Abstract
Background
Historically, ankle fractures have been treated with open reduction and internal fixation (ORIF) procedures, which are considered safe and effective. Patient characteristics may contribute to postoperative difficulties thereby increasing risk of hospital readmission. The objective of this study was to determine the frequency of and reasons for 30-day readmission and postoperative complications following ORIF for ankle fractures.
Methods
A retrospective review of the National Surgical Quality Improvement Program (NSQIP) database from 2015 to 2021 identified patients undergoing ORIF for ankle fractures. Patient demographics, complication incidence, and reasons for unplanned hospital readmission were collected. Multivariable analyses identified patient risk factors for any adverse event (AAE) and readmission within 30-days of surgery.
Results
The 29,905 patients queried who underwent ORIF procedures for ankle fractures between 2015 and 2021 were 49.6 ± 18.40 years of age, 30.9 ± 7.10 kg/m2, and 40.81% male. Of this cohort, 981 (3.30%) experienced 30-day postoperative adverse events, with surgical site infections (SSI; 1.25%) the most common. Unplanned readmission was observed in 2.08% of patients after a mean of 14.64 days. Surgical site related readmissions were 20.55% (n = 128) of reported readmissions with the most common being superficial incisional SSI. Notable risk factors for adverse events included ASA class (OR = 1.579, P < .001), COPD (OR = 1.522, P < .001), bleeding disorders (OR = 1.489, P = .001), diabetes (OR = 1.254, P = .008), and current smoking status (OR = 1.295, P = .002). Risk factors for readmission were ASA class (OR = 1.762, P < .001), COPD (OR = 1.599, P < .001), bleeding disorder (OR = 1.711, P < .001), diabetes (OR = 1.494, P < .001), end stage renal disease (OR = 3.304, P < .001), steroid use (OR = 2.144, P < .001), and current smoking status (OR = 1.667, P < .001).
Conclusion
Despite a low adverse event rate, 2% of patients required unplanned readmission after ORIF for ankle fractures. Surgical site complications account for almost half of reported readmissions. ASA class and various medical comorbidities were found to significantly increase the risk of postoperative adverse events and hospital readmission.
Similar content being viewed by others
Introduction
Ankle fractures are a common musculoskeletal injury that is often seen in athletes, the elderly population, and those with osteoporosis [1,2,3]. It has been estimated that between 2016 and 2019, the incidence of ankle fractures in the United States was 14.1 per 10,000 patient years [4]. While some injuries can be treated conservatively with bracing and analgesics, unstable ankle joints may require surgical intervention. The incidence of surgery for ankle fractures may be up to 3.3 per 10,000 patient years [4]. Moreover, the prevalence of these injuries was estimated to have a financial burden of 367 million dollars in relation to perioperative admissions, with Medicare patients being disproportionately affected [5, 6]. As value-based care and bundled payment models become a central part of orthopedic surgeries, the reduction of costs, readmissions, and adverse events is a growing priority [6, 7].
The vast majority of ankle fractures are successfully treated with surgical open reduction internal fixation (ORIF) procedures with postoperative complication rates between 1–40% [6, 21, 25, 26]. Certain risk factors may predispose patients to postoperative difficulties such as pain, loss of reduction, development of arthritis, and infections [4, 8,9,10,11]. Thus, patients face an increased burden of care, decreased quality of life, and greater financial strain [4, 6, 7]. Identification and reduction of the comorbidities that impede care for ankle fractures is a growing priority for surgeons, especially when considering the need for surgical interventions over conservative ones [12]. However, identification of high-risk patients is always a point of contention and individualized assessments are not always feasible on a large scale for physicians. With an increased transition to outpatient procedures, further data is also required to identify patients who are at risk for readmission [2, 4, 6].
Very few database studies have investigated 30-day outcomes and risk factors following ORIF for ankle fractures [7, 13,14,15]. Most of these studies either emphasize specific comorbidities in relation to postoperative outcomes or have small cohorts that have not been updated [7, 10, 16]. A recent study investigated the risk factors for readmissions after ankle fracture surgeries between 2013 and 2014 using the American College of Surgeon’s National Surgical Quality Improvement Program (NSQIP) database [9]. The authors found that strong predictors of readmission included ASA class and a history of pulmonary disease. Several other studies identify a history of diabetes, bleeding disorders, and age as risk-factors for adverse events or readmission [3, 9, 10, 16, 17].
Our study aims to expand upon existing literature by determining the reasons for 30-day readmission and postoperative adverse events following ORIF for ankle fractures using NSQIP data in a large cohort over a period of seven years (2015 to 2021). We hypothesize that previously elucidated trends in literature that report ASA class, age, and chronic illnesses as strong predictors of readmission or adverse events, will hold. Additionally, we hypothesize that reasons for readmission will be sequelae of these underlying comorbid conditions.
Methods
Study design
This is a retrospective cohort study of prospectively collected data as part of the ACS-NSQIP database. This registry contains demographics, comorbidities, and laboratory values with corresponding readmission, excluding emergency department visits, and complication rates within 30 days of the indexed procedure. Patients are identified through Current Procedural Terminology (CPT) and International Classification of Diseases (ICD), Ninth and Tenth Revision codes [18]. NSQIP-participating hospitals each employ trained nurse surgical clinical reviewers to oversee data collection adding an additional quality measure. All patients are monitored for 30 days postoperatively for any adverse events (AAEs), readmissions, and reoperations. No outcome differences exist between institutions participating in the NSQIP program and nonparticipants [19]. The ACS NSQIP database is comprised of a network of hospitals which are required to employ surgical clinical reviewers to collect 274 variables from surgical procedures. The database implements several quality assurance measures, such as biweekly random internal audits, which have reported < 1.8% inter-rater disagreement [20, 21].
Data collection
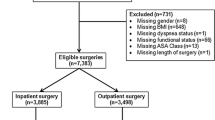
Data was collected for adult patients (at least 18 years old) who had undergone ORIF procedures from 2015 to 2021 for medial malleolus fracture (CPT 27766), posterior malleolus fracture (CPT 27769), distal fibular fracture (CPT 27792), bimalleolar ankle fracture (CPT 27814), trimalleolar ankle fracture (medial and/or lateral malleolus; with or without fixation of posterior lip) (CPT 27822 and CPT 27823), distal tibiofibular joint disruption (CPT 27829), and ankle dislocation, with or without percutaneous skeletal fixation; with or without repair or internal or external fixation (CPT 27846 and CPT 27848). All cases were isolated procedures without any concomitant procedures, thus excluding subjects with polytrauma. Cases of ankle dislocation were included on the basis of requiring operative intervention and fixation, and did not include fracture. The 7-year study period was chosen to expand upon the most recent published articles regarding this topic, while allowing for more comprehensive insight into a larger population. Patient demographics, including age, smoking status, body mass index (BMI), gender, medical comorbidities, operative time, and American Society of Anesthesiologists (ASA) physical status classification scores were collected along with complication data for each. Age and BMI were treated as continuous variables. Subjects with missing data entries were excluded from the cohort.
For each patient, length of stay (LOS), readmission rate, reason for readmission, death, and 30-day complications were collected. Included in these complications were superficial and deep surgical site infections (SSI), wound dehiscence, pneumonia, unplanned intubation, pulmonary embolism, postoperative renal insufficiency or failure, urinary tract infection, cerebrovascular accident, cardiac arrest, myocardial infarction (MI), transfusions, deep vein thrombosis (DVT), sepsis, and return to the operative room. For the purposes of data analysis, the complications were grouped and redefined as Any Adverse Event (AEE). LOS was categorized as the number of days from procedure to postoperative discharge. An extended LOS was defined as greater than the 75% quartile LOS (≥ 2 d) for the entire sample.
Statistical analysis
Multivariate logistic regression with robust error variance was carried out using R-Studio software version 2023.06.0 + 421 (R Foundation for Statistical Computing, Vienna, Austria). Demographic variables were included as predictors, and risk factors for AAE and readmission were identified. Statistical significance was set a priori at P < .05.
Results
A total of 981 (3.30%) patients experienced 30-day postoperative adverse events, with extended LOS (19.80%) being the most common event and stroke (0.05%) the least. Unplanned readmission was observed in 2.08%, with a mean time to readmission of 14.64 days (Table 1). Of the readmissions, 128 (20.55%) were related to the surgical site, with superficial incisional SSI (6.74%) being the primary cause (Table 2). Patients undergoing operative intervention and fixation for ankle dislocations had the highest readmission rate at 4.10%, with posterior malleolus repair having the lowest at 0.95% (Table 1).
The 29,905 patients identified for this study from 2015 to 2021 were 49.6 ± 18.40 years of age, 30.9 ± 7.10 kg/m2, and 40.81% male. In this cohort, hypertension (31.13%) and diabetes (12.14%) were the most common comorbidities, followed by COPD (3.15%) and bleeding disorders (2.96%). There was a mean ASA class of 2.1 ± 0.70. Our cohort also had a smoking status prevalence of 22.66% (Table 3). Bimalleolar fractures were the most common fracture type (36.37%), followed by lateral malleolus fractures (26.18%), trimalleolar fractures (26.18%), medial malleolus fractures (5.10%), distal tibiofibular joint disruption (4.95%), ankle dislocation (0.82%), and posterior malleolus (0.71%) (Table 3).
Risk factors for any adverse event
Significant risk factors for AAE after ankle fracture surgery included age (OR = 1.023, P < .001), BMI (OR = 1.051, P < .001), ASA class (OR = 1.579, P < .001), partially dependent functional status (OR = 1.735, P < .001), fully dependent functional status (OR = 2.509, P < .012), current smoking status (OR = 1.295, P = .002), congestive heart failure (OR = 2.993, P < .001), dialysis (OR = 1.947, P = .002), bleeding disorders (OR = 1.489, P = .001), preoperative transfusion (OR = 3.037, P < .001), diabetes (OR = 1.254, P = .008), and COPD (OR = 1.522, P < .001) (Table 4).
Risk factors for readmission
After ORIF ankle surgery, significant risk factors for readmission were age (OR = 1.015, P < .001), operative time (OR = 1.002, P = .040), ASA class (OR = 1.762, P < .001), partially dependent functional status (OR = 1.863, P < .001), fully dependent functional status (OR = 3.066, P = .006), current smoking status (OR = 1.667, P < .001), dialysis (OR = 3.304, P < .001), steroid use (OR = 2.144, P < .001), hypertension (OR = 1.266, P = .022), bleeding disorder (OR = 1.711, P < .001), diabetes (OR = 1.494, P < .001), and COPD (OR = 1.599, P < .001) (Table 4).
Discussion
This study sought to identify causes for 30-day readmission and postoperative adverse events following ORIF for ankle fractures using the NSQIP database. To our knowledge, this is the largest study, consisting of a cohort of 29,906 patients over 7 years, that looks not only at multiple risk factors, but also clarifies reasons for readmission (without ED visits). In our analysis, age, BMI, ASA class, partially and fully dependent functional status, smoker status, congestive heart failure, dialysis, bleeding disorder, preoperative transfusion, diabetes, and COPD were all significant predictors of any adverse events following surgery. Of these risk factors, BMI, congestive heart failure, and preoperative transfusion did not predict readmissions. Other risk factors for readmission included operative time, steroid use, and hypertension. Surgical site complications accounted for almost half of all readmissions, when excluding unknown or unreported reasons. Of these complications, superficial incisional SSI was the largest contributor, followed by deep incisional SSI. When stratifying by fracture, ankle dislocations requiring ORIF saw the greatest number of adverse events and readmissions. Repair of distal tibiofibular joint fractures saw 1.55% of patients experiencing SSI, followed by trimallelolar fractures at 1.40%.
Our analysis is novel compared to previous similar studies like those by Basques et al. and Belmont et al. in that it outlines the specific reasons for readmission rather than only reporting total readmission and risks for these readmissions [8, 22]. It also identifies a greater number of risk factors for readmission. While Basques et al. only identified an ASA class ≥ 3 as a significant risk factor for readmission, our analysis supplemented these findings by identifying additional factors (Table 4). Our study also presents a lower readmission rate from the initial publication of the NSQIP study by Basque et al. [8] We found that although the adverse event rate after ORIF for ankle fractures was relatively low (3.3%), roughly 2% of all patients required unplanned hospital readmission, compared to 3.17% in the aforementioned study. In this case, it is also important to make the distinction that readmission data was only available for 2521 of 4412 patients included in their study [8]. In contrast, we confirm the findings of Fu et al. that surgical site complications, reported to be 42.2% in their paper, are a notable reason for readmission after ORIF for ankle fractures [9]. Additionally, results of the present study confirm the existing data and support our hypothesis that age, ASA class, and chronic illnesses are key predictors of readmission or adverse events [8, 9, 22]. Overall, the present study sought to consolidate and update the gap in the subject in recent years through a larger cohort over a longer period of time.
In our study, the most common reasons for readmission unrelated to the surgical site were venous thromboembolism, including pulmonary embolism and deep vein thromboses. We identified bleeding disorders as predictors of adverse events and readmissions. These findings align with the observations made by Malyavko et al., who reported a higher incidence of complications among patients with bleeding disorders within 30 days of undergoing ORIF for ankle fractures [17]. The implications of these conclusions are evident in the incidence of VTE which accounted for 7.22% (DVT: 1.28%; pulmonary embolism: 5.94%) of all readmissions in the present study. Consideration of fracture type in relation to VTE showed that patients undergoing ORIF for distal tibiofibular joint disruption experienced the greatest relative amount of DVT and PE, accounting for 2.43% of all patients. The presence of bleeding disorders, in conjunction with factors such as age, diabetes, congestive heart failure, and dialysis, are predictive of VTE, which has been shown to collectively increase readmissions [16]. This is likely due to decreased mobility of the operative leg and lack of early weight-bearing ambulation due to pain, postoperative protocol, or both. It can be postulated that bleeding disorders may confer an elevated risk of VTE, particularly following foot and ankle surgeries [16, 17]. Overall, other orthopedic procedures such as ORIF for hip fractures seem to follow similar trends with surgical complications and VTE being strong reasons for unplanned readmissions [23, 24]. For these reasons, the foot and ankle surgeon should consider the risk of postoperative VTE in their surgical candidates and mitigate risk however possible in this vulnerable population.
Chronic obstructive pulmonary disease was identified as a significant risk factor for adverse events and readmissions. Chronic obstructive pulmonary disease has been indicated to be predictive of readmissions and adverse events following ORIF for ankle surgeries in multiple studies [8,9,10, 22]. Gupta et al. looked at a cohort of 9,986 patients using NSQIP from 2006 to 2018 to compare groups with and without a history of COPD and their postoperative outcomes. They found that patients with COPD were at higher risk for readmission (9.6%), compared to those without (2.5%). The COPD group also experienced a greater number of complications such as pneumonia, but not operative complications or VTE. Nonetheless, the presence of COPD seemed to predispose patients to greater adverse events and readmission. The present study, similar to Gupta et al., demonstrates that patients with COPD are more likely to experience 30-day postoperative complications after ORIF.
Diabetes was found to be a risk factor for adverse events and readmission in our study, which is consistent with other literature [25]. Liu et al. conducted a matched cohort study comparing readmission rates between patients with and without diabetes and found significant differences between the two groups [25]. When adjusted for age and comorbidities, patients with diabetes were 1.7 times more likely to experience readmission, which is in line with our findings (odds ratio of 1.474; P < .001). This may be attributed to impaired wound healing that is associated with the decreased blood supply, infection, and neuropathy in diabetic patients undergoing orthopedic surgery [25, 26].
Smoking has been implicated as a hindrance in bone and wound healing, potentially explaining SSI, and was a significant predictor of readmissions in our study [8, 27, 28]. Sagherian et al. compared readmissions in smoking and nonsmoking patients following surgical fixation of ankle fractures and found significant differences [28]. They reported that superficial incisional SSIs were notable reasons for readmission in smoking patients compared to nonsmoking patients (0.10% versus 0.20%; P < .001). However, these are in contrast to Miller et al., who did not find smoking to be a risk factor for adverse events [27]. An important difference between the present study and Miller et al. is that they broadly classified wound complications as major or minor, rather than the complication itself. The authors attributed the decreased comparative risk in their single institution to their ability to counsel patients regarding smoking cessation [27].
Some broader differences arise in regards to risk factors of both adverse events and readmissions when compared to other studies [8, 9, 22]. Primarily, our study identified a greater number of significant predictors for adverse events such as age, BMI, smoker status, congestive heart failure, dialysis, bleeding disorder, preoperative transfusion, and diabetes. Our predictors for readmission also included age, operative time, smoker status, steroid use, hypertension, dialysis, bleeding disorder, and diabetes. This may be attributable to our larger cohort or longer time period of collected data. Other predictors in our study were also more specific, such as looking at congestive heart failure instead of a broader history of cardiac disease, or COPD instead of pulmonary disease, and considering both partially and fully dependent functional status [8, 9, 22].
Limitations
While this study offers findings on readmissions after ORIF for ankle fractures, it is not without limitations, many of which are related to the database used. A large percentage (nearly 60%) of reasons for readmission after ORIF for ankle fractures were not reported in the database. It is possible that the distribution of readmission reasons would differ between the reported and non-reported patients. For patients with reported reasons for readmission and complications, however, there is an inherent risk of misclassified data that may skew outcomes for any studies using the NSQIP database. Additionally, NSQIP does not provide any perioperative data related to severity of fracture such as radiographic findings, or method of fixation, which can significantly alter the difficulty of surgical repair and affect postoperative complications. Functional outcomes such as pain, joint range of motion, postoperative imaging, or postoperative activity levels are also not included in NSQIP, leaving out outcome data that is of particular interest to orthopedic surgeons. In regard to specific risk factors such as bleeding disorders, there is no categorization for the types of disorders encompassed in the group [17]. Further, explanations for reduced postoperative recovery in patients with diabetes and smoking may not be fully observed as NSQIP only tracks patients for 30 days [25, 28].
Beyond limitations related to NSQIP, our inclusion of ankle dislocations may inadvertently include more serious ankle fractures, such as pilon fractures, which were not coded by the surgeon and subsequently not considered in this analysis. Similarly, not separating diabetic ankle neuropathic fractures assumes they are included in the study, but does not account for the resultant variation in readmissions and adverse events, especially since diabetes is a significant predictor for both. Conversely, excluding other fracture types such as open fractures may overlook the differences in challenges and outcomes compared to closed fractures, even when treated with ORIF. Differentiating between these fracture types in future studies may provide more comprehensive insights into readmission and complication patterns in patients.
In its statistical methods, the present study accounts for confounding by use of multivariate logistic regression. Multicollinearity was not accounted for, thereby leading to wider confidence intervals and potentially altering the significance of some predictors. Furthermore, specific risk factors such as bleeding disorder and preoperative transfusions may be related, with the former potentially increasing the need for the latter. We chose to include both under the assumption that bleeding disorders are uncommon causes of anemia necessitating transfusions in the setting of trauma. Instead, we suspect that the majority of preoperative transfusions are due to secondary causes of anemia including hemorrhage or insensible loss. This cannot be substantiated within the dataset and poses limitations to our study.
When investigating LOS, we are limited by varying protocols between centers. Although patients with more severe injuries are expected to have longer LOS, some facilities may require a minimum inpatient time, whereas others treat all injuries as outpatient procedures. Finally, treating BMI as a continuous variable may neglect non-linear relationships; a low BMI may not necessarily confer increased risks.
Conclusion
The results of this study corroborate existing literature in that COPD, diabetes, smoking, and bleeding disorders continue to be strong predictors of readmission. Additionally, surgical site infections were the most common reasons for readmission while pulmonary embolism was the most frequent non-surgical site-related reason for readmission. Our study also identifies a number of risk factors such as COPD, smoking status, diabetes, bleeding disorders, and ASA class for both adverse events and readmission. The prominence of these risk factors in existing literature is relevant to the reasons for readmission in our study and demonstrates a greater need to take appropriate preoperative precautions. When preparing for ORIF for ankle fractures, it is important to counsel patients on predisposing risk factors for adverse events and costly hospital readmission.
Data availability
The datasets generated and/or analyzed during the current study are available in the American College of Surgeons ACS National Surgical Quality Improvement Program repository.
References
Magan A, Golano P, Maffulli N, Khanduja V. Evaluation and management of injuries of the tibiofibular syndesmosis. Br Med Bull. 2014;111(1):101–15. https://doi.org/10.1093/bmb/ldu020
Qin C, Dekker RG, Helfrich MM, Kadakia AR. Outpatient Management of Ankle fractures. Orthop Clin North Am. 2018;49(1):103–8. https://doi.org/10.1016/j.ocl.2017.08.012
Sinha A, Robertson G, Maffulli N, Doctor. I fractured my ankle. When can I return to play? An updated systematic review. Br Med Bull. 2022;143(1):35–45. https://doi.org/10.1093/bmb/ldac016
Vanderkarr MF, Ruppenkamp JW, Vanderkarr M, Parikh A, Holy CE, Putnam M. Incidence, costs and post-operative complications following ankle fracture – A US claims database analysis. BMC Musculoskelet Disord. 2022;23:1129. https://doi.org/10.1186/s12891-022-06095-x
Belatti DA, Phisitkul P. Economic burden of foot and ankle surgery in the US Medicare Population. Foot Ankle Int. 2014;35(4):334–40. https://doi.org/10.1177/1071100713519777
Stull JD, Bhat SB, Kane JM, Raikin SM. Economic Burden of Inpatient Admission of Ankle fractures. Foot Ankle Int. 2017;38(9):997–1004. https://doi.org/10.1177/1071100717709576
Gordon AM, Malik AT. Anemia severity and the Risks of Postoperative Complications Following Total Ankle Arthroplasty. Foot Ankle Spec. Published Online June. 2022;29:19386400221106650. https://doi.org/10.1177/19386400221106650
Basques BA, Miller CP, Golinvaux NS, Bohl DD, Grauer JN. Morbidity and Readmission after Open reduction and internal fixation of ankle fractures are Associated with Preoperative patient characteristics. Clin Orthop. 2015;473(3):1133–9. https://doi.org/10.1007/s11999-014-4005-z
Fu MC, Young K, Cody E, Schairer WW, Demetracopoulos CA, Ellis SJ. Most readmissions following ankle fracture surgery are unrelated to Surgical Site issues: an analysis of 5056 cases. Foot Ankle Orthop. 2017;2(2):2473011417695254. https://doi.org/10.1177/2473011417695254
Gupta P, Quan T, Abdo MG, Manzi JE, Knapp B, Shaffer G. Thirty-day morbidity and mortality in patients with COPD following open reduction and internal fixation for rotational ankle fractures. J Foot Ankle Surg. 2022;61(6):1275–9. https://doi.org/10.1053/j.jfas.2022.03.015
SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Jt Surg-Am Vol. 2009;91(5):1042–9. https://doi.org/10.2106/JBJS.H.00653
Gougoulias N, Khanna A, Sakellariou A, Maffulli N. Supination-External Rotation Ankle fractures: Stability a Key Issue. Clin Orthop. 2010;468(1):243–51. https://doi.org/10.1007/s11999-009-0988-2
Del Balso C, Halai MM, MacLeod MD, Sanders DW, Rahman Lawendy A. Factors Predictive of Early Complications Following Total Ankle Arthroplasty. Foot Ankle Orthop. 2022;7(2):24730114221102456. https://doi.org/10.1177/24730114221102456
Smith KS, Drexelius K, Challa S, Moon DK, Metzl JA, Hunt KJ. Outcomes following ankle fracture fixation with or without Ankle Arthroscopy. Foot Ankle Orthop. 2020;5(1):2473011420904046. https://doi.org/10.1177/2473011420904046
Tedder C, DeBell H, Dix D, et al. Comparative Analysis of Short-Term Postoperative Complications in Outpatient Versus Inpatient Total Ankle Arthroplasty: a database study. J Foot Ankle Surg. 2019;58(1):23–6. https://doi.org/10.1053/j.jfas.2018.06.003
Brennan J, Keblish D, Friedmann E, Spirt A, Holt E, Turcotte J. Postoperative venous thromboembolism risk-prediction in foot and ankle fracture surgery. Foot. 2023;56:102017. https://doi.org/10.1016/j.foot.2023.102017
Malyavko A, Quan T, Stoll WT, et al. Association of Bleeding Disorders and Risk of complications following open reduction and internal fixation of the ankle. Foot Ankle Int. 2022;43(4):551–9. https://doi.org/10.1177/10711007211058163
Khuri SF. The NSQIP: a new frontier in surgery. Surgery. 2005;138(5):837–43. https://doi.org/10.1016/j.surg.2005.08.016
Molina CS, Thakore RV, Blumer A, Obremskey WT, Sethi MK. Use of the National Surgical Quality Improvement Program in Orthopaedic surgery. Clin Orthop. 2015;473(5):1574–81. https://doi.org/10.1007/s11999-014-3597-7
Davis CL, Pierce JR, Henderson W, et al. Assessment of the Reliability of Data Collected for the Department of Veterans Affairs National Surgical Quality Improvement Program. J Am Coll Surg. 2007;204(4):550–60. https://doi.org/10.1016/j.jamcollsurg.2007.01.012
Trickey AW, Wright JM, Donovan J, et al. Interrater Reliability of Hospital Readmission Evaluations for Surgical patients. Am J Med Qual. 2017;32(2):201–7. https://doi.org/10.1177/1062860615623854
Belmont PJ, Davey S, Rensing N, Bader JO, Waterman BR, Orr JD. Patient-based and Surgical Risk factors for 30-Day postoperative complications and Mortality after Ankle fracture fixation. J Orthop Trauma. 2015;29(12):e476–82. https://doi.org/10.1097/BOT.0000000000000328
Martin CT, Gao Y, Pugely AJ. Incidence and risk factors for 30-Day readmissions after hip fracture surgery. Iowa Orthop J. 2016;36:155–60.
Minhas SV, Kester BS, Lovecchio FC, Bosco JA. Nationwide 30-Day readmissions after elective orthopedic surgery: reasons and implications. J Healthc Qual JHQ. 2017;39(1):34. https://doi.org/10.1097/JHQ.0000000000000045
Liu JW, Ahn J, Raspovic KM, et al. Increased Rates of Readmission, Reoperation, and Mortality following open reduction and internal fixation of ankle fractures are Associated with Diabetes Mellitus. J Foot Ankle Surg. 2019;58(3):470–4. https://doi.org/10.1053/j.jfas.2018.09.023
Kwon NF, Danilkowicz RM, Kim J, Grimm NL, Adams SB. Short-term complications following total ankle arthroplasty and Associated Risk factors: a NSQIP database analysis. Foot Ankle Spec. 2023;16(3):214–20. https://doi.org/10.1177/19386400211072379
Miller AG, Margules A, Raikin SM. Risk factors for Wound complications after Ankle fracture surgery. JBJS. 2012;94(22):2047. https://doi.org/10.2106/JBJS.K.01088
Sagherian BH, Hoballah JJ, Tamim H. Comparing the 30-Day complications between smokers and nonsmokers undergoing Surgical fixation of ankle fractures. Foot Ankle Orthop. 2022;7(3):24730114221115677. https://doi.org/10.1177/24730114221115677
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
A.S. was responsible for Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. P.B.W. and C.R.W. were responsible for Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – review & editing. J.S. and C.N.O. were responsible for Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. A.A., T.P., A.H., S.A., J.L., K.S. were responsible for Conceptualization, Project administration, Supervision, Validation, Writing – review & editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
(1) Dr.Samuel Adams, MD: Royalties or licenses from Conventus flexthread; consulting fees from Exactech, Enovis; compensation from Stryker; stock and stock options from Restor3d, 4Web (2) Dr. Albert Anastasio, MD: consulting fees from QPIX Solutions (3) Dr. Andrew Hanselman, MD: consulting fees from OneSurgical; compensation from Arthrex, Exactech (4) Dr. Karl M. Schweitzer, Jr. MD: consulting fees from Stryker Inc, Arthrex, Inc., TAR consulting; Ibex Charcot Solutions Inc.; Leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid from Ibex Charcot Solutions Inc., Tayco Brace Inc.; Stock or stock options in Ibex Charcot Solutions Inc., Restor3D Inc., Tayco Brace Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sharma, A., Wyatt, P.B., Reiter, C.R. et al. Readmission within 30-days of open reduction and internal fixation for ankle fractures: NSQIP analysis of 29,905 patients. J Orthop Surg Res 19, 576 (2024). https://doi.org/10.1186/s13018-024-04895-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04895-6