform consent if they agreed to participate.
Exclusion criteria included: American Society of Anesthesiologists (ASA) grade ≥ 4, pregnancy, and difficult intubation. Decreased oxygen saturation below 85% at any time during the surgery was set as an end point, at which the study would be stopped. The primary outcome variables are the PaO2 measurements, while the secondary outcome variables are the spirometry measurements and the surgeons’ evaluation of the surgical field.
Study protocol
On arrival in the operating room, an intravenous line was placed. Each patient was monitored with an electrocardiogram, pulse oximeter, invasive blood pressure, end tidal capnography, and eosophageal thermometer. Following the induction of general anesthesia using fentanyl 2–5 microgram/kg; propofol 1–3 mg/kg and rocuronium 0.6–0.8 mg/kg, the trachea was intubated with a left double lumen tracheal tube VivaSight (ETView Ltd. Misgav Business Park, Israel) where verification of the tube position was monitored continuously with on-line video surveillance. The dependent lung was ventilated by anesthesia machine (Dräger Narkomed 2A) with sevoflurane for maintenance of anesthesia.
Ventilation parameters were as follows: volume controlled mode with tidal volume was set to 8 ml/kg during two lung ventilation (TLV) and reduced to 6 ml/kg during OLV; respiratory rate of 10–12 breaths per minute during TLV, increased to 12–15 per minute during OLV, adjusted to keep PaCO2 below 50 mmHg; inspired oxygen of 100% at all times; positive end expiratory pressure (PEEP) was 2 cm H2O, first in both lungs and then in the dependent lung during OLV. All patients were placed in the lateral decubitus position for surgery.
When OLV was initiated, the non- dependent lung was open to the atmosphere. Ten minutes after the first trocar was introduced, measurements were recorded and then the operated lung was either connected to a CPAP system or to a small portable time-cycled ventilator paraPAC-2D (Transport Ventilator, SIMS pneuPAC Ltd., Luton, UK). The order of intervention was randomized by one of the researchers (MB), using computerized software (random.org). The CPAP pressure was set to 5 cm H2O. Differential Lung Ventilation of the non-dependent lung was set at a rate of 8 breaths per minute, inspired gas 100% oxygen, peak pressure and tidal volume set to the lowest available values, resulting in a peak pressure of 10 cm H2O and a tidal volume around 50 ml. The treatment of the operated lung was alternated with a 5-min interval between modes of ventilation, without additional ventilatory support or oxygen insufflations, to avoid the influence of one modality upon the other. In that 5 min interval, the tube connection of the non-dependent lung was opened to room air.
Measurements
Demographic data regarding the patients’ age, weight, gender and ASA classification was recorded. Arterial blood gas, peak inspiratory pressure (PIP), and plateau pressure (Pplat) were measured during: two lung ventilation, OLV (10 min after the first trocar was introduced), OLV+ CPAP and OLV+ DLV. PIP and Pplat were recorded from the anesthesia machine spirometer. At the same time, the chief surgeon was asked to comment on the surgical field conditions. The surgeon’s evaluation was graded from 0 (no interference) to 3 (maximal interference). The surgeons were blinded to the ventilation mode used at that time since the patient’s sterile covers were pulled up, concealing the anesthesia machine and the ventilator.
Statistical analysis
Sample size was calculated assuming difference in PaO2 between CPAP and mini-ventilation of 50 mmHg; a safety level of 95%; standard deviation of 60; intensity of 80% and measurement ratio of 1:1. Comparison between the groups of patients was performed using the Mann Whitney non-parametric test. Data of the arterial blood gas and spirometry variables during the different ventilation techniques were compared with Wilcoxon non-parametric test. Surgeons’ estimations of interference with the surgical field were compared with the chi-square test. Differences were considered statistically significant at p < 0.05.
Results
Thirty patients were recruited as participants. One patient in the group that had DLV first was excluded, due to difficulty in tracheal intubation. No significant difference was found between the two groups, CPAP first or DLV first, in all studied variables. Participant’s demographics are shown in Table 1 and data regarding the surgery in Table 2.
Regarding arterial blood gas: oxygenation reduced significantly when changing from two lung ventilation to OLV (Fig. 1). Oxygenation during OLV+ CPAP was significantly lower that OLV + DLV (p = 0.018). Alterations of PCO2, pH and HCO3 during the different ventilating modes were not significant (Figs. 2, 3, 4 respectively).
No significant difference was noted between peak and plateau pressures during OLV, OLV + CPAP or OLV + DLV.
Regarding the surgeons’ assessment of interference in surgical field exposure:
None of the patients was graded as 3, where interference is maximal. One patient was graded as 1 during CPAP and 2 during DLV. One patient was graded as 2 for both techniques. The rest of the patients received 0 interference for CPAP while six had 1 grade interference with DLV (p = 0.073).
Discussion
In this study we found that DLV is superior to CPAP as mean for improving patient’s oxygenation during OLV. The theoretical explanation for DLV superiority relies on the physiologic phenomenon of heterogeneity in different areas in the lung [10, 11]. Ventilating both lungs with the same pressure results in fresh gas flow ventilating the lower resistance parts of the lung, while the areas with high resistance, such as atalectatic areas, remain unventilated. Heterogeneous lung aeration may result in lung inflammation and injury, which deteriorates gas exchange furthermore [12, 13]. Ventilating independently different parts of the lung with different pressures may help force the air into atalectatic parts, reduce V/Q mismatch and improve oxygenation [14, 15]. This theory is supported by experimental models [7, 12]. Clinical trials showed a similar beneficial effect of DLV in patients in intensive care units [16,17,18] and during open thoracic surgery [9, 19]. However, we found no data regarding DLV during thoracoscopic surgery.
Theoretically, changing ventilation may improve oxygenation indirectly by reducing CO2 levels, according to the formula: PaO2 = FiO2 (Pbr-PH2O)-PCO2/K. However, we found no significant change in CO2 in this study. Thus, improved oxygenation was not the outcome of CO2 levels.
The main disadvantage of DLV, as with CPAP, is that both may interfere with surgical field exposure. Spirometry of the dependent lung was recorded in order to find whether the different ventilation modes of the non-dependent lung influence the dependent one. No significant difference was found.
An important weakness of this study relies on its design as a cross-over study. There is a possibility of carry-over effects and its influence on interpretation of the findings. In order to overcome it we set a period of 5-min interval between modes of ventilation, without additional ventilatory support or oxygen insufflations. In that 5 min interval, the tube connection of the non-dependent lung was opened to room air. We assume that this time interval was long enough to allow patient’s oxygenation return to its baseline. Another problem was the non-significant results of the surgical exposure assessment (p = 0.073). This marginally non-significant result may be caused by Type II error, and may have been different in a larger scale study. The surgeons were blinded to the mode of ventilation, yet the anesthesiologist was not. This may have set additional error to the study.
In the past decades, when cardio-thoracic surgery became minimally invasive, good lung deflation became a necessity. Video- and robot- assisted thoracoscopic operations require high quality OLV [20, 21]. Moreover, many of these procedures are performed with the patient in the supine position, with a large shunt and low oxygenation. At the same time, the patient often has poor basic lung functions, and hypoxemia occurs rapidly. Patients with ischemic heart disease who undergo coronary artery bypass graft are especially susceptible to injury during hypoxemia, and aggressive treatment of arterial desaturation is mandatory to ensure the patient’s safety [22, 23]. The challenge of the anesthesiologist is to overcome hypoxemia without disturbing exposure of the surgical field. We believe the DLV is an additional tool for improving oxygenation during OLV.
Conclusions
The use of DLV while ventilating one lung may improve patient’s oxygenation, and was found to be better than CPAP. Differential lung ventilation may be used where CPAP failed.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- CPAP:
-
Continuous positive airway pressure
- DLV:
-
Differential lung ventilation
- OLV:
-
One lung ventilation
- PEEP:
-
Positive end expiratory pressure
- PIP:
-
Peak inspiratory pressure
- Pplat:
-
Plateau pressure
- VATS:
-
Video-assisted thoracoscopic surgery
References
Kirschner PA. The surgery-anesthesia relationship: a surgeon’s view. In: Cohen E, editor. The Practice of Thoracic Anesthesia. Philadelphia: JB Lippincott Company; 1995. p. 163–80.
Karzai W, Schwarzkopf K. Hypoxemia during one-lung ventilation: prediction, prevention, and treatment. Anesthesiology. 2009;110:1402–11.
Cohen E. Management of one-lung ventilation. Anesthesiol Clin N Am. 2001;19:475–95.
Nomoto Y. Perioperative pulmonary blood flow and one lung anesthesia. Can J Anaesth. 1987;34:447.
Benumof JL. One lung ventilation and hypoxic pulmonary vasoconstriction: implications for anesthetic management. Anesth Analg. 1985;64:821.
Mierdl S, Meininger D, Dogan S, et al. Does poor oxygenation during one-lung ventilation impair aerobic myocardial metabolism in patients with symptomatic coronary artery disease? Interact Cardiovasc Thorac Surg. 2007;6:209–13.
Borges JB, Senturk M, Ahlgren O, Hedenstierna G, Larsson A. Open lung in lateral decubitus with differential selective positive end-expiratory pressure in an experimental model of early acute respiratory distress syndrome. Crit Care Med. 2015;43:e404–11.
Skjeflo GW, Dybwik K. A new method of securing the airway for differential lung ventilation in intensive care. Acta Anaesthesiol Scand. 2014;58:463–7.
Shechtman MY, Ziser A, Barak M, Ben-Nun A. Mini-ventilation for improved oxygenation during lung resection surgery. Anaesth Intensive Care. 2011;39:456–9.
Aliverti A, Pennati F, Salito C, Woods JC. Regional lung function and heterogeneity of specific gas volume in healthy and emphysematous subjects. Eur Respir J. 2013;41:1179–88.
Kaminsky DA, Irvin CG, Lundblad LK, et al. Heterogeneity of bronchoconstriction does not distinguish mild asthmatic subjects from healthy controls when supine. J Appl Physiol (1985). 2008;104:10–9.
Tojo K, Nagamine Y, Yazawa T, et al. Atelectasis causes alveolar hypoxia-induced inflammation during uneven mechanical ventilation in rats. Intensive Care Med Exp. 2015;3:56.
Bowser JL, Lee JW, Yuan X, Eltzschig HK. The hypoxia-adenosine link during inflammation. J Appl Physiol (1985). 2017;123:1303–20.
Klingstedt C, Baehrendtz S, Bindslev L, Hedenstierna G. Lung and chest wall mechanics during differential ventilation with selective PEEP. Acta Anaesthesiol Scand. 1985;29:716–21.
Siegel JH, Stoklosa JC, Borg U, et al. Quantification of asymmetric lung pathophysiology as a guide to the use of simultaneous independent lung ventilation in posttraumatic and septic adult respiratory distress syndrome. Ann Surg. 1985;202:425–39.
Anantham D, Jagadesan R, Tiew PEC. Clinical review: independent lung ventilation in critical care. Crit Care Lond Engl. 2005;9:594–600.
Yamakawa K, Nakamori Y, Fujimi S, Ogura H, Kuwagata Y, Shimazu T. A novel technique of differential lung ventilation in the critical care setting. BMC Res Notes. 2011;4:134.
Wickerts CJ, Blomqvist H, Baehrendtz S, Klingstedt C, Hedenstierna G, Frostell C. Clinical application of differential ventilation with selective positive end-expiratory pressure in adult respiratory distress syndrome. Acta Anaesthesiol Scand. 1995;39:307–11.
Baraka A, Muallem M, Baroody MA, Sibai AN, Usta N, Sibai AM. Differential lung ventilation during thoracotomy. Middle East J Anaesthesiol. 1988;9:357–62.
Umari M, Falini S, Segat M, et al. Anesthesia and fast-track in video-assisted thoracic surgery (VATS): from evidence to practice. J Thorac Dis. 2018;10(Suppl 4):S542–S54.
Seco M, Edelman JJ, Yan TD, Wilson MK, Bannon PG, Vallely MP. Systematic review of robotic-assisted, totally endoscopic coronary artery bypass grafting. Ann Cardiothorac Surg. 2013;2:408–18.
Liu TJ, Shih MS, Lee WL, et al. Hypoxemia during one-lung ventilation for robot-assisted coronary artery bypass graft surgery. Ann Thorac Surg. 2013;96:127–32.
Deshpande SP, Lehr E, Odonkor P, et al. Anesthetic management of robotically assisted totally endoscopic coronary artery bypass surgery (TECAB). J Cardiothorac Vasc Anesth. 2013;27:586–99.
Acknowledgments
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
RK: study design. WA: study design and data collection. OH: patient recruitment and data analyzing. MA: manuscript preparation. MB: study design, data collection and manuscript preparation. Review of manuscript: all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institution local Ethic Committee and all the patients included signed an inform consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kremer, R., Aboud, W., Haberfeld, O. et al. Differential lung ventilation for increased oxygenation during one lung ventilation for video assisted lung surgery. J Cardiothorac Surg 14, 89 (2019). https://doi.org/10.1186/s13019-019-0910-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-019-0910-2