Abstract
Background
In recent years, surgical outcomes have improved, and positive reports on surgery for type A aortic dissection (AAD) in the elderly are increasing. However, the difference between surgical and conservative treatments in the elderly remains unclear. Therefore, we conducted this study to determine whether surgery should be performed for Stanford (AAD) in elderly patients.
Methods
Data of patients aged 80 years or older who were hospitalized for AAD from April 2014 to March 2016 were extracted from the Japanese national inpatient database. Outcome measures were all-cause in-hospital death, stroke, acute kidney injury and tracheotomy, and composite adverse events (consisting of all-cause in-hospital death, stroke, acute kidney injury, and tracheotomy), and we compared them between surgical and conservative treatments using propensity score matching.
Results
The study cohort included 3258 patients, with 845 matched pairs (1690 patients) in the propensity score matching. All-cause in-hospital death was significantly lower in the surgical treatment group than in the conservative treatment group before and after matching (15.6% vs. 51.1%, p < 0.001; 16.7% vs. 31.6%, p < 0.001, respectively); however, there was no significant difference in composite adverse events after matching (36.0%, conservative vs. 37.2%, surgical; p = 0.65), and adjusted odds ratio was 1.06 and 95% confidence interval was 0.86–1.29 (p = 0.61) with reference to conservative treatment.
Conclusions
All-cause in-hospital death among elderly patients with AAD was significantly lower in patients treated surgically than in those undergoing conservative treatment. However, there was no significant difference between the two groups in the event-free survival, which is important for the elderly. These findings may be used in the consideration of treatment course for elderly patients with AAD.
Similar content being viewed by others
Background
The ageing of populations is presenting new challenges to developed countries worldwide. In 2015, 26.7% of the Japanese population was over 65 years of age, and 8.0% of the population was over 80. The fraction of the Japanese population aged 80 or older is estimated to reach 10% by 2025 [1]. The opportunity for elderly patients with fatal diseases to be transported is increasing, and type A aortic dissection (AAD) is no exception. However, whether emergency surgical intervention should be performed in elderly patients is controversial because of the high postoperative mortality and complication rates associated with the extreme invasiveness of this procedure, and age of ≥80 years is a significant risk factor associated with postoperative short-term mortality rate [2,3,4,5,6]. As previously reported by Hata et al. [4], surgery may not necessarily lead to a good outcome for patients and their family, as the elderly may become bedridden or depressed after surgery. However, because AAD has a high mortality rate (42.9–63.6%) without surgery [7,8,9,10,11], whether surgery should be performed for an elderly patient is an ethically difficult decision for surgeons. Clarifying the difference between the outcomes including mortality as well as complications and physical functions of conservative and surgical management of AAD in the elderly may help in therapeutic decision making in patients with AAD admitted to the emergency room.
Although retrospective cohort studies have compared conservative and surgical management of AAD, the patient cohorts of these studies were not adjusted for background. Thus, many inoperable patients with severe conditions may have been included in the non-surgical treatment group, making comparison of the two groups by randomization difficult. Therefore, this study compares the conservative and surgical management of patients with AAD aged > 80 years after adjusting for severity by propensity scores using data from the national inpatient database in Japan.
Methods
Data collection
We performed a retrospective cohort study using the Japanese Diagnosis Procedure Combination (DPC) database. The DPC system was introduced in Japan in 2003 as a comprehensive daily evaluation system for acute-phase hospital medical care. In 2016, DPC-participating hospitals accounted for approximately 80% of acute-phase beds in Japan. Clinical information and other data for patients were registered in the DPC database and classified by a 14-digit DPC code. The system holds the following clinical information: patient demographics, diagnoses, comorbidities and complications [registered using the International Classification of Disease, 10th revision (ICD10)], drugs and devices used, procedures performed, healthcare costs and status at admission and discharge.
Patient selection
Data were extracted from the DPC database between April 2014 and March 2016. First, we identified patients aged 80 years or older with acute aortic dissection (ICD10 code, I71.0) recorded as either the “main diagnosis,” “admission-precipitating diagnosis,” or “most resource-consuming diagnosis” and identified patients with dissection in the ascending aorta with “Stanford type A,” “DeBakey I,” or “DeBakey II” as the disease name. We excluded patients who had planned admission and unknown admission pathway. The final cohort was divided into the conservative and surgical treatment groups.
Variables and outcomes
We matched propensity scores between the surgical and conservative treatment groups. Propensity scores were calculated using a logistic regression model with the following variables: age, sex, body mass index (divided into the four following groups: < 18.5, 18.5–25.0, > 25.0, and data missing), admission pathway (home, other hospital, or clinic and nursing-care facility), ambulance use, hypertension, diabetes mellitus, chronic obstructive pulmonary disease (COPD), chronic kidney disease, ischemic heart disease, chronic liver disease, cancer, dementia, cardiopulmonary arrest, cardiac tamponade, shock, coronary malperfusion, limb ischemia, aortic insufficiency, hospital volume [low (< 10 cases), middle (10–20 cases), and high (>20cases)] and consciousness level upon admission (Japan coma scale: 0, alert; 1–3, delirious; 10–30, somnolent and 100–300, coma). Outcome measures were all-cause in-hospital death, stroke, and acute kidney injury (AKI) requiring renal replacement therapy (RRT), tracheotomy, composite adverse events (all-cause in-hospital death, stroke, AKI, and tracheotomy), length of hospital stay, length of intensive care unit (ICU) stay, inpatient costs, home discharge rate, and activities of daily living (ADL) of surviving patients at discharge. ADL was evaluated using the Barthel index (BI), which assesses the ADL using a 100-point scale comprising the following 10 items: “Bowels,” “Bladder,” “Grooming,” “Toilet use,” “Feeding,” “Transfer,” “Mobility,” “Dressing,” “Stairs,” and “Bathing,” and we set the BI cut-off at 60 points, which indicates having functional dependency. [12, 13].
Statistical analysis
Summary statistics are presented as frequencies and percentages for categorical variables and median and interquartile ranges for continuous variables (with non-normal distribution in the Shapiro–Wilk test). Data were compared using the Mann–Whitney U test for continuous variables and the chi-squared test for categorical variables before matching; after matching, the Wilcoxon signed rank and McNemar tests were performed. We performed one-to-one pair matching using nearest neighbor matching without replacement within 0.2 standard deviations of the logit of the propensity score as caliper width [12]. Covariate balance between the two groups was checked depending on whether the absolute standardized difference was < 10% [13]. Adjusted odds ratios (AOR) for the primary outcome were estimated using multivariable logistic regression in all patients aged > 80 years to investigate the influence of the type of surgery. As a subgroup analysis, the status of surviving patients at discharge in both the groups was compared before after matching. The robustness of the result was confirmed using the following method as sensitivity analysis for the BMI missing value (749 cases): list-wise deletion method (excluded the BMI missing data), median imputation for BMI missing data and multiple imputation for BMI missing data. All analyses were performed using the R statistical software (version 3.5.1; R Foundation for Statistical Computing, Vienna, Austria), and the packages used for analyses were “Matching” for propensity score matching and “mice” for missing value complement. P < 0.05 was considered significant, and hypothesis tests were two sided. This study was performed with the approval of the Ethics Committee, Kyoto University Graduate School and Faculty of Medicine (Approval number: R0135).
Results
The process used to select eligible patients is shown in Fig. 1. The total patient cohort included 3258 patients (surgical treatment group, n = 1241; conservative treatment group, n = 2017) who were hospitalized in a total of 634 hospitals. The study had 845 matched pairs (1690 patients) in the propensity score matching. As shown in Fig. 2, the fraction of patients treated conservatively increased with increasing age, with a steep increase for patients over 80 years of age. Patient background and clinical findings before and after matching are compared in Table 1. Before matching, the age of the conservative treatment group was significantly higher than that of the surgical treatment group [86.0 years (82.0–89.0) vs. 83.0 years (81.0–86.0), respectively]. The rate of patients transferred from other hospitals was significantly higher for the surgical treatment group, whereas that of patients from nursing-care facilities was significantly higher for the conservative treatment group. Dementia was frequently observed in the conservative treatment group (9.5% vs. 6.4%). The surgical treatment group had considerably more patients with a good level of consciousness upon admission. The rate of cardiopulmonary arrest was also higher in the conservative treatment group (10.0% vs. 0.4%), whereas shock and aortic insufficiency were higher in the surgical treatment group. Surgical management was often selected in high volume hospitals. All baseline characteristics between the groups after matching remained balanced, with the absolute standardized effect size < 10%.
Outcomes are shown in Tables 2 and 3. All-cause in-hospital death was higher in the conservative treatment group even after matching (31.6% vs. 16.7%) (AOR, 0.42; 95% CI, 0.33–0.54; p < 0.001), but complications and tracheotomy during hospitalization were high in the surgical treatment group both before and after matching: stroke (3.5% vs. 17.2%)/(4.5% vs. 17.5%), acute kidney injury (1.0% vs. 8.8%)/(1.7% vs. 8.6%), and tracheostomy (0.8% vs. 8.7%)/(1.1% vs. 9.2%). Composite adverse events occurred in 54.0 and 36.6% in conservative and surgical treatment groups, respectively, before matching but occurred in 36.0 and 37.2%, respectively, after matching, which was not significant.
The hospital length of stay and ICU length of stay were significantly longer in the surgical treatment group before/after matching, although the difference was lower after matching. The medical expenses were also significantly higher in the surgical treatment group than in the conservative treatment group before/after matching [$4100 (1400–10,200) vs. $36,600 (30,300–45,400); p < 0.001]/[$7200 (2700–12,100) vs. $36,400 (30,300–45,900); p < 0.001].
The results of functional status at discharge of surviving patients are shown in Table 4. The home discharge rate was significantly higher for the conservative treatment group both before and after matching (52.8% vs. 42.8%). BI score was significantly higher and patients whose BI was < 60 points was significantly lower in the surgical treatment group, but these differences became insignificant after matching.
The AOR for postoperative outcomes by each type of surgeries is shown in Table 5. As the procedure of the surgery became more complicated, AOR for all-cause in-hospital death and composite events tended to increase. The AOR for postoperative complications and tracheotomy was the highest in the total arch replacement.
Multiple sensitivity analyses about missing data showed similar point estimates and 95% CIs (See Additional file 1).
Discussion
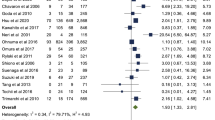
Advances in minimally invasive surgery and the advent of aortic aneurysm stent grafts and transcatheter aortic valve implantation provide more treatment options for previously difficult-to-treat cardiovascular conditions in high-risk or elderly patients. In contrast, although there are some reports of endovascular treatment for AAD [14, 15], it still requires surgery involving sternotomy and cardiopulmonary bypass under hypothermia. Because such treatment imposes a tremendous burden on elderly patients, the establishment of AAD treatment standards for elderly patients has been controversial. However, the surgical outcomes of these patients are improving because of advancements in surgical techniques, cardiopulmonary bypass and postoperative management. Recent reports of AAD surgery in elderly patients are positive [16,17,18]. In a meta-analysis of elderly patients with AAD (> 80 years of age), Biancari et al. compared immediate postoperative mortality among patients treated surgically and those treated with conservative therapy using Pool analysis of data reported in two previous studies [13]. Although this study cohort was small, their analysis indicates more favorable outcomes for patients treated surgically (postoperative mortality rate: surgical treatment, 25.2%; non-surgical treatment, 59.0%). Furthermore, postoperative mortality of AAD surgery in the elderly in some reports from Japan is generally low (3.7–13.6%) and favorable, although their age definition of ‘elderly’ varies from 70 to 80 years of age [16,17,18,19,20,21,22]. Despite these favorable reports, our survey indicates that only half of the elderly patients with AAD (80 years or older) are treated surgically.
We observed a lower in-hospital mortality rate in patients undergoing surgery than in those receiving conservative treatment (15.6% /16.7%; before/after matching), the risk difference was 14.9% even after matching. These results certainly indicate that surgery is a good treatment option; however, on the other hand, the percentage of patients who could be discharged to home after surgery was approximately 40, and 40% of the patients in the surgical treatment group had BI < 60 and required a lot of assistance. These results support the observation by Hata et al. that AAD surgery poses issues including the risk of being bedridden and/or depressed and a burden on the family [3]. In addition, stroke, acute kidney injury and tracheostomy during hospitalization were significantly higher in the surgical treatment group than in the conservative treatment group, so there was no significant difference in the primary outcome after matching between the groups. Once these complications and events occur in the elderly, there is a high possibility that irreversible function decline will occur in them than in younger patients. Further, the hospital length of stay, ICU length of stay and inpatient costs were higher in the surgical treatment group. However there was no difference in the functional status between the two groups, that is, low-grade stroke or AKI do not necessarily lead to functional decline. These results make it difficult for the elderly with AAD to select a treatment option (Fig. 2).
Extremely positive outcomes have been reported for elderly patients undergoing hemiarch replacement and a short-time/less-invasive ascending aortic replacement for entry closure [16, 21], and favorable outcomes with a good QOL assessment after AAD surgery have been reported for elderly patients with use of 36-Item Short Form Health Survey (SF36) [23, 24]. Our results also show favorable results with ascending aortic or hemiarch replacement. Conversely, Ozaki and colleagues recently proposed medical treatment as an option for AAD, reporting good results with medical treatment for AAD in a small cohort of elderly patients [25]. Our results also show favorable results with ascending aortic or hemiarch replacement, but complex procedures such as root surgery may be worse than conservative therapy.
Few reports have compared conservative and surgical treatment of the elderly, and the results of this study may be useful for choosing treatment plans in patients with AAD. The strengths of this study are that we examined an unprecedented number of AAD cases in the elderly and are the first to compare surgical and conservative treatments using propensity scores and that we compared short-term mortality as well as event-free survival rate and functional status at discharge, which is particularly important in the elderly. However, this study also has some limitations. Because the study cohort includes a very specific population over 80 years of age, the results cannot be extrapolated to different populations. The retrospective design of this study has inherent limitations, especially selection bias and dependence on historical records. Other limitations include a lack of clinical information, including preoperative vital signs, laboratory data/diagnostic imaging, specific anaesthesia method/surgical technique, and postoperative management. Other underlying diseases may not have been identified because of the extraction of comorbidity or findings on admission from registered disease names. Propensity scores may have been influenced by the presence of unmeasured factors. Because our study was short term, the results do not reflect subsequent death after discharge or the later need for surgery. Thus, our results do not address the mid- or long-term outcomes after discharge.
Conclusions
Our results indicate that AAD surgery is a feasible treatment option for the elderly and has a significantly lower hospital mortality rate than does conservative treatment, even in patients over 80 years of age. Despite these findings, many elderly patients with AAD are not treated surgically. This may be due to postoperative complications and poor condition at discharge. With the growth of older populations in Japan and other countries worldwide, postoperative outcomes of the elderly will be an increasingly important issue, and increase in event-free survival rate will support the choice of AAD surgery for the elderly patients.
Abbreviations
- AAD:
-
Type A aortic dissection
- ADL:
-
Activities of daily living
- AKI:
-
Acute kidney injury
- AOR:
-
Adjusted odds ratio
- BI:
-
Barthel index
- COPD:
-
Chronic obstructive pulmonary disease
- DPC:
-
Diagnosis procedure combination
- ICU:
-
Intensive care unit
- RRT:
-
Renal Replacement therapy
References
Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. 2015;385:800–11.
Estrera AL, Safi HJ. Aortic dissections in the elderly ethical dilemmas of treatment. Tex Heart Inst J. 2012;39(6):831–3.
Hata M, Sezai A, Niino T, Yoda M, Unosawa S, Furukawa N, et al. Should emergency surgical intervention be performed for octogenarian with type a acute aortic dissection? J Thorac Cardiovasc Surg. 2008;135:1042–6.
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The international registry of acute aortic dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897–903.
Chan SH, Liu PY, Lin LJ, Chen JH. Predictors of in-hospital mortality in patients with acute aortic dissection. Int J Cardiol. 2005;105:267–73.
Trimarchi S, Eagle KA, Nienaber CA, Rampoldi V, Jonker FH, De Vincentiis C, et al. Role of age in acute type a aortic dissection outcome: report from the international registry of acute aortic dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140:784–9.
Dumfarth J, Peterss S, Luehr M, Etz CD, Schachner T, Kofler M, et al. Acute type A dissection in octogenarians: does emergency surgery impact in-hospital outcome or long-term survival? Eur J Cardiothorac Surg. 2017;51:472–7.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Bruno VD, Chivasso P, Guida G, Vohra HA. Surgical repair of Stanford type a aortic dissection in elderly patients: a contemporary systematic review and meta-analysis. Ann Cardiothorac Surg. 2016;5:257–64.
Kilic A, Tang R, Whitson BA, Sirak JH, Sai-Sudhakar CB, Crestanello J, et al. Outcomes in the current surgical era following operative repair of acute type a aortic dissection in the elderly: a single-institutional experience. Interact Cardiovasc Thorac Surg. 2013;17:104–9.
Malvindi PG, Modi A, Miskolczi S, Kaarne M, Barlow C, Ohri SK, et al. Acute type a aortic dissection repair in elderly patients. Eur J Cardiothorac Surg. 2015;48:664–70.
Biancari F, Vasques F, Benenati V, Juvonen T. Contemporary results after surgical repair of type a aortic dissection in patients aged 80 years and older: a systematic review and meta-analysis. Eur J Cardiothorac Surg. 2011;40:1058–6.
Horton JD, Kölbel T, Haulon S, Khoynezhad A, Green RM, Borger MA, et al. Endovascular repair of type a aortic dissection: current experience and technical considerations. Semin Thoracic Surg. 2016;28:312–7.
Sobocinski J, O’Brien N, Maurel B, Bartoli M, Goueffic Y, Sassard T, et al. Endovascular approaches to acute aortic type A dissection: a CT-based feasibility study. Eur J VascEndovasc Surg. 2011;42:442–7.
Hata M, Suzuki M, Sezai A, Niino T, Unosawa S, Furukawa N, et al. Less invasive quick replacement for octogenarians with type a acute aortic dissection. J Thorac Cardiovasc Surg. 2008;136:489–93.
Goda M, Imoto K, Suzuki S, Uchida K, Yanagi H, Yasuda S, et al. Risk analysis for hospital mortality in patients with acute type a aortic dissection. Ann Thorac Surg. 2010;90:1246–50.
Matsushita A, Tabata M, Fukui T, Sato Y, Matsuyama S, Shimokawa T, et al. Outcomes of contemporary emergency open surgery for type A acute aortic dissection in elderly patients. J Thorac Cardiovasc Surg. 2014;147:290–4.
Tanaka M, Kimura N, Yamaguchi A, Adachi H. In-hospital and long-term results of surgery for acute type A aortic dissection: 243 consecutive patients. Ann Thorac Cardiovasc Surg. 2012;18:18–23.
Komatsu K, Takano T, Terasaki T, Wada Y, Seto T, Fukui D, et al. Surgical outcomes of acute type A aortic dissection in elderly patients. Ann Thorac Surg. 2014;97:1576–81.
Suenaga E, Sato M, Fumoto H. Ascending aortic replacement for acute type A aortic dissection in octogenarians. Gen Thorac Cardiovasc Surg. 2016;64:138–43.
Kawahito K, Kimura N, Yamaguchi A, Aizawa K, Misawa Y, Adachi H. Early and late surgical outcomes of acute type A aortic dissection in octogenarians. Ann Thorac Surg. 2018;105:137–43.
Tang GH, Malekan R, Cindy JY, Kai M, Lansman SL, Spielvogel D. Surgery for acute type A aortic dissection in octogenarians is justified. J Thorac Cardiovasc Surg. 2013;145:S186–90.
Jussli-Melchers J, Panholzer B, Friedrich C, Broch O, Renner J, Schöttler J, et al. Long-term outcome and quality of life following emergency surgery for acute aortic dissection type A: a comparison between young and elderly adults. Eur J Cardiothorac Surg. 2017;51:465–71.
Ozaki N, Yuji D, Sato M, Inoue K, Wakita N. Medical treatment for acute type a aortic dissection. Interact Cardiovasc Thorac Surg. 2018;26:696–99.
Acknowledgements
Not applicable.
Funding
This study was supported by a Health and Labour Sciences Research Grant from the Ministry of Health, Labour and Welfare, Japan [Grant Number: H27-iryo-ippan-001, 2015; H28-seisaku-sitei-009, 2016] and a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science [Grant number: (A) 16H02634, 2014].
Availability of data and materials
The data availability is not applicable due to an ethical restriction. However, data will be made available by the DPC research group for researchers who meet the criteria for access to these confidential data. Requests to access the data should be submitted to the corresponding author.
Author information
Authors and Affiliations
Contributions
TA study design, data collection or management, data analysis, manuscript writing, YI study design, manuscript editing, SK data collection or management, KF data collection or management, TS study design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed with the approval of the ethics committee of Kyoto University (approval number: R0135).
Consent for publication
Not applicable.
Competing interests
All authors declared that they had no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Additional table. Sensitivity analysis for BMI missing data (DOCX 19 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Aoyama, T., Kunisawa, S., Fushimi, K. et al. Comparison of surgical and conservative treatment outcomes for type a aortic dissection in elderly patients. J Cardiothorac Surg 13, 129 (2018). https://doi.org/10.1186/s13019-018-0814-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-018-0814-6