Abstract
Background
The bone status of postmenopausal women is worsening. In fact, postmenopausal period is the high incidence stage of osteoporosis and falls. Notably, a recent study has pointed out that exercise can improve bone health in postmenopausal women. However, the effect of Tai Chi exercise on postmenopausal women is controversial. Therefore, a meta-analysis was designed to analyze the effect of Tai Chi exercise on bone health and fall prevention in postmenopausal women.
Methods
The researches on Tai Chi improving the bone health of postmenopausal women before August 31, 2023 were collected from Chinese and English databases, such as PubMed, Embase, and Web of Science, etc. The risk of bias of the included studies was assessed using the Cochrane risk-of-bias tool for randomized trials. Besides, R software 4.3.1 was employed to analyze the effect sizes in the meta-analysis to summarize the impact of Tai Chi on vertebral bone mineral density, serum calcium, clinical balance scores, the number of falls, total falls, and health status scores in postmenopausal women.
Results
There were 12 studies eventually included in this meta-analysis. A total of 1,272 postmenopausal women were involved, including 628 in the experimental group (intervention with Tai Chi exercise) and 644 in the control group (without any intervention). Briefly, postmenopausal women practicing Tai Chi presented a significant increase in vertebral bone density [standardized mean difference (SMD) = 0.37, 95% confidence interval (CI) (0.04–0.71), P = 0.03] and health status score [SMD = 0.25, 95% CI (0.01–0.49), P = 0.04]. In contrast, there were no significant differences for postmenopausal women between the two groups in terms of serum calcium [SMD = -0.01, 95% CI (-0.39, 0.36), P = 0.77], clinical balance [SMD = 0.17, 95% CI (-0.01, 0.46), P = 0.23], number of falls [SMD = -0.61, 95% CI (-1.24, 0.02), P = 0.06] and total falls [odds ratio = 0.35, 95% CI (0.11–1.12), P = 0.07].
Conclusion
Tai Chi exercise can improve the bone mineral density of postmenopausal women, thereby maintaining bone health. Hence, Tai Chi exercise is necessary to prevent osteoporosis.
Similar content being viewed by others
Introduction
A study has shown that the bone mineral density (BMD) of women decreases by 9–10% from one year before menopause to three years after menopause. The decrease of BMD mainly occurs in the cancellous bone in the early stage of menopause, while after the age of 65 years, it is predominantly manifested as cortical bone loss [1]. When the estradiol concentration decreases by 50% or the follicle-stimulating hormone concentration doubles, the BMD of lumbar spine separately declines by 10% and 39%, and the BMD of femoral neck correspondingly declines by 12% and 27% [2]. Such process is considered as postmenopausal osteoporosis. As a systemic disease, postmenopausal osteoporosis is characterized with an increased risk of fracture caused by decreased bone mass and damaged bone microarchitecture [3]. Up to now, osteoporosis has been recognized as a major health problem worldwide. It is estimated that 200 million people suffer from osteoporosis worldwide, of which postmenopausal women account for 30% [4]. The balance between bone formation and resorption is disrupted by the decrease in estrogen levels after menopause. As described by a study, estrogen can increase osteogenic differentiation and osteoblast maturation of mesenchymal stem cell, thereby promoting bone formation [5]. Besides, estrogen deficiency in women inhibits bone anabolism and osteoclasts function, leading to persistent bone destruction [6]. Notably, the imbalance in the interaction between immunocyte and osteocyte is also an essential factor triggering osteoporosis [7]. Due to particularly complicated mechanism, postmenopausal osteoporosis attracts much attention from researchers.
Currently, the purpose of the prevention and treatment of postmenopausal osteoporosis is to reduce or stop bone loss, increase BMD and bone strength, and prevent falls. There are two main treatment strategies, namely, pharmacological and non-pharmacological treatments [8]. Of them, pharmacological treatment mainly focuses on hormones, including tibolone and bisphosphonates. However, all of these drugs bring adverse effects, even complications, to patients [9]. It is worth noting that exercise can enhance muscle strength, dynamic balance, coordination, and overall functional performance. As demonstrated by Daly, R. M. et al., exercise benefited to postmenopausal women with osteoporosis [10]. Also, Kemmler et al. performed a meta-analysis for the effects of different exercise modalities on postmenopausal osteoporosis. Their results revealed that different exercise modalities could improve osteoporosis in patients [11]. Notably, Tai Chi, a traditional exercise in China, is popular among middle-aged and elderly people. Tai Chi is an exercise combined meditation with slow, gentle movement that is easy to learn. Interestingly, a number of studies have shown that Tai Chi contributes to increasing BMD, thereby preventing or improving osteoporosis [12, 13]. A study conducted by Wayne et al. further illustrated the effect of Tai Chi on improving osteoporosis in postmenopausal women [14]. However, a recent meta-analysis conducted by Li et al. evaluated the efficacy and safety of Tai Chi exercise for bone health. The results revealed that Tai Chi exercise did not benefit from serum phosphorus, alkaline phosphatase and BMD of the femoral shaft and forearm in peri-menopausal and postmenopausal women. Besides, they concluded that Tai Chi exercise is safe for perimenopausal and postmenopausal women [15]. Therefore, there is still controversy about the role of Tai Chi in bone health and fall prevention in postmenopausal women. A meta-analysis was performed in this paper to search and systematically evaluate all clinical studies on the effects of Tai Chi on bone health and fall prevention in postmenopausal women. The results from our study will be useful as a reference for postmenopausal women and health care providers interested in Tai Chi training. Furthermore, they will be helpful for researchers in designing future clinical trials to more comprehensively disclose the role of Tai Chi in the improvement of bone health in postmenopausal women.
Methods and material
Literature search
Several authoritative medical and biomedical literature databases were searched, and these databases included PubMed, Embase, Willey Library, Web of Science, China National Knowledge Infrastructure, Wanfang, and Chinese Science and Technology Periodical Database. The searched literature was limited to English and Chinese, and the data update was available up to August 31, 2023. The English search terms consisted of “Tai Chi”, “Postmenopausal Women”, “Bone Health” and “Fall Prevention”. The search strategies were shown as follows: (“Tai Chi” or “Postmenopausal Women”) and (“Bone Health” or “Fall Prevention”). The corresponding Chinese keywords were adopted for the data search from Chinese database. The specific search strategy is shown in Supplementary Table 1.
Inclusion and exclusion criteria
Inclusion criteria were shown as follows: (1) Subjects: postmenopausal women, including those entering menopause for the first time or having been in postmenopausal stage for a long time; with a clear description of age and years of menopause. (2) Interventions: subjects in the experimental group were intervened with Tai Chi exercise, while subjects in the control group were not intervened by any measures or simple stretching exercises. (3) Outcome measures: ① vertebral bone density; ② serum calcium; ③ clinical balance score: the one-leg stand test, in which the subject stands on one leg for as long as possible with both arms along the side of the body. The test is interrupted after 60 s or when the subject’s swinging leg touches the ground. Record the best score. ④ number of falls; ⑤ total falls; ⑥ health status score: The assessment was carried out using the Short Form of the Health Status Questionnaire (SF-36). The higher the score, the better the status. (4) Study type: clinical randomized controlled trials (RCT).
Exclusion criteria were listed as follows: (1) Case reports, reviews, meta-analyses, commentaries, conference abstracts, animal studies; (2) patients in the experimental group were subject to Tai Chi combined with other interventions; (3) studies with incomplete or unclear data.
Data screening and extraction
Initial screening was completed by two independent researchers based on titles and abstracts, and during initial screening, studies that were irrelevant or did not meet the inclusion criteria were extracted. Then, further screening involved full text to ensure that the included literature was fully compliant with the criteria. Divergent literature was subjected to discussion or third-party arbitration to reach consensus. As for the included studies, two researchers independently extracted data, and the extracted data included basic information of studies, characteristics of subjects, implementation details of Tai Chi exercise and outcome measures. All extracted data were cross-validated to ensure accuracy and consistency. Discrepancies were resolved through discussion or with the assistance of a third party.
Risk of bias
Two independent reviewers used the Cochrane risk-of-bias tool for RCT to assess the risk of bias of the included studies from five domains: the randomization process, deviation from intended intervention, missing outcome data, outcome measures, and selection of the reported results. Each domain was judged by “low risk”, “uncertain”, or “high risk” based on corresponding algorithms. The risk of bias was assessed via two independent reviewers, followed by cross-checking. Two reviewers discussed the disagreements or consulted with a third reviewer.
Statistical analysis
Meta effect size analysis was performed in this study using R software 4.3.1, and Cochrane literature quality assessment was plotted using Reviewer Manager 5.4. Continuous and dichotomous variables were adopted in this paper. For dichotomous variables, odds ratio (OR) and 95% confidence interval (CI) were calculated; for continuous variables, the standardized mean difference (SMD) and 95% CI were calculated. Heterogeneity was measured by the I2 statistic and Q test. I2 < 50% or P < 0.1 indicated that the heterogeneity was significant, and the random-effect model was used for analysis. Otherwise, the fixed-effect model was performed to analyze. The funnel plot, Egger’s and Begg’s tests were used to assess publication bias when the included studies exceeded 10. The level of statistical significance for all results was set as P < 0.05.
Results
Literature search results
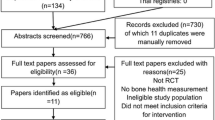
A total of 563 articles were searched from Chinese and English databases based on the search strategy. After removing 54 duplicated articles by using Endnote X8, 509 articles were collected. Next, 436 articles that were obviously inconsistent with the theme of this article were excluded preliminarily. The remaining 72 articles (removing 1 article for which full text was unavailable) were subject to full-text reading and detailed evaluation, of which 60 articles were further excluded. Ultimately, 12 studies were included for meta-analysis [14, 16,17,18,19,20,21,22,23,24,25,26]. The flow diagram of the literature screening was shown in Fig. 1.
A total of 1,272 postmenopausal women were enrolled in this study, including 628 in the experimental group (interference with Tai Chi exercise) and 644 in the control group. The general information on the literature included was shown in Table 1.
Risk of bias assessment
Figure 2 illustrates the risk of bias assessment for the included studies. The randomized methods were clearly described in the all literature, ensuring comparability at the baseline between the experimental and control groups. However, double-blind designs, in particular, have only been applied in 25% studies; selective reports were absent in 66.7% studies. Overall, the included literature satisfied our requirements.
Meta-analysis results
Vertebral bone density
The results of vertebral BMD were reported in 7 literature [14, 17, 22,23,24,25,26]. Heterogeneity among the included papers was analyzed by a random effects model (I2 = 67% and P < 0.01). According to the meta-analysis results, postmenopausal women interfered with Tai Chi exercises showed a significant increase in vertebral BMD compared to the control group [SMD = 0.37, 95% CI (0.04–0.71), P = 0.03] (Fig. 3).
Serum calcium
Of all included literature, there was 3 literature reporting serum calcium results [20, 21, 23]. The heterogeneity was not observed among the included literature (I2 = 35% and P = 0.21) based on the fixed effect model. Meta-analysis results showed that there was no significant difference in serum calcium between postmenopausal women interfered with Tai Chi exercise and the control group [SMD = -0.01, 95% CI (-0.39,0.36), P = 0.77] (Fig. 4).
Clinical balance
The results of clinical balance scores were reported in 3 included literature [14, 16, 18]. There was no heterogeneity among the included literature (I2 = 0% and P = 0.98) using a fixed effects model. The results showed that no significant difference was found in clinical balance between the two groups of postmenopausal women [SMD = 0.17, 95% CI (-0.01,0.46), P = 0.23] (Fig. 5).
Number of falls
The number of falls was mentioned in 2 studies [18, 19]. Significant heterogeneity among the included literature (I2 = 82% and P = 0.02) was analyzed by a random effects model. Meta-analysis outcomes showed that relative to the control group, there was no difference in the number of falls among postmenopausal women practicing Tai Chi exercises [SMD = -0.61, 95% CI (-1.24, 0.02), P = 0.06] (Fig. 6).
Number of total falls
The outcome of total falls was reported in 3 included studies [14, 17, 19]. No heterogeneity was shown among the included literature (I2 = 0% and P = 0.69), so a fixed effects model was employed for analysis. According to the meta-analysis, the number of total falls among postmenopausal women practicing Tai Chi exercise were the same as that in the control group [OR = 0.35, 95% CI (0.11–1.12), P = 0.07] (Fig. 7).
Health status scores
Health status scores were compared in 4 literature [14, 16, 18, 21]. There was no heterogeneity among the included literature (I2 = 0% and P = 0.69), so a fixed effects model was adopted for analysis. The analysis results displayed that health status scores of postmenopausal women practicing Tai Chi exercise were significantly higher than those of the control group [SMD = 0.25, 95% CI (0.01–0.49), P = 0.04] (Fig. 8).
Discussion
Healthy bones are the support to maintain normal life activities. However, osteoporosis will bring a lot of safety hazards, threatening human life and health. The risk of osteoporosis is significantly increased in postmenopausal women relative to menopausal women, resulting in many women being deeply disturbed [27]. Fortunately, a recent study has concluded that appropriate exercises is effective in preserving BMD of the lumbar spine, femoral neck, total hip, and total body in postmenopausal women [28]. Tai chi is a slow and gentle exercise combined with deep breathing and relaxation. Tai Chi enhances muscle strength, particularly in the lower limbs, through its gentle, flowing movements. This improvement in musculoskeletal function helps support the skeletal system and can lead to increased bone density, reducing the risk of osteoporosis common in postmenopausal women [29, 30]. Although direct evidence is limited, some studies suggest that Tai Chi can modulate hormones related to bone metabolism, which could be particularly beneficial for postmenopausal women experiencing hormonal changes [31, 32]. Tai Chi incorporates meditative elements that help in reducing stress and anxiety [32]. High stress levels are associated with increased cortisol production, which can negatively impact bone density. However, it is still controversy about the effect of Tai Chi exercise on bone health in postmenopausal women. 12 literature related to bone health and fall prevention in postmenopausal women was collected in this study. After analysis, we observed that Tai Chi exercise could increase BMD and health status scores in postmenopausal women, but did not affect serum calcium, clinical balance score, number of falls and total number of falls. All in all, Tai Chi exercise is able to improve BMD and bone health in postmenopausal women. Previous meta-analysis [33] also demonstrated that Tai Chi could improve the BMD of the lumbar spine, femoral neck, and trochanter in postmenopausal women. However, them didn’t access the effect of Tai Chi on falls. The findings of our research serve as a valuable addition to it.
The studies (n = 12) included in this study belonged to RCT. There were limitations in most of the RCT, including lack of detailed methodology and poor quality of study design. Notably, among these 12 studies, a large heterogeneity existed when analyzing spinal BMD and number of falls.
Besides, some potential limitations of this study also should be considered. Tai Chi exercise, as a physical activity, may be affected by many factors, such as practice intensity, attendance, and single exercise duration [34]. In the included literature, the practice time of Tai Chi in the experimental group was not equal, ranging from 4 months to more than 12 months, with a relatively long time span. Moreover, it cannot be ignored that these studies came from different regions, including Canada, Hong Kong, China, Poland, the United States, Australia, and mainland China. A potential problem should be noticed that there are more than five schools of Tai Chi in China alone [35]. For example, Chen style Tai Chi is famous for its fast speed, powerful movements, and deep postures, while Yang Style Tai Chi advocates for slow, continuous, large movements, and high postures. Additionally, Wu style Tai Chi is different from Chen and Yang style [35]. Although Yang style Tai Chi is now the most popular, there is also a significant number of people who practice Chen and Wu style [36]. It is worth noting that different Tai Chi styles may have different effects on bone health in postmenopausal women. Also, the impact of Tai Chi exercises on different races is different [37, 38]. Finally, the studies included in this meta-analysis had small sample sizes and low methodological quality. Therefore, further well-designed, long-term and feasible RCT are needed to explore the effects of Tai Chi exercises on bone health in postmenopausal women.
Conclusion
To sum up, Tai Chi exercise could improve BMD and increase health status scores in postmenopausal women. Besides, we believe our results are reliable. However, more detailed and high-quality trials are needed to confirm the effects of Tai Chi exercise.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
- BMD:
-
Bone mineral density
- RCT:
-
Randomized controlled trials
- OR:
-
Odds ratio
References
Anagnostis P, Bosdou JK, Vaitsi K, Goulis DG, Lambrinoudaki I. Estrogen and bones after menopause: a reappraisal of data and future perspectives. Horm (Athens). 2021;20(1):13–21.
Shieh A, Greendale GA, Cauley JA, Karvonen-Gutierrez C, Crandall CJ, Karlamangla AS. Estradiol and follicle-stimulating hormone as predictors of Onset of Menopause Transition-related bone loss in pre- and Perimenopausal women. J Bone Min Res. 2019;34(12):2246–53.
Fischer V, Haffner-Luntzer M. Interaction between bone and immune cells: implications for postmenopausal osteoporosis. Semin Cell Dev Biol. 2022;123:14–21.
Lobersztajn A, Tremollieres F. [Menopause and bone]. J Gynecol Obstet Biol Reprod (Paris). 2012;41(7 Suppl):F28–32.
McNamara LM. Osteocytes and Estrogen Deficiency. Curr Osteoporos Rep. 2021;19(6):592–603.
Lu L, Tian L. Postmenopausal osteoporosis coexisting with Sarcopenia: the role and mechanisms of estrogen. J Endocrinol. 2023;259(1).
Wu D, Cline-Smith A, Shashkova E, Perla A, Katyal A, Aurora R. T-Cell mediated inflammation in postmenopausal osteoporosis. Front Immunol. 2021;12:687551.
Yong EL, Logan S. Menopausal osteoporosis: screening, prevention and treatment. Singap Med J. 2021;62(4):159–66.
Lobo RA, Pickar JH, Stevenson JC, Mack WJ, Hodis HN. Back to the future: hormone replacement therapy as part of a prevention strategy for women at the onset of menopause. Atherosclerosis. 2016;254:282–90.
Daly RM, Dalla Via J, Duckham RL, Fraser SF, Helge EW. Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz J Phys Ther. 2019;23(2):170–80.
Kemmler W, Shojaa M, Kohl M, von Stengel S. Effects of different types of Exercise on Bone Mineral density in Postmenopausal women: a systematic review and Meta-analysis. Calcif Tissue Int. 2020;107(5):409–39.
Zou L, Wang C, Chen K et al. The Effect of Taichi Practice on attenuating bone Mineral density loss: a systematic review and Meta-analysis of Randomized controlled trials. Int J Environ Res Public Health 2017;14(9).
Zhang Y, Chai Y, Pan X, Shen H, Wei X, Xie Y. Tai Chi for treating osteopenia and primary osteoporosis: a meta-analysis and trial sequential analysis. Clin Interv Aging. 2019;14:91–104.
Wayne PM, Kiel DP, Buring JE, et al. Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: a pilot pragmatic, randomized trial. BMC Complement Altern Med. 2012;12:7.
Li J, Guo J, Wang X, et al. Efficacy and safety of Tai Chi exercise on bone health: an umbrella review. Osteoporos Int. 2023;34(11):1853–66.
Barbat-Artigas S, Filion ME, Dupontgand S, Karelis AD, Aubertin-Leheudre M. Effects of Tai Chi training in dynapenic and nondynapenic postmenopausal women. Menopause. 2011;18(9):974–9.
Chan K, Qin L, Lau M, et al. A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women. Arch Phys Med Rehabil. 2004;85(5):717–22.
Chyu MC, James CR, Sawyer SF, et al. Effects of Tai Chi exercise on posturography, gait, physical function and quality of life in postmenopausal women with osteopaenia: a randomized clinical study. Clin Rehabil. 2010;24(12):1080–90.
Li F, Harmer P, Fitzgerald K, et al. Effectiveness of a therapeutic Tai Ji Quan Intervention vs a Multimodal Exercise intervention to Prevent Falls among older adults at high risk of falling: a Randomized Clinical Trial. JAMA Intern Med. 2018;178(10):1301–10.
Liu G, Liu. Xiaojin. Effects of taijiquan exercise on bone mineral density and bone metabolism indexes in postmenopausal women. Contemp Sports Sci Technol. 2021;11:19–21.
Shen CL, Chyu MC, Pence BC, et al. Green tea polyphenols supplementation and Tai Chi exercise for postmenopausal osteopenic women: safety and quality of life report. BMC Complement Altern Med. 2010;10:76.
Wang H, Yu B, Chen W, Lu Y, Yu D. Simplified Tai Chi Resistance Training versus Traditional Tai Chi in slowing bone loss in Postmenopausal Women. Evid Based Complement Alternat Med. 2015;2015:379451.
Xiao C, Kang Y, Zhuang YC. Effects of Tai Chi Ball on Estrogen levels, bone metabolism index, and muscle strength of Perimenopausal Women. J Am Geriatr Soc. 2015;63(12):2629–31.
al YYe. Effects of Tai Chi exercise on bone mineral density in postmenopausal women. Chin Rehabilitation Theory Pract 2012;18.
J Z. Changes in bone mineral density in perimenopausal women receiving tai chi exercise. Chin Tissue Eng Res 2020;24.
al ZJe. Effects of long-term taijiquan exercise on bone mineral density and balance in postmenopausal women. Chin Rehabilitation Theory Pract 2011;17.
Gosset A, Pouilles JM, Tremollieres F. Menopausal hormone therapy for the management of osteoporosis. Best Pract Res Clin Endocrinol Metab. 2021;35(6):101551.
Zhao R, Zhang M, Zhang Q. The effectiveness of Combined Exercise interventions for preventing postmenopausal bone loss: a systematic review and Meta-analysis. J Orthop Sports Phys Ther. 2017;47(4):241–51.
Choi JH, Moon JS, Song R. Effects of Sun-style Tai Chi exercise on physical fitness and fall prevention in fall-prone older adults. J Adv Nurs. 2005;51(2):150–7.
Ahmad OS, Leong A, Miller JA, et al. A mendelian randomization study of the effect of Type-2 diabetes and glycemic traits on bone Mineral Density. J Bone Min Res. 2017;32(5):1072–81.
Esch T, Duckstein J, Welke J, Braun V. Mind/body techniques for physiological and psychological stress reduction: stress management via Tai Chi training - a pilot study. Med Sci Monit. 2007;13(11):CR488–497.
Nedeljkovic M, Ausfeld-Hafter B, Streitberger K, Seiler R, Wirtz PH. Taiji practice attenuates psychobiological stress reactivity–a randomized controlled trial in healthy subjects. Psychoneuroendocrinology. 2012;37(8):1171–80.
Liu X, Jiang C, Fan R, et al. The effect and safety of Tai Chi on bone health in postmenopausal women: a meta-analysis and trial sequential analysis. Front Aging Neurosci. 2022;14:935326.
Sun Z, Chen H, Berger MR, Zhang L, Guo H, Huang Y. Effects of Tai Chi exercise on bone health in perimenopausal and postmenopausal women: a systematic review and meta-analysis. Osteoporos Int. 2016;27(10):2901–11.
Yeung A, Chan JSM, Cheung JC, Zou L. Qigong and Tai-Chi for Mood Regulation. Focus (Am Psychiatr Publ). 2018;16(1):40–7.
Yang GY, Sabag A, Hao WL, et al. Tai Chi for health and well-being: a bibliometric analysis of published clinical studies between 2010 and 2020. Complement Ther Med. 2021;60:102748.
Siu KC, Padilla C, Rajaram SS. The interrelationship between balance, Tai Chi and depression in latino older adults. Aging Clin Exp Res. 2017;29(3):395–401.
Jimenez ER, Juarez J, Struwe L, Cohen MZ. Tai Chi as a complementary therapy for depression and anxiety among U.S. Veterans in a Mental Health Inpatient setting. J Am Psychiatr Nurses Assoc 2023:10783903231201592.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Yi Zhang and Huan Chen contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yi Zhang. The first draft of this manuscript was written by Yi Zhang and Huan Chen. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Y., Chen, H. Effect of Tai Chi exercise on bone health and fall prevention in postmenopausal women: a meta-analysis. J Orthop Surg Res 19, 471 (2024). https://doi.org/10.1186/s13018-024-04962-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04962-y