Abstract
Degenerative disc disease is the leading cause of lower back and leg pain, considerably impacting daily life and incurring substantial medical expenses for those affected. The development of annulus fibrosus tissue engineering offers hope for treating this condition. However, the current annulus fibrosus tissue engineering scaffolds fail to accurately mimic the natural biological environment of the annulus fibrosus, resulting in limited secretion of extracellular matrix produced by the seeded cells and poor biomechanical properties of the constructed biomimetic annulus fibrosus tissue. This inability to match the biomechanical performance of the natural annulus fibrosus hinders the successful treatment of annulus fibrosus defects. In this study, we fabricated decellularized annulus fibrosus matrix (DAFM)/chitosan hydrogel-1 (DAFM: Chitosan 6:2) and DAFM/chitosan hydrogel-2 (DAFM: Chitosan 4:4) by varying the ratio of DAFM to chitosan. Rat annulus fibrosus (AF)-derived stem cells were cultured on these hydrogel scaffolds, and the cell morphology, AF-related gene expression, and Interleukin-6 (IL-6) levels were investigated. Additionally, magnetic resonance imaging, Hematoxylin and eosin staining, and Safranine and Fast Green staining were performed to evaluate the repair effect of the DAFM/chitosan hydrogels in vivo. The gene expression results showed that the expression of Collagen type I (Col-I), Collagen type I (Col-II), and aggrecan by annulus fibrosus stem cells (AFSCs) cultured on the DAFM/chitosan-1 hydrogel was higher compared with the DAFM/chitosan-2 hydrogel. Conversely, the expression of metalloproteinase-9 (MMP-9) and IL-6 was lower on the DAFM/chitosan-1 hydrogel compared with the DAFM/chitosan-2 hydrogel. In vivo, both the DAFM/chitosan-1 and DAFM/chitosan-2 hydrogels could partially repair large defects of the annulus fibrosus in rat tail vertebrae. In conclusion, the DAFM/chitosan-1 hydrogel could be regarded as a candidate scaffold material for the repair of annulus fibrosus defects, offering the potential for improved treatment outcomes.
Similar content being viewed by others
Introduction
Lumbar disc herniation is a prevalent spinal disorder and one of the main causes of lower back and leg pain, leading to considerable implications for global health and socio-economic progress [1, 2]. There are various treatment options available for lumbar disc herniation, which can be broadly categorized into conservative treatment and surgical intervention. Conservative treatment methods include bed rest, physical therapy, and medication therapy. However, in cases where conservative treatment fails or when there is a progressive deterioration of neurological symptoms, surgical intervention is often necessary [3, 4]. Endoscopic discectomy has gained increasing popularity in clinical practice because it involves minimal trauma, quick recovery, and short hospital stays [5,6,7]. Nevertheless, endoscopic removal of the nucleus pulposus can potentially lead to further intervertebral disc degeneration, and improper postoperative activity may result in the recurrence of herniation caused by ruptures in the annulus fibrosus [8]. The annulus fibrosus, being a relatively enclosed avascular tissue, has limited self-healing capabilities [9, 10]. The annulus fibrosus encapsulates the nucleus pulposus, and is rich in collagen type I, imparting elasticity and resistance to lateral expansion, as well as withstanding axial loads and various stresses of the spine. It serves as the principal load-bearing tissue of the intervertebral disc and plays a crucial role in maintaining the initial morphology and position of the nucleus pulposus and sustaining physiological pressure within the disc [11]. Currently, an annulus fibrosus suture method is commonly used to treat defects. Although direct suturing of the annulus fibrosus can reduce the recurrence rates, the repaired annulus fibrosus is only mechanically closed and the physiological structure is not restored [12, 13]. Thus, the mechanical characteristics of the annulus fibrosus under pressure are not fully restored to the original physiological state. Therefore, fully repair of annulus fibrosus defects cannot be achieved solely through straightforward annulus fibrosus suturing [14]. Consequently, there is a high demand for tissue-scaffold-based strategies to repair and regenerate annulus fibrosus tissue, and tissue engineering has emerged as a new method for annulus fibrosus repair in recent years [15, 16]. The tissue engineering scaffold is a vital component of annulus fibrosus tissue engineering, primarily providing a suitable environment for cell survival and proliferation [17, 18].
Of the various available biomaterials, hydrogels have considerable value for annulus fibrosus repair because of the highly customizability and mechanical adjustability [19, 20]. Currently, gel materials are often crosslinked with other composite materials to improve the performance. Numerous studies have demonstrated that the use of decellularized matrix can eliminate immunogenicity, while preserving the majority of the remaining functional constituents of cells, such as cytokines and the micro/nanostructure of the native tissue [21]. Chitosan exhibits excellent biodegradability, biocompatibility, and antimicrobial properties, which is rich in hydroxyl and amino groups, exhibits excellent water absorption properties, making it an ideal material for preparing hydrogels [22, 23]. Additionally, chitosan shares an extremely similar molecular structure with glycosaminoglycans, which is a constituent of the native annulus fibrosus tissue [24]. Therefore, chitosan could be regarded as a kind of scaffold for annulus fibrosus tissue engineering. Genipin has been widely used in articular cartilage and intervertebral disc tissue engineering research because of its low cytotoxicity and good biological stability [25, 26].
Insufficient extracellular matrix secretion of the annulus fibrosus secreted by the seeded cells is one of the main reasons for the failure of tissue engineering in the treatment of annulus fibrosus defects. Therefore, different cell growth factors have been grafted into scaffolds to provide specific growth and differentiation signals to promote targeted cell differentiation [27, 28]. In a previous study, we used a genipin crosslinked decellularized AF matrix (DAFM)/chitosan hydrogel scaffold with basic fibroblast growth factor (bFGF), which combined the advantages of DAFM and chitosan. The bFGF can be incorporated as a sustained-release formulation [29]. However, there are limited reports on the use of scaffolds loaded with growth factors for annulus fibrosus defect repair in vivo [30], with results available only up to 8 weeks of release [31]. Annulus fibrosus defect repair is a lengthy process and while bioactive factors have potential application in the treatment of early annulus fibrosus injuries, the short half-life of bioactive factors may mean that an insufficient amount of extracellular matrix is deposited before the bioactive factors are degraded. Therefore, relying solely on the use of growth factor-loaded scaffolds to enhance extracellular matrix secretion by fibrochondrocytes is not feasible [32]. Therefore, we investigated whether adjusting the ratio of DAFM to chitosan could provide a suitable hybrid hydrogel that would promote the secretion of extracellular matrix in the annulus fibrosus without the need for the addition of growth factors.
Herein, we designed two types of hybrid hydrogels using different ratios of DAFM to chitosan. Atomic force microscopy (AFM) and scanning electron microscopy (SEM) were used to observe the surface and internal structures of these hydrogels. Rat annulus fibrosus stem cells (AFSCs) were implanted into the hybrid hydrogels to investigate the cell proliferation and extracellular matrix secretion of the annulus fibrosus from AFSCs. Additionally, the hybrid hydrogels were implanted into defects of the annulus fibrosus in the rat caudal vertebrae. The repair effect of annulus fibrosus defects was assessed using magnetic resonance imaging (MRI), Hematoxylin and eosin (HE) staining, and Safranine and Fast Green staining.
Materials and methods
Fabrication of the DAFM/chitosan hybrid hydrogels
All animal procedures were approved by the Institutional Review Board of Yijishan Hospital of Wannan Medical College (Wuhu, China). Decellularized annulus fibrosus matrix (DAFM) was prepared following the protocol as the previous study reported [33]. A chitosan solution was prepared by dissolving 1.5 g of chitosan powder in 100 mL of 3% acetic acid. A genipin solution was obtained by dissolving 0.1 g of genipin powder in 10 mL of 75% ethanol. Two types of DAFM/chitosan hybrid hydrogels were prepared as follows: DAFM/chitosan 6:2 hydrogel (DAFM/chitosan-1) was prepared by mixing 6 mL of DAFM solution, 2 mL of chitosan solution, and 1 mL of 1% genipin solution by stirring; DAFM/chitosan 4:4 hydrogel (DAFM/chitosan-2) was prepared by mixing 4 mL of DAFM solution, 4 mL of chitosan solution, and 1 mL of 1% genipin solution by stirring.
Atomic force microscopy
A portion of the prepared DAFM/chitosan hybrid hydrogel was cut off, PBS was added, and the hybrid hydrogels were kept moist before being placed under an atomic force microscope to observe the surface microstructure of both types of the DAFM/chitosan hybrid hydrogels.
Morphological characterization of DAFM/chitosan hybrid hydrogels
For SEM analysis, the two types of hybrid hydrogels were shock-frozen in liquid nitrogen and immediately transferred to a freeze dryer for lyophilization. The dry hybrid hydrogel surfaces were then coated with a thin layer of gold and measured using a Hitachi JSM-840 microscope.
Cell morphology observations
300 µl of DAFM/chitosan-1 hybrid hydrogel solution and DAFM/chitosan-2 hybrid hydrogel solution was added per well in each of six wells of the 24-well plate, respectively. And the hybrid hydrogels were formed after 24 h at room temperature. Following 60Co irradiation sterilization, 2000 rat AFSCs were seeded onto the two types of hybrid hydrogels. After culturing for 3 days, cytoskeleton staining was performed. FITC-phalloidin solution (200 µl) at a concentration of 5 µg/mL was added to each well and the wells were incubated in the dark for 5 min. The AFSC-hybrid hydrogel complexes were then washed three times in PBS with agitation on a shaker for 5 min each time. After removing the PBS solution, 200 µl of DAPI solution at a concentration of 5 µg/mL was added to each well to stain the cell nuclei and the wells were incubated in the dark for 5 min. The AFSC-hybrid hydrogel complexes were then washed three times in PBS with agitation on a shaker for 5 min each time. The morphology of the AFSCs on the hybrid hydrogels was observed using inverted immunofluorescence microscopy. After being cultured for 3 days, the cell morphology was also examined by SEM analysis. Rat AFSCs on the hybrid hydrogels were rinsed with PBS twice, fixed with 2.5% glutaraldehyde for 2 h, and then rinsed with deionized water three times. The cell-hybrid hydrogel complexes were dehydrated using a series of ethanol concentrations (50%, 60%, 70%, 80%, 90%, 95%, and 100%) for 10 min each time. The dried samples were subsequently sputter-coated with gold and visualized by SEM using an accelerating voltage of 3 kV.
AF-related gene expression analysis
Aliquots of the hybrid hydrogel liquid (3 ml) were placed in a 6-well culture plate, and the hybrid hydrogels were formed after 24 h at room temperature. After 60Co irradiation sterilization, 1 × 104 rat AFSCs were planted on the hydrogel. After being cultured for one week, RT-qPCR was conducted to analyze the expression of annulus fibrosus-related genes, including Col-I, Col-II, and aggrecan; and MMP-9 and inflammatory mediators, including IL-6. RNA extraction utilized TRIzol reagent (Invitrogen, USA), with subsequent reverse transcription using the a Revert-Aid™ First-Strand cDNA Synthesis Kit (K1622; Fermentas, Lithuania) and oligo (dT) primers according to the manufacturer’s instructions. RT-qPCR were performed using the Bio-Rad CFX96™ Real-Time System (Roche, Switzerland) to assess the expression of the above genes. The primer sequences for Col-I, Col-II, aggrecan, MMP-9, IL-6, and GAPDH are provided in Table 1. The relative expression levels of these genes were calculated using the 2−∆∆Ct method and normalized to GAPDH, which served as an internal control. Each sample was analyzed in triplicate.
Animal study
Sixteen Sprague-Dawley rats were divided into four groups, with four rats in each group. The first group was the DAFM/chitosan-1 hybrid hydrogel group. The second group was the DAFM/chitosan-2 hybrid hydrogel group. The third group was the control group, which had annulus fibrosus defects. The fourth group was the sham group, which did not receive any treatment. The specific procedure was as follows: 1% pentobarbital sodium was administered intraperitoneally to anesthetize the rats at a dose of 0.08 mL of 1% pentobarbital sodium solution per 20 g of body weight. The rats were placed in a prone position, and the tail vertebrae of the rats were disinfected and draped. A 1-cm incision was made on the dorsal side of the tail vertebrae at the end of the trunk. All animal experiments were conducted by the same skilled spinal surgeon to ensure uniformity in defect creation. The posterior part of the tail vertebrae was exposed layer by layer, and a 2 mm×2 mm square section of the annulus fibrosus was removed under microscopic guidance using microsurgical instruments. In the annulus fibrosus defect group, the wound was sutured layer by layer after partial removal of the annulus fibrosus. In the experimental groups, Then DAFM/chitosan-1 hybrid hydrogel and DAFM/chitosan-2 hybrid hydrogel with a size of about 2 mm×2 mm with square shape were implanted into the AF defect. After implantation, the surrounding tendons and muscles were sutured with 5 − 0 absorbable suture to assist in retaining the hydrogel within the defect site. After the surgery, the incision was sutured layer by layer, and the surgical site was washed with diluted iodine. Penicillin was injected into the buttocks of the SD rats twice a day for three consecutive days, at a dosage of 80,000 U of penicillin each time. The rats were free to move, eat, and drink in cages.
Magnetic resonance imaging
At 12 weeks after surgery, magnetic resonance imaging was performed to evaluate the structural changes in targeted intervertebral discs (PharmaScan 7.0 T, Bruker, Germany). T2-weighted sections in the sagittal plane were obtained using the following settings: Fast spin echo sequence with time to repetition of 2500 ms and time to echo of 33 ms, percent phase field of view of 260. The section thickness was 1 mm with a 0-mm gap.
Histology analysis
Rat tail samples were collected and fixed using 10% formalin. Following decalcification and dehydration, the samples were embedded in paraffin. Paraffin sections were stained with HE staining and Safranine and Fast Green staining according to the manufacturer’s instructions.
Statistical analysis
The results were reported as mean ± standard deviation (SD), and significance was defined as p < 0.05. Statistical comparisons of RT-qPCR between the two groups were assessed using student t-test. Statistical analyses were conducted using IBM SPSS software version 19.0. Graphical representations of the data were generated using GraphPad Prism 5 software (GraphPad Software Inc., San Diego, CA).
Results
Characterization of DAFM/chitosan hybrid hydrogels
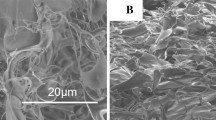
The surfaces of both types of the DAFM/chitosan hybrid hydrogels demonstrated clear collagen fiber distribution when observed using AFM. Notably, the DAFM/chitosan-1 hybrid hydrogel exhibited a higher concentration of collagen fibers than the DAFM/chitosan-2 hybrid hydrogel (Fig. 1A, B). The SEM image showed that both types of DAFM/chitosan hybrid hydrogels had a three-dimensional porous structure, although the pore density in the DAFM/chitosan-1 hybrid hydrogel was greater compared with the DAFM/chitosan-2 hybrid hydrogel (Fig. 2A-D). Additionally, interconnected micropores were observed on the surfaces of both types of the DAFM/chitosan hybrid hydrogels, indicating an increased facility for nutrient and metabolic exchange.
Cell morphology on the hydrogels
The cytoskeleton staining (Fig. 3A-F) and SEM images (Fig. 4A-B) indicated that the rat AFSCs exhibited excellent spreading characteristics on both the DAFM/chitosan-1 and DAFM/chitosan-2 hybrid hydrogels. Notably, it was observed that the rat AFSCs displayed a higher proliferation rate on the DAFM/chitosan-1 hybrid hydrogel compared with the DAFM/chitosan-2 hybrid hydrogel through cytoskeleton staining results.
Gene expression
The level of expression of the AF-related metabolic genes col-I, col-II, and aggrecan at 1 week after culture was twice as high in the DAFM/chitosan-1 hybrid hydrogel compared with the DAFM/chitosan-2 hybrid hydrogel (Fig. 5A-C). However, the level of expression of the AF-related catabolic gene, MMP-9, was twice as high in the DAFM/chitosan-2 hybrid hydrogel compared with the DAFM/chitosan-1 hybrid hydrogel (Fig. 5D). The level of expression of the inflammatory factor gene, IL-6, was 1.5 times higher in the DAFM/chitosan-2 hybrid hydrogel compared with the DAFM/chitosan-1 hybrid hydrogel (Fig. 5F). The differences were found to be statistically significant (p < 0.05) for the expression of all five genes.
After 1 week of culture, the expression of Col-I (A), Col-II (B) and aggrecan (C) by AFSCs cultured on DAFM/chitosan-1 hydrogel was higher compared with on the DAFM/chitosan-2 hydrogel. In contrast, the expression of MMP-9 (D) and IL-6 (E) was lower on DAFM/chitosan-1 hydrogel compared with on DAFM/chitosan-2 hydrogel (n = 3). *p < 0.05
MRI
The 12-week postoperative MRI sagittal T2-weighted images showed a mild reduction in the intervertebral disc height in both the DAFM/chitosan-1 hybrid hydrogel and the DAFM/chitosan-2 hybrid hydrogel groups, with the disc signal not completely turning dark. Conversely, the annulus fibrosus defect group exhibited notable intervertebral disc degeneration accompanied by a loss in disc height. In contrast, the sham group displayed normal intervertebral disc height and signal intensity (Fig. 6A-D). These results indicated that the DAFM/chitosan-1 hybrid and DAFM/chitosan-2 hybrid hydrogels had a partially repair effect on annulus fibrosus defects.
At 12 weeks post-surgery, magnetic resonance imaging revealed a slight decrease in intervertebral disc height in both the DAFM/chitosan-1 hybrid hydrogel (A) and DAFM/chitosan-2 hybrid hydrogel (B) groups. However, the AF defect group (C) exhibited a loss of intervertebral height and noticeable changes in intervertebral disc signal. The intervertebral height and intervertebral disc signal remained normal in the sham group (D)
Histology evaluation
HE staining and Safranine and Fast Green staining were employed to assess the repair of the annulus fibrosus defects. The macroscopic view of rat caudal vertebrae is depicted in Fig. 7A-D. In the DAFM/chitosan-1 hybrid hydrogel group, partial preservation of annulus fibrosus was observed (Fig. 7E, I), while the DAFM/chitosan-2 hybrid hydrogel group showed a limited presence of annulus fibrosus structure (Fig. 7F, J). The anulus fibrosus defect group exhibited a substantial absence of distinct annulus fibrosus structure, indicating concurrent impairment of the annulus fibrosus and nucleus pulposus, leading to endplate damage (Fig. 7G, K). Beside, annulus fibrosus-resembling tissue (marked with black triangle in Fig. 7E, F, I, J) could be observed at the site of annulus fibrosus defect in DAFM/chitosan-1 hybrid hydrogel group and DAFM/chitosan-2 hybrid hydrogel group, whereas irregular scar tissue (marked with black triangle in Fig. 7G, K) was visible at the site of annulus fibrosus defect in the annulus fibrosus defect group. In comparison, the sham group displayed an intact annulus fibrosus enveloping the nucleus pulposus structure (Fig. 7H, L).
Gross specimen images of DAFM/chitosan-1 hybrid hydrogel (A), DAFM/chitosan-2 hybrid hydrogel (B), the AF defect group (C), and the sham group (D) 12 weeks after surgery. HE and Fast Green-Safranin staining indicated partial preservation of the annulus fibrosus of the DAFM/chitosan-1 hybrid hydrogel (E, I) and DAFM/chitosan-2 hybrid hydrogel (F, J) groups; and H&E and Fast Green-Safranin staining indicated there was an absence of distinct annulus fibrosus structure in the control group (G, K) and an intact nucleus pulposus-annulus fibrosus structure in the sham group (H, L). Annulus fibrosus-resembling tissue (marked with black triangle) could be observed at the site of annulus fibrosus defect in DAFM/chitosan-1 hybrid hydrogel group and DAFM/chitosan-2 hybrid hydrogel group, whereas irregular scar tissue (marked with black triangle) was visible at the site of annulus fibrosus defect in the annulus fibrosus group. Scale bar: 200 μm
Discussion
In the present study, we prepared two types of DAFM/chitosan hybrid hydrogels by altering the ratio of DAFM to chitosan. Rat AFSCs were able to adhere, proliferate, and secrete annulus fibrosus-related extracellular matrix on both types of DAFM/chitosan hybrid hydrogels. In vivo experiments further demonstrated the reparative effects of both of the DAFM/chitosan hybrid hydrogels on defects in the rat tail annulus fibrosus.
The AFM images revealed the presence of collagen fibers on the surface of the hybrid hydrogels. SEM analysis revealed that both the DAFM/chitosan-1 hybrid hydrogel and the DAFM/chitosan-2 hybrid hydrogel exhibited a porous structure. Following cell implantation, the rat AFSCs were observed to grow, not only on the hydrogel surface, but also within the internal structure, facilitated by interconnected micropores that enhanced the nutrient exchange. Cell cytoskeleton staining showed that the AFSCs showed superior proliferation on the DAFM/chitosan-1 hybrid hydrogel, compared with the DAFM/chitosan-2 hybrid hydrogel, which was potentially attributable to the higher DAFM content, which was also indicated by AFM analysis. In another study, human dermal fibroblasts and human epithelial keratinocytes have been shown to be able to attach and proliferate on decellularized, dehydrated human amniotic membrane. In contrast, dehydrated human amnion/chorion membrane did not support cell attachment and proliferation under the same conditions [34]. Li et al. [35] have fabricated a decellularized matrix hydrogel using human dental pulp (hDDPM-G) and observed that surfaces coated with hDDPM-G promoted adhesion, migration, and proliferation of human dental pulp stem cells.
According to the gene expression results, AFSCs exhibited higher expression levels of annulus fibrous extracellular matrix-related metabolic genes, including Col-I, Col-II, and aggrecan genes, in DAFM/chitosan-1 hybrid hydrogels compared with the expression in DAFM/chitosan-2 hybrid hydrogels. In contrast, the expression of the degradation-related gene MMP-9 was found to be lower in DAFM/chitosan-1 hybrid hydrogels compared with DAFM/chitosan-2 hybrid hydrogels. These findings suggested that DAFM enhanced the expression of metabolic genes but suppressed the expression of a degradation-related gene associated with the annulus fibrosus extracellular matrix. Bioscaffolds originating from the decellularized extracellular matrix of tissues have the capacity to replicate the complex extracellular microenvironment by preserving the specific composition, biomechanics, and structure of the native extracellular matrix. Previous studies have demonstrated that decellularized matrix can enhance the secretion of decellularized-derived extracellular matrix. For instance, Fu et al. have developed a blood vessel matrix (BVM) hydrogel and demonstrated that coating a plate with the BVM hydrogel enhanced the tube formation of human umbilical vein endothelial cells in vitro. Furthermore, when injected into skin flaps, the BVM hydrogel improved the flap survival rate and increased blood perfusion and capillary density [36]. Bahrami et al.. [37] have created a scaffold using decellularized sheep knee cartilage for osteochondral tissue engineering. This scaffold not only facilitated EnSC osteogenic differentiation, but also induced the chondrogenic differentiation of stem cells. In vivo, acellularized scaffolds have demonstrated a good ability to support cell adhesion and proliferation, leading to improved regeneration of articular lesions in rats after 4 weeks. Huang et al. [38] have prepared human periodontal ligament cell decellularized matrix (PDLC-DCM), dental pulp cell decellularized matrix (DPC-DCM), and gingival fibroblast decellularized matrix (GF-DCM) and found that PDLC-DCM facilitated osteogenic differentiation and periodontal ligament differentiation of PDLSCs, while DPC-DCM and GF-DCM promoted osteogenic differentiation. In our previous study, we also observed increased gene expression and extracellular matrix secretion of col-I, col-II, and aggrecan in annulus fibrosus-derived stem cells cultured on DAFM/PECUU electrospun scaffolds, compared with cells cultured on PECUU fibrous scaffolds [39]. It is of interest that DAFM can downregulate the expression of MMP-9. It is widely recognized that disc degeneration is characterized by the accelerated degradation of elastin, which is caused by an increase in the expression of MMP-9 [40], MMP-9 degrades denatured collagen molecules and basement membrane collagens, which has been shown to be correlated with the lumbar intervertebral disc disease grade [41]. Kao et al. [42] have observed that the expression of the Lipocalin-2 gene and protein in rat AF cells was upregulated upon Nerve Growth Factor stimulation, resulting in increased MMP-9 activity and glycosaminoglycan release, which are likely to potentiate the degeneration of AF tissue in vivo. A similar result was found in another study in which AF cells were cultured on a plastic surface coated with fibronectin, vitronectin, col-I, gelatin, and a cell-free matrix deposited by human nucleus pulposus cells. The results showed that fibronectin, collagen, and gelatin downregulated the expression of MMP-2 and MMP-9 in the culture media [43].
The expression of IL-6, an inflammatory mediator, was lower in DAFM/chitosan-1 hydrogel than in DAFM/chitosan-2 hydrogel, indicating that DAFM could downregulate the expression of IL-6. Similar results have also been found in the study of Ahmed et al. in which an injectable hydrogel enriched with liver extracellular matrix and silver nanoparticles was developed for the treatment of acute liver failure, and significant reductions in the expression of IL-6 and transforming growth factor-beta were observed [44]. This decreased expression of pro-inflammatory factors resulted in a weaker immune response of the cells toward the material.
In the present study, we employed microsurgical instruments to generate defects in the annulus fibrosus of rat caudal vertebrae. After 3 months, MRI was conducted, which revealed that both the DAFM/chitosan hybrid hydrogel-1 and DAFM/chitosan hybrid hydrogel-2 groups had experienced some loss of intervertebral space height and darkening of disc signals, although a discernible intervertebral space was still present. The annulus fibrosus defect group exhibited a significant loss of intervertebral space height and indications of fusion. The sham group did not show any significant abnormalities in the intervertebral space height, and the disc signal remained normal. The results of HE staining and Safranine and Fast Green staining demonstrated similar findings to the MRI results. Furthermore, Safranine and Fast Green staining resulted in distinct visualization of the annulus fibrosus and nucleus pulposus tissue in the sham group, showing normal endplate morphology. The DAFM/chitosan-1 hybrid hydrogel and the DAFM/chitosan-2 hybrid hydrogel groups showed partial endplate morphology, while no obvious endplate morphology was observed in the annulus fibrosus defect group. Degeneration of the annulus fibrosus results in altered spinal stress distribution, sustained irregular stress, and aggravated intervertebral disc and spinal degeneration, ultimately leading to loss of intervertebral space height [45]. The nucleus pulposus was also hardly visible in DAFM/chitosan-1 hybrid hydrogel and the DAFM/chitosan-2 hybrid hydrogel groups. We hypothesize it was due to substantial annulus fibrosus defects and disrupted nucleus pulposus. The results of MRI, HE staining, and Safranine and Fast Green staining all demonstrated that the DAFM/chitosan hybrid hydrogels were incapable of sustaining the signal of the intervertebral disc; nevertheless, the hydrogels could partially mend defects in the annulus fibrosus, retard intervertebral disc degeneration, and forestall additional loss of intervertebral disc height. Our previous study also demonstrated that the implantation of a DAFM/PECUU blended fiber scaffold at the site of an annulus fibrosus defect in rats could partially maintain disc height in degenerated intervertebral space and potentially contributed to the reversal of disc degeneration. Studies have also demonstrated that the implantation of biomaterials can help maintain the height of degenerated intervertebral space. In a study by Li et al., the in vivo repair efficacy of hydrogels was assessed using a rat AF defect model. The findings indicated that the implantation of PEGDA/DAFM/TGF-β1 hydrogels successfully sealed the AF defect, prevented nucleus pulposus atrophy, preserved the disc height, and partially restored the biomechanical properties of the intervertebral disc [46].
There are some limitations with the present study. Annulus fibrosus is a heterogeneous tissue with considerable variations in the cell type, extracellular matrix composition, and mechanical properties along the radial regions. On the basis of the differences in mechanical properties and biochemical composition, previous studies have divided the annulus fibrosus into inner and outer regions. The radial heterogeneity of the actual annulus fibrosus was overlooked in the present study. In future studies, we will extract the inner and outer regions of the annulus fibrosus separately and prepare decellularized extracellular matrix. These matrices will be crosslinked with chitosan to create hydrogels. We will observe the proliferation of rat annulus fibrosus stem cells on these two hydrogels and monitor the secretion of extracellular matrix by annulus fibrosus stem cells. Besides, nucleus pulposus was hardly visible in hybrid hydrogel groups, we hypothesize it was due to substantial annulus fibrosus defects and disrupted nucleus pulposus. we propose utilizing a needle puncture method to induce AF defects, simultaneously with hybrid hydrogel implantation in the future study, Thus would allow for a clearer observation of nucleus pulposus and annulus fibrosus defect repair.
Conclusions
In conclusion, DAFM/chitosan-1 and DAFM/chitosan-2 hydrogels were fabricated by changing the ratio of DAFM to chitosan. Rat AFSCs tended to show higher gene expression of Col-I, Col-II, and aggrecan and lower gene expression of MMP-9 and IL-6 on the DAFM/chitosan-1 hydrogel compared with those on the DAFM/chitosan-2 hydrogel. Furthermore, an in vivo experiment indicated that the DAFM/chitosan-1 and DAFM/chitosan-2 hydrogels were able to partially repair large defects of the annulus fibrosus. Thus, the DAFM/chitosan-1 hydrogel could be regarded as a candidate scaffold for annulus fibrosus tissue engineering.
Data availability
No datasets were generated or analysed during the current study.
References
Chen KT, Wei ST, Tseng C, et al. Transforaminal endoscopic lumbar discectomy for L5-S1 disc herniatton with high iliac crest: technical note and preliminary series. Neurospine. 2020;17(Suppl 1):S81–7.
Yu P, Mao F, Chen J, et al. Characteristics and mechanisms of resorption in lumbar disc herniation. Arthritis Res Ther. 2022;23(1):205.
Bredow J, Eysel P, Oikonomidis S. Postoperative management of weight bearing and rehabilitation after lumbar spinal surgery. Orthopäde. 2020;49(3):201–10.
Baig MZ, Abdullah UEH, Muhammad A, et al. Use of platelet-rich plasma in treating low back Pain: a review of the current literature. Asian Spine J. 2021;15(1):117–26.
Jing Z, Li L, Song J. Percutaneous transforaminal endoscopic discectomy versus microendoscopic discectomy for upper lumbar disc herniation: a retrospective comparative study. Am J Transl Res. 2021;13(4):3111–9.
Sairyo K, Chikawa T, Nagamachi A. State-of-the-art transforaminal percutaneous endoscopic lumbar surgery under local anesthesia: discectomy, foraminoplasty, and ventral facetectomy. J Orthop Sci. 2018;23(2):229–36.
Pan M, Li Q, Li S, et al. Percutaneous endoscopic lumbar discectomy: indicattons and complicattons. Pain Physician. 2020;23(1):49–56.
Zhou C, Zhang G, Panchal RR, et al. Unique Complicattons of Percutaneous Endoscopic Lumbar Discectomy and percutaneous endoscopic interlaminar discectomy. Pain Physician. 2018;21(2):E105–12.
Kim JH, Ham CH, Kwon WK. Current knowledge and future therapeutic prospects in symptomatic intervertebral disc degeneration. Yonsei Med J. 2022;63(3):199–210.
Muthu S, Jeyaraman M, Chellamuthu G, et al. Does the Intradiscal Injection of Platelet Rich Plasma have any beneficial role in the management of lumbar disc disease? Global Spine J. 2022;12(3):503–14.
Ashinsky BG, Gullbrand SE, Bonnevie ED, et al. Multiscale and multimodal structure–function analysis of intervertebral disc degeneration in a rabbit model. Osteoarthr Cartil. 2019;27(12):1860–9.
Tavakoli J, Diwan AD, Tipper JL. Advanced strategies for the regeneratton of lumbar disc Annulus Fibrosus. Int J Mol Sci. 2020;21(14):4889.
Peredo AP, Gullbrand SE, Smith HE, et al. Putting the Pieces in Place: mobilizing Cellular players to improve Annulus Fibrosus Repair. Tissue Eng Part B Rev. 2021;27(4):295–312.
Roebke E, Jacho D, Eby O, et al. Injectable Cell-Laden Nanofibrous Matrix for treating Annulus Fibrosus defects in Porcine Model: an Organ Culture Study. Life (Basel). 2022;12(12):1866.
Jin XY, Kang R, Deng RR, et al. Fabrication and characterization of an acellular annulus fibrosus scaffold with aligned porous construct for tissue engineering. J Biomater Appl. 2022;36(6):985–95.
Liu C, Li Y, Zhang Y, et al. The experimental study of regeneration of annulus fibrosus using decellularized annulus fibrosus matrix/poly(ether carbonate urethane)urea-blended fibrous scaffolds with varying elastic moduli. J Biomed Mater Res A. 2022;110(5):991–1003.
Long RG, Ferguson SJ, Benneker LM, et al. Morphological and biomechanical effects of annulus ffbrosus injury and repair in an ovine cervical model. JOR Spine. 2019;21(1):e1074.
Peng Y, Huang D, Li J, et al. Genipin-crosslinked decellularized annulus fibrosus hydrogels induces tissue-speciffc differenttatton of bone mesenchymal stem cells and intervertebral disc regeneratton. J Tissue Eng Regen Med. 2020;14(3):497–509.
Sharon OB, Sigita M, Kieran M, et al. Synthesis of poly(acrylic acid)-Cysteine-based hydrogels with highly customizable Mechanical properties for Advanced Cell Culture Applications. ACS Omega. 2022;7(11):9108–17.
Xu PP, Xu HX, Yang Y, et al. A nonswellable gradient hydrogel with tunable mechanical properties. J Mater Chem B. 2020;8(13):2702–8.
Peng YZ, Chen XZ, Rao ZL, et al. Multifunctional annulus fibrosus matrix prevents disc-related pain via inhibiting neuroinflmmation and sensitization. Acta Biomater. 2023;15:170.
Deepak K, Sachin G, Manoj KS, et al. A review on the synthesis of graft copolymers of chitosan and their potential applications. Int J Biol Macromol. 2020;15:163.
Egemen A, Fatih EB, Mert G, et al. Biodegradable polymer Matrix composites containing graphene-related materials for antibacterial applications: a critical review. Acta Biomater. 2022;1:151:1–44.
Yuan DC, Chen Z, Xiang XC, et al. The establishment and biological assessment of a whole tissue-engineered intervertebral disc with PBST fibers and a chitosan hydrogel in vitro and in vivo. J Biomed Mater Res B Appl Biomater. 2019;107(7):2305–16.
Ching KY, Andriotis O, Sengers B, et al. Genipin crosslinked chitosan/PEO nanofibrous scaffolds exhibiting an improved microenvironment for the regeneration of articular cartilage. J Biomater Appl. 2021;36(3):503–16.
Panebianco CJ, Rao S, Hom WW, et al. Genipin-crosslinked fibrin seeded with oxidized alginate microbeads as a novel composite biomaterial strategy for intervertebral disc cell therapy. Biomaterials. 2022;287:121641.
Sun BB, Lian MF, Han Y, et al. A 3D-Bioprinted dual growth factor-releasing intervertebral disc scaffold induces nucleus pulposus and annulus fibrosus reconstruction. Bioact Mater. 2020;14(1):179–90.
Akyuva Y, Kaplan N, Yilmaz I, et al. Delivering growth factors through a Polymeric Scaffold to cell cultures containing both Nucleus Pulposus and Annulus Fibrosus. Turk Neurosurg. 2019;29(2):180–93.
Liu C, Jin ZX, Ge X, et al. Decellularized Annulus Fibrosus Matrix/Chitosan Hybrid Hydrogels with Basic Fibroblast Growth factor for Annulus Fibrosus tissue Engineering. Tissue Eng Part A. 2019;25(23–24):1605–13.
Guillaume O, Naqvi SM, Lennon K, et al. Enhancing cell migration in shape-memory alginate-collagen composite scaffolds: in vitro and ex vivo assessment for intervertebral disc repair. J Biomater Appl. 2015;29(9):1230–46.
Tu ZD, Han F, Zhu Z, et al. Sustained release of basic fibroblast growth factor in micro/nanofibrous scaffolds promotes annulus fibrosus regeneration. Acta Biomater. 2023;166:241–53.
Shamsah AH, Cartmell SH, Richardson SM et al. Material characterization of PCL:PLLA Electrospun fibers following six months degradation in Vitro. Polymers (Basel),2020;21;12(3):700.
Zhang J, Li B, Wang JH. The role of engineered tendon matrix in the stemness of tendon stem cells in vitro and the promotion of tendon-like tissue formation in vivo. Volume 32. Biomaterials; 2011. pp. 6972–81. 29.
Guo X, Kaplunovsky A, Zaka R, et al. Modulation of cell attachment, proliferation, and angiogenesis by decellularized, Dehydrated Human Amniotic Membrane in in vitro models. Wounds. 2017;29(1):28–38.
Li JD, Rao ZL, Zhao YM, et al. A decellularized Matrix Hydrogel Derived from Human Dental Pulp promotes Dental Pulp Stem Cell Proliferation, Migration, and Induced multidirectional differentiation in Vitro. J Endod. 2020;46(10):1438–47.
Fu W, Xu P, Feng B, et al. A hydrogel derived from acellular blood vessel extracellular matrix to promote angiogenesis. J Biomater Appl. 2019;33(10):1301–13.
Bahrami N, Bordbar S, Hasanzadeh E, et al. The effect of decellularized cartilage matrix scaffolds combined with endometrial stem cell-derived osteocytes on osteochondral tissue engineering in rats. Vitro Cell Dev Biol Anim. 2022;58(6):480–90.
Huang JP, Wu YM, Liu JM, et al. Decellularized matrix could affect the proliferation and differentiation of periodontal ligament stem cells in vitro. J Periodontal Res. 2021;56(5):929–39.
Liu C, Xiao L, Zhang Y, et al. Regeneration of annulus fibrosus tissue using a DAFM/PECUU-blended electrospun scaffold. J Biomater Sci Polym Ed. 2020;31(18):2347–61.
Loreto C, Musumeci G, Castorina A, et al. Degenerative disc disease of herniated intervertebral discs is associated with extracellular matrix remodeling, vimentin-positive cells and cell death. Ann Anat. 2011;193(2):156–62.
Basaran R, Senol M, Ozkanli S, et al. Correlation of matrix metalloproteinase (MMP)-1, -2, -3, and – 9 expressions with demographic and radiological features in primary lumbar intervertebral disc disease. J Clin Neurosci. 2017;41:46–9.
Kao TS, Peng YJ, Salter DM, et al. Nerve growth factor increases MMP9 activity in annulus fibrosus cells by upregulating lipocalin 2 expression. Eur Spine J. 2015;24(9):1959–68.
Xiao L, Ding MM, Saadoon O, et al. A novel culture platform for fast proliferation of human annulus fibrosus cells. Cell Tissue Res. 2017;367(2):339–50.
Ahmed E, Saleh T, Yu L, et al. Decellularized extracellular matrix-rich hydrogel-silver nanoparticle mixture as a potential treatment for acute liver failure model. J Biomed Mater Res A. 2020;108(12):2351–67.
Moriguchi Y, Borde B, Berlin C, et al. In vivo annular repair using high-density collagen gel seeded with annulus fibrosus cells. Acta Biomater. 2018;1:79.
Wei Q, Liu DC, Chu GL, et al. TGF-β1-supplemented decellularized annulus ffbrosus matrix hydrogels promote annulus ffbrosus repair. Bioact Mater. 2022;10:19.
Acknowledgements
This study was supported by funding from the National Natural Science Foundation of China (82172427); National Natural Science Foundation of Anhui Province (2208085MH211); Excellent Young Project of Anhui Provincial University Research Project (2023AH030104); Anhui Provincial Clinical Medical Research Center for Spinal Deformities “Medical Innovation Fund” Youth Project (AHJZJX-QN2023-001), the Youth Research Foundation of Anhui Medical University (2021xkj092), Key Project of Wannan Medical College (WK2021ZF14), and “Peak” Training Program for Scientific Research of Yijishan Hospital, Wannan Medical College (GF2019T02, GF2019G07, and GF2019G12).
Author information
Authors and Affiliations
Contributions
The experimental design was executed by Chen Liu, while the implementation of the experiment was conducted by both Chen Liu and Xin Ge. Chen Liu took on the responsibility of writing the manuscript. Xin Ge and Yifeng Li was in charge of proofreading and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, C., Ge, X. & Li, Y. Repair of annulus fibrosus defects using decellularized annulus fibrosus matrix/chitosan hybrid hydrogels. J Orthop Surg Res 19, 535 (2024). https://doi.org/10.1186/s13018-024-05017-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-05017-y