Abstract
Background
Bochdalek hernia is a type of congenital diaphragmatic hernia that typically presents in childhood, while this diseases is extremely rare in adults.
Case presentation
We review a case of a 63-year-old man with a left-sided Bochdalek hernia who was experiencing occasional pain at the left side of his chest for 8 months. The diagnosis of Bochdalek hernia was made by chest computed tomography. A part of the retroperitoneal adipose tissue was herniated into the left thoracic cavity through the diaphragmatic defect. The hernia was treated via video-assisted thoracoscopic surgery and he made an uneventful recovery.
Conclusions
We report a rare case of a left-sided Bochdalek hernia for which our patient was treated successfully via video-assisted thoracoscopic surgery. Even though rare, this disorder should be recognised, examined and treated appropriately to avoid complications.
Similar content being viewed by others
Background
Bochdalek hernias (BH) are a congenital posterolateral diaphragmatic defect, which were first described by Bochdalek in 1848 [1]. Once diagnosed, Bochdalek hernias should be surgically treated during the neonatal period. Therefore, adult cases are rare, with a reported frequency of 0.17 to 6% among all diaphragmatic hernias [2]. Herein we present a case of a 63-year-old man whose Bochdalek hernia was successfully treated by video-assisted thoracoscopic surgery (VATS).
Case presentation
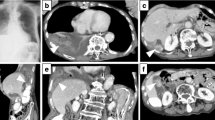
A 63-year-old man was referred to our hospital because of chest pain. He had experienced occasional pain at the left side of his chest for 8 months. During the past month the pain had become increasingly severe with no hard signs (negative physical examination). The computed tomography (CT) showed a mass in the left thoracic cavity and a left diaphragmatic defect (Fig. 1). According to computed tomography scan and such a location, the diagnosis of a Bochdalek hernia was thus suggested.
The Video-assisted thoracoscopic surgery (VATS) was performed under general anesthesia with single lung ventilation on June 30, 2015. The patient was placed in the right decubitus position, a 15 mm port was made through the 7th intercostal space on the midaxillary line, and then a 30-degree thoracoscope was inserted. Another two ports were next placed at the 5th intercostal space on the anterior axirally line and 7th intercostal space on the scapular line.
Exploratory thoracoscopy showed that a part of the retroperitoneal adipose tissue was herniated into the left thoracic cavity through the defect (Fig. 2a), 4 cm in length approximately, in the posterior region of the left diaphragm, but no hernia sac was identified. After cutting the parietal pleura enveloping the mass, clear margins of the defect of the diaphragm were revealed (Fig. 2b). The herniated tissue was moved back to the abdominal cavity, and the defect of the diaphragm was then closed with 3-0 polypropylene sutures. The postoperative course was uneventful and the patient was discharged 8 days after the operation without any symptoms. At follow-up, he remains well without any signs of recurrence 6 months after surgery.
Discussion
BH is a common congenital anomaly in neonatal and postnatal patients and occurs in about one in 2,200 to 12,500 live births, but it is rare in adults [3]. A defective closure of the lumbar and costal muscle groups in the posterolateral diaphragm during the embryonic stage is considered to be the cause of BH. This congenital diaphragmatic hernia is considered to be extremely rare in adults and have a left-sided predominance. Our patient also had left-sided hernia. Complete closure occurs on the right side before it is complete on the left side-a fact that may contribute to the left sided BH being more common than right sided hernias [4]. Most BH are found and repaired in childhood, as many as 5% are first detected in adulthood [5]. BH usually present with severe respiratory distress immediately after birth, which is life-threatening, while most adults present with more chronic symptoms, such as chronic dyspnoea, chest pain and pleural effusion. Recurrent abdominal pain, postprandial fullness and vomiting are the most common abdominal symptoms in adults [6]. Our patient was experiencing the symptoms of recurrent chest pain, while some patients have no symptoms and the disorder is unexpectedly detected on chest X-ray [7].
Diagnosis is usually made on radiological findings. The best radiological investigation in adults is CT scan which has a sensitivity of 78% for left-sided hernia and 50% for the right-sided hernia [8]. Usually, the CT scan show a mass of fat or soft tissue contour of the upper surface of the diaphragm, and a discontinuity of the diaphragm adjacent to the mass. In our case, the diaphragmatic defect could be identified clearly in the computed tomography (CT), and the diagnosis was confirmed. In contrast to Morgagni hernias, BH rarely contains a hernia sac. Only 10.4% patients (18/173) had a hernia sac [4]. Most asymptomatic Bochdalek hernias contain only retroperitoneal adipose tissue, but almost any organ of the peritoneal cavity can herniated through the foramen of Bochdalek [9].
The first successful repair of a BH was performed in 1901 by Aue [10]. The most frequent approach for the Bochdalek hernia is a thoracotomy or transabdominal, and the surgical method is to return the herniated organs to the abdominal cavity and close the diaphragmatic defect [11]. Transthoracic approach is thought to be effective as it allows for direct observation of the herniated viscera or hilium of the hernia or sac, and it is easier to remove the herniated viscera if there is some adherence [12]. With the advancement of modern surgical techniques, less invasive means of repair are available. The VATS is generally considered to be advantageous over standard thoracotomy because it is less invasive, reduced postoperative pain, and allows the surgeon to make more precise incisions. The diaphragmatic defects sometimes do not have sufficient margin for reapproximation directly. Several surgeons reported using artificial material for closing large defect [13, 14]. In our case, the diaphragmatic defect was small (3 cm × 4 cm in size), so we perform primary closure of the diaphragmatic defect by thoracoscopic surgery alone, and we didn’t apply a mesh to reinforce the diaphragm.
Conclusion
We report a rare case of a left-sided Bochdalek hernia in an adult who was treated via VATS. People with a Bochdalek hernia may not have any symptoms and the disorder may be detected unexpectedly, or the symptoms and expressions may vary from mild to serious complications. Even though rare, this disorder should be recognised, examined and treated appropriately to avoid complications.
Abbreviations
- BH:
-
Bochdalek hernia
- CT:
-
Computed tomography
- VATS:
-
Video-assisted thoracoscopic surgery
References
Novakov IP, Paskalev G. Adult Bochdalek hernia simulating left pleural effusion: a review and a case report. Folia Med (Plovdiv). 2010;52(4):62–6.
Tokumoto N, Tanabe K, Yamamoto H, et al. Thoracoscopic-assisted repair of a bochdalek hernia in an adult: a case report. J Med Case Rep. 2010;4:366.
Laaksonen E, Silvasti S, Hakala T. Right-sided Bochdalek hernia in an adult: a case report. J Med Case Rep. 2009;3:9291.
Brown SR, Horton JD, Trivette E, et al. Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia. 2011;15(1):23–30.
Langham Jr MR, Kays DW, Ledbetter DJ, et al. Congenital diaphragmatic hernia. Epidemiology and outcome. Clin Perinatol. 1996;23(4):671–88.
Kanazawa A, Yoshioka Y, Inoi O, et al. Acute respiratory failure caused by an incarcerated right-sided adult bochdalek hernia: report of a case. Surg Today. 2002;32(9):812–5.
Niwa T, Nakamura A, Kato T, et al. An adult case of Bochdalek hernia complicated with hemothorax. Respiration. 2003;70(6):644–6.
Husain M, Hajini FF, Ganguly P, et al. Laparoscopic repair of adult Bochdalek’s hernia. BMJ Case Rep. 2013;2013. doi:10.1136/bcr-2013-009131.
Wilbur AC, Gorodetsky A, Hibbeln JF. Imaging findings of adult Bochdalek hernias. Clin Imaging. 1994;18(3):224–9.
Abdullah M. Congenital diaphragmatic hernia in a post-partum woman. Med J Malaysia. 2003;58(1):99–101.
Mousa A, Sanusi M, Lowery RC, et al. Hand-assisted thoracoscopic repair of a Bochdalek hernia in an adult. J Laparoendosc Adv Surg Tech A. 2006;16(1):54–8.
Brusciano L, Izzo G, Maffettone V, et al. Laparoscopic treatment of Bochdalek hernia without the use of a mesh. Surg Endosc. 2003;17(9):1497–8.
Nguyen TL, Le AD. Thoracoscopic repair for congenital diaphragmatic hernia: lessons from 45 cases. J Pediatr Surg. 2006;41(10):1713–5.
Ambrogi V, Forcella D, Gatti A, et al. Transthoracic repair of Morgagni’s hernia: a 20-year experience from open to video-assisted approach. Surg Endosc. 2007;21(4):587–91.
Acknowledgements
Not applicable.
Funding
No funding.
Availability of data and materials
The data supporting the conclusions of this article are included within the article.
Authors’ contributions
All authors participated in the design of the case report and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
Not required.
Disclosures
The authors have no funding, financial relationships or conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Shen, YG., Jiao, NN., Xiong, W. et al. Video-assisted thoracoscopic surgery for adult Bochdalek hernia: a case report. J Cardiothorac Surg 11, 165 (2016). https://doi.org/10.1186/s13019-016-0558-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-016-0558-0





