Abstract
Background
This study aimed to evaluate the effect of foraminoplasty using large-channel endoscopy during TESSYS on the biomechanics of the lumbar spine.
Methods
A complete lumbar spine model, M1, was built using 3D finite elements, and models M2 and M3 were constructed to simulate the intraoperative removal of the superior articular process of L5 using a trephine saw with diameters of 5 mm and 8.5 mm, respectively, and applying normal physiological loads on the different models to simulate six working conditions—anterior flexion, posterior extension, left-right lateral bending, and left-right rotation—to investigate the displacement and facet joint stress change of the surgical segment, and the disc stress change of the surgical and adjacent segments.
Results
Compared with the M1 model, the M2 and M3 models showed decreased stress at the L4-5 left FJ and a significant increase in stress at the right FJ in forward flexion. In the M2 and M3 models, the L4-5 FJ stresses were significantly greater in left lateral bending or left rotation than in right lateral bending or right rotation. The right FJ stress in M3 was greater during left rotation than that in M2, and that in M2 was greater than that in M1. The L4-5disc stress in the M3 model was greater during posterior extension than that in the M1 and M2 models. The L4-5disc stress in the M3 model was greater in the right rotation than in the M2 model, and that in the M2 model was greater than that in the M1 model.
Conclusion
Foraminoplasty using large-channel endoscopy could increase the stress on the FJ and disc of the surgical segment, which suggested unnecessary and excessive resection should be avoided in PTED to minimize biomechanical disruption.
Similar content being viewed by others
Introduction
Lumbar disc herniation (LDH) is a common and frequent disease in spinal surgery that seriously affects patients’ quality of life and imposes a heavy economic burden on their families and society [1, 2]. Patients with LDH who fail to respond to strict conservative treatment require surgical treatment. Traditional open surgery requires extensive incisions of the lumbar muscles and vertebral plate, and postoperative epidural scar formation is prone to cause adhesions between the dura and nerve roots, resulting in renewed compression of the dural sac, restricted nerve root movement, and possible recurrence of clinical symptoms or even surgical failure [3, 4]. A study by Ross et al. [5] revealed a significant correlation between postoperative radicular symptoms and epidural scar formation, with as many as 24% of patients suffering from scar formation resulting in prolonged postoperative pain in the lumbar spine.
The emergence of percutaneous endoscopic transforaminal discectomy (PETD) is epoch-making, and the technique has become widely popular in the last decade [6,7,8]. Depending on the size of the patient’s intervertebral foramen and the location of the herniated disc, intraoperative foraminoplasty is often required in PETD [9,10,11]. During the process of foraminoplasty, the superior articular process and synchondral ligaments are damaged to varying degrees. The lumbar facet joint (FJ) is a synovial joint that consists of a synovial membrane, joint capsule, joint fluid, and articular cartilage structures [12]. FJs play a role in restricting and guiding the movement of the spine and effectively prevent discs from being damaged by excessive shear and torsional tension. Therefore, angular changes, intraoperative injuries or even resection of the lumbar articular process may accelerate the surgical segment degeneration or even lead to degenerative spinal disease [13].
In recent years, large-channel endoscopes have become increasingly widely used in clinical practice [14, 15]. Large-channel endoscopes have a wider working channel than ordinary endoscopes and allow use of larger surgical instruments, which are minimally invasive and highly efficient. Large-channel endoscopes are usually combined with the use of an 8.5-mm-diameter trephine, which can enlarge the working space of endoscopy, making it easier to expose protruded disc, dural sac and nerve roots, but causing more damage to the FJ compared with ordinary endoscopes. To our knowledge, however, there are few studies investigating the effect of large-channel endoscopes-based foraminoplasty on lumbar biomechanics in percutaneous endoscopic discectomy.
In the present study, the authors employed the three-dimensional finite element method to simulate ordinary endoscopes-based and large-channel endoscopes-based foraminoplasty respectively on L5 superior articular process in lumbar percutaneous endoscopic discectomy, hereby to study the effect of large-channel endoscopes-based foraminoplasty on the biomechanics of operating segment and adjacent segments in percutaneous endoscopic lumbar discectomy.
Materials and methods
Experimental materials
Experimental subjects
One healthy male adult volunteer (35 years old, height 178 cm, weight 75 kg, no history of previous spinal diseases or spinal trauma) was selected for physical examination. Lumbar spine positive and lateral, hyperextension and hyperflexion films were used to exclude spinal pelvic deformity and other spinal diseases. Informed consent was signed, discussed and approved by the Ethics Committee of the Affiliated Hospital of Xuzhou Medical University.
Imaging equipment
A Siemens 64-slice spiral CT scanner (Siemens Sensation Open CT scanner, Siemens, Erlangen, Germany) provided by the Department of Imaging of the Affiliated Hospital of Xuzhou Medical University was used.
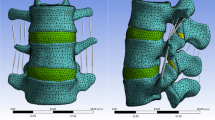
Establishment of the normal L1-S1 3D finite element model
CT image processing and 3D image reconstruction of the L1-S1 vertebrae
The patient’s lumbar spine CT data was imported into Mimics in DICOM format, the segmentation threshold was set to 226–1612, the region growth mode was set to “6-connectivity”, and the model was optimized by mask separation, fill and mask separation. When generating the 3D geometric model, select the “high” quality level. After the 3D model is obtained, the smoothing process is carried out, the “Iterations” is set to 5, and the “Smooth factor” is set to 0.4.
Mesh the 3D model of theL1-S1 vertebrae
Using the remesh tool to enter the Mimics comes with the Magics plug-in, showing the vertebra 3D solid surface mesh division, Magics has a powerful face mesh redrawing (remesh) function, the use of which the Smoothing tool to smooth the face mesh processing, and then use the Triangle reduction to remove some of the quality of the low Then use Triangle reduction to remove some of the poor quality triangular surface pieces, and then observe the surface of the model and manually edit and eliminate the surfaces that are still of poor quality. The modified face mesh model is shown in Fig. 1.
Modeling process of each intervertebral disc, articular cartilage, ligament and joint capsule in the model
The anterior longitudinal ligament, posterior longitudinal ligament, supraspinous ligament, interspinous ligament, articular capsule ligament, and intertransverse ligament were constructed in the model using three-dimensional rod units. According to the literature [16], endplates were created on the upper and lower surfaces of the vertebral body with a thickness of 1 mm. between the upper and lower endplates was the intervertebral disc, which consisted of the annulus fibrosus and the nucleus pulposus (Nucleus pulposus). The nucleus pulposus was first added between the upper and lower endplates, and then four 1.5-mm-thick concentric rings were added around the nucleus pulposus to form the annulus fibrosus. The fibers of the annulus fibrosus are constructed from rod units that can only withstand tension, and in the annulus the fibers travel in a scissor-like pattern and form an average angle of 25° to 40° to the disc. The nucleus pulposus accounts for approximately 44% of the disc volume, and the center of the nucleus pulposus is located approximately 3.5 mm behind the center of the disc. The boundary of the intervertebral discs was offset inward by 12 mm, and then its center is displaced backward by 3.5 mm, and the resulting is the boundary of the nucleus pulposus (Fig. 2). The articular cartilage is created between the upper and lower articular processes.
Optimization of the model
Through the smooth and wrap functions in Mimics software, the finite element model was preliminarily processed, and the surface of the model was simplified by increasing the quality of the bone and introducing some irregular structures on the surface. The model was subsequently input into Geomagic Studio software to minimize the noise points of the point cloud, fill the ineffective cavities on the surface of the finite element model, remove the characteristic burrs and dents, smooth and relax the surface (Fig. 3), and finally obtain the geometric model of the L1-S1 segment for this experiment. The surface was smoothed and relaxed (Fig. 3) to obtain the L1-S1 segment geometry model for this experiment.
Segmenting the finite element model and assigning material properties to each tissue
A finite element model of the L1-S1 segment was generated, and the structures of cancellous bone, cortical bone and the posterior part of the vertebral body were established. The complete 3D model was imported into Ansys 18.0 computing software for finite element analysis, and the material properties were added to the material library according to the literature [17,18,19]. Then, the values were assigned to each structure, and the material parameters are shown in Tables 1 and 2.
Simulation of foraminoplasty on the three-dimensional finite element model
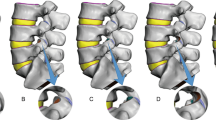
Basis on the normal L1-S1 3D finite element model, the following 3D finite element models were established based on the intraoperative situation by simulating the surgical procedure using Mimics software.
-
L4-5disc herniation without surgical treatment model (M1): Approximately 1/4 of the left posterior part of the L4-5 disc was defined as the material property of the degenerated disc, and other tissues such as the L3-4 and L5-S1 discs were defined as normal properties.
-
5 mm foraminoplasty model (M2): The fibrous annulus and nucleus pulposus of the left posterior 1/4 of the L4-5 intervertebral disc were removed to simulate resection of the protruding disc and replaced with scar tissue. The tip of the left superior articular process of L5 was used as the puncture point, 5 mm of bone was removed from the tip of the foraminoplasty site at an angle of approximately 30 degrees from the coronal plane to simulate the removal of part of the bone of the superior articular process, the foramen was enlarged, and foraminoplasty was performed. This model simulated the intraoperative removal of the L5 superior articular process using a conventional 5 mm-diameter trephine under ordinary endoscopy.
-
8.5 mm foraminoplasty model (M3): In the same way as above, this model simulated the intraoperative removal of the L5 superior articular process using a 8.5 mm-diameter trephine under large-channel endoscopy.
Loading conditions and observables
When the model is in the neutral position, the bottom of S1 is fixedly constrained, and the upper surface of the L1 endplate is not constrained as the location of pressure and moment application. When setting the magnitude and direction of the load, the ‘Component’ method is selected to set the load, which simulates the stress on the lumbar vertebrae caused by the weight of the human body under different conditions, so that the load is uniformly transmitted to the nodes on the surface. Pressure and moment were applied to the upper surface of the L1 vertebral body. Pressure and moment were 1175 N and 7.5 N⋅m in flexion, 500 N and 7.5 N⋅m in posterior extension, 700 N and 7.8 N⋅m in lateral flexion, and 720 N and 5.5 N⋅m in rotation [20,21,22], simulating the lumbar spine under six working conditions, including forward flexion, backward extension, left and right lateral bending and left and right rotation.
Definition of contact surfaces and interactions: After the model was assembled, the contact surfaces were defined according to the anatomical situation. For the relative sliding between the lumbar disc surfaces and the upper and lower endplates of each vertebral body, contact was defined as a “tie” pattern, with the upper and lower endplates of each vertebral body serving as the master surfaces, and the upper and lower surfaces of the disc serving as the follower surfaces. The FJ was set as a micromanipulation joint, and contact was defined as limited sliding contact with a friction coefficient of 0.1, with the next vertebral body’s upper articular process serving as the master surface.
Changes in the range of motion of the L4-5 segment under forward flexion, backward extension, left and right lateral bending and left and right rotation were observed in the three models. The stress changes in L3-4, L4-5 and L5-S1 discs of the three models were observed. The stress changes in L4-5 FJs were observed in the three models. For the recording of the simulation results, according to previous methods reported in the literature, data were collected in the region of maximum stress or displacement, and five points in the collection region were randomly selected and represented by the mean.
Statistical analyses
Statistical processing was carried out using SPSS 23.0 software, and measurement data are presented as the means ± standard deviations (‾x ± s). Comparisons of data between multiple groups were performed using one-way analysis of variance (ANOVA), and if the results of the analyses were overall different, then two-by-two comparisons were performed using the least significant difference (LSD) method. P < 0.05 was considered to indicate statistical significance.
Results
Normal 3D finite element modeling and validation
We established the L4-5disc herniation model (M1), 5 mm foraminoplasty model (M2) and 8.5 mm foraminoplasty model (M3) (Fig. 4), and compared with the model of Shim [23] (Table 3), we found that the range of motion (ROM) of the joints was in a reasonable range, which proved the validity of the present finite element model.
Mechanical changes after stress loading in the three models
Displacement analysis of L4 vertebra
As shown in Fig. 5, the differences in the degree of relative displacement of the L4 vertebra among the three models under the six working conditions were not statistically significant (P > 0.05).
Stress analysis of L4-5 facet joints
Compared with those in the M1 model, the stresses in the L4-5 left FJ decreased under forward flexion conditions in the M2 and M3 models (P < 0.05), but there was no significant difference between the M2 and M3 models (P > 0.05). There was no significant difference in the L4-5 left FJ stress between the M2 and M3 models under left lateral bending condition (P > 0.05), but both were greater than that of the M1 model (P < 0.05). Under posterior extension, right lateral bending, left rotation and right rotation working conditions, there was no statistically significant difference in L4-5 left FJ stress among the three models (P > 0.05). In the M2 and M3 models, the stress of the L4-5 left FJ was significantly greater than that in M1 in left lateral bending, left rotation, right lateral bending, and right rotation (Fig. 6a).
Under forward flexion condition, the L4-5 right FJ stress increased significantly in the M2 and M3 models compared with that of the M1 model (P < 0.05), but there was no significant difference between the M2 and M3 models (P > 0.05). The differences in L4-5 right FJ stress were not statistically significant among the three models under posterior extension, right and left lateral bending and right rotation working conditions (P > 0.05). Under left rotation condition, the L4-5 right FJ stress in M3 was greater than that in M2, and the stress in M2 was greater than that in M1, and the differences were statistically significant (P < 0.05). In the M2 and M3 models, the L4-5 right FJ stress was significantly greater than that in M1 under right lateral bending, right rotation, left lateral bending, and left rotation conditions (Fig. 6b).
Stress analysis of L4-5 discs
The L4-5 disc stress in the M2 and M3 models were greater than that in the M1 model under forward flexion, left rotation, and right and left lateral bending conditions, but the differences were not statistically significant (P > 0.05). L4-5 disc stress was greater in the M3 model than those in the M1 and M2 models under posterior extension condition (P < 0.05), whereas there was no significant difference between the M1 and M2 models (P > 0.05). Under right rotation condition, the L4-5 disc stress in the M3 model was greater than that in the M2 model, and the L4-5 disc stress in the M2 model than that in the M1 model, and the differences were statistically significant (P < 0.05) (Fig. 6c).
Stress analyses of the adjacent segmental discs
There was no significant difference in the stress distribution of L3-4 and L5-S1 discs among the three models under six working conditions (Fig. 6d and e).
Histograms of the stress distribution in facet joints and intervertebral discs under six working conditions. a: stress distribution in the left FJ of L4-5; b: stress distribution in the right FJ of L4-5; c: stress distribution in L4-5 disc; d: stress distribution in L3-4 disc; e: stress distribution in L5-S1 disc
Discussion
The FEA method can simulate the human body and analyze the biomechanical changes associated with different surgical methods on various parts of the spine and is widely used in the field of spinal surgery [24,25,26,27]. The L4-5 segment is the segment with the highest incidence of LDH, so in the present study, the L4-5 segment was used as the target segment, and the FEA method was used to establish a normal 3D finite element model of the L1-S1 segment. Based on this model, an intraoperative foraminoplasty model was established to investigate the effects of intraoperative foraminoplasty on lumbar spine biomechanics. A foraminoplasty model was established based on this model to investigate the effect of intervertebral foraminoscopy on the biomechanics of the lumbar spine in patients after foraminoplasty. Based on this model, a large-channel-based foraminoplasty model was established to investigate the effects of intraoperative foraminoplasty on lumbar biomechanics, providing a theoretical basis for improvement of treatment strategies and prediction of patient prognosis.
The first step after establishing a 3D finite element model is to verify the validity of the model, which is usually performed by comparing the experimental results with similar 3D finite element models from previous literature [28,29,30]. A comparison of our established finite element model with the results of Shim et al. [23] shows that the ROM of our model is within the error range reported in the literature and is comparable, indicating the validity of the finite element modeling method and material assignment in this paper, which can be used for biomechanical analysis. The modeling methods and loading constraints used in this study are the same as those used in previous studies, with only the individual samples differing, and the results are plausible from the point of view of a qualitative comparative study. The diversity of the individual morphology and material properties of vertebral cancellous bone means that finite element models do not exactly match the results of computer simulations with those of in vivo experiments [31, 32]. Most studies including the present study assign values based on previous studies, rather than patient-specific values, which is a limitation. The reason for this difference is the inconsistency in the sources used to construct the finite element models, and although the ideal approach would be to use the same in vitro experimental subject and finite element model object, this approach is essentially impossible for any experiment due to ethical issues. The advantage of using cadaveric samples for modeling is that the samples can be dissected and directly validated for each tissue, and the disadvantage is that the metrics in the physiological state are not available. Although the reconstruction of the human spine model can be achieved using cadaveric samples, it cannot be validated against homologous cadaveric samples, so the method of validating the finite element model is mainly to compare it with the test data of previous cadaveric specimens.
During TESSYS, depending on the size of the intervertebral foramen and the location of the herniated disc, foraminoplasty on one side is usually required to enlarge the foramen, a procedure that can injure the FJ to varying degrees. Previous studies have reported on the effect of conventional open surgery on FJs. Shah et al. [33] reported that 33–35% of FJs are injured during lumbar nailing via the transosseous interspace approach, whereas Monshirfar et al. [34] analyzed the probability of injury to the FJ during pedicle screw placement via the posterior median approach, and the presence of an injury to the FJ was detected on postoperative radiographs in approximately 15% of the patients. After we established a finite element model of intraoperative foraminoplasty, we analyzed the degree of displacement of the L4 vertebral body under different working conditions, and found that there was no significant difference in L4 vertebral body displacement among the three models, which suggests that intraoperative foraminoplasty is relatively safe and generally does not cause lumbar instability in the postoperative period.
Stress analyses of the L4-5 FJ in the three models revealed that after foraminoplasty, the stresses in the L4-5 bilateral FJ in the left lateral flexion condition increased compared with those in the preoperative condition in all patients and that the 8.5 mm foraminoplasty had a greater effect on the right FJ than did the 5 mm foraminoplasty. In two foraminoplasty models, the stress in the bilateral FJ of L4-5 was significantly greater in left lateral bending or left rotation than in right lateral benging or right rotation, and the magnitude of the increase was greater than that in the unoperated model, which suggests that foraminoplasty with an ipsilateral disc injury will lead to increased stress in the contralateral FJ. The larger the extent of foraminoplasty is, the greater the increased stress in the contralateral FJ. This finding suggests that it is better to minimize the removel of the FJ when performing foraminoplasty. Stress analysis of the L4-5 intervertebral discs of the three models showed that L4-5 intervertebral disc stress was greater in the M3 model than that in the M2 model under conditions of posterior extension and right rotation, which indicated that a large range of foraminoplasty might aggravate the degeneration of the intervertebral discs of the segments compared with a small range of foraminoplasty. In contrast, there was no significant difference in the distribution of L3-4 or L5-S1 disc stresses among the three models under various working conditions, suggesting that foraminoplasty had no significant effect on disc degeneration in adjacent segments. This is an advantage of nonfusion surgery over fusion surgery, as lumbar fusion surgery mostly accelerates the degeneration of neighboring segments [35,36,37,38].
There were several limitations in this study. First, the finite element models established in this study are similar to those that have been well-validated in previous studies, but they all simplify the physiological contraction force of the lumbar spine to varying degrees, especially simplifying the muscles connected to the lumbar spine and the weight of the upper body, which is still somewhat different from that of a real human body. Second, t FEA is an instant loading analysis method, which cannot systematically analyze the effect of fatigue loading on lumbar biomechanics. Third, the geometric characteristics of the intervertebral disc have a strong influence on the biomechanical behaviour of the segment [39], but in the current study, only a single geometry has been considered for disc modelling. Furthermore, the model did not take into consideration many patient-specific parameters, such as various level of degeneration and bulging, nutrient supply and biochemical alterations in intervertebral disc as proposed in previous study [40, 41]. In future, individualized computational modeling, which may incorporate patient-specific geometry and/or tissue properties, is needed to improve treatment strategies and patient prognosis.The actual clinical situation is complex and variable, and the repeated accumulation of stress in the lumbar spine after disc removal and foraminoplasty may accelerate the degeneration of the injured area.
The outcomes of the present study indicated that foraminoplasty using large-channel endoscopy increased the stress on the facet joints and disc of the surgical segment, which suggested unnecessary and excessive resection should be avoided in PTED to minimize biomechanical disruption. Further research should integrate clinical outcomes, a broader range of surgical scenarios and patient-specific models to valid the connection of these findings to the clinical outcomes and assess how individual variations in spinal anatomy affect the biomechanical and clinical outcomes, which could enhance the utility of these findings in patient selection, surgical planning, and the improvement of surgical procedures and patient prognosis.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- LDH:
-
Lumbar Disc Herniation
- FJ:
-
Facet Joint
- PETD:
-
Percutaneous Endoscopic Transforaminal Discectomy
- FSU:
-
Functional Spinal Unit
- FEA:
-
Finite Element Analysis
- PLIF:
-
Posterior Lumbar Interbody Fusion
References
Lucas CCosta J, Paixão J, Silva F, et al. Low back Pain: A Pain that May not be harmless. Eur J Case Rep Intern Med. 2018;5(3):000834.
Higgins DM, LaChappelle KM, Serowik KL, et al. Predictors of participation in a nonpharmacological intervention for Chronic Back Pain. Pain Med. 2018;19(suppl1):S76–83.
Samy Abdou M, Hardy RW Jr. Epidural fibrosis and the failed back surgery syndrome: history and physical findings. Neurol Res. 1999;21(Suppl 1):S5–8.
Almeida DB, Prandini MN, Awamura Y, Vitola ML, Simião MP, Milano JB, Bordignon KC, Ache MP, Ramina R. Outcome following lumbar disc surgery: the role of fibrosis. Acta Neurochir (Wien). 2008;150(11):1167–76.
Ross JS, Robertson JT, Frederickson RC, et al. Association between peridural scar and recurrent radicular pain after lumbar discectomy: magnetic resonance evaluation. ADCON-L European Study Group. Neurosurgery. 1996;38(4):855–61.
Choi SH, Adsul NM, Kim HS, et al. Percutaneous endoscopic interlaminar unilateral ventral Dural Approach for symptomatic bilateral L5-S1 herniated Nucleus Pulposus: technical note. J Neurol Surg Cent Eur Neurosurg. 2018;79(6):518–23.
Ao S, Wu J, Zheng W, et al. A Novel targeted Foraminoplasty device improves the efficacy and Safety of Foraminoplasty in Percutaneous endoscopic lumbar discectomy: preliminary clinical application of 70 cases. World Neurosurg. 2018;115:e263–71.
Tacconi L, Baldo S, Merci G, et al. Transforaminal percutaneous endoscopic lumbar discectomy: outcome and complications in 270 cases. J Neurosurg Sci. 2020;64(6):531–6.
Lee CW, Yoon KJ, Jun JH. Percutaneous endoscopic laminotomy with Flavectomy by Uniportal, Unilateral Approach for the Lumbar Canal or lateral recess stenosis. World Neurosurg. 2018;113:e129–37.
Liu X, Yuan S, Tian Y, et al. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: minimum 2-year follow-up results. J Neurosurg Spine. 2018;28(3):317–25.
Chen Z, Zhang L, Dong J, et al. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J Neurosurg Spine. 2018;28(3):300–10.
Van den Heuvel SAS, Cohen SPC, de Andrès Ares J. Pain originating from the lumbar facet joints. Pain Pract. 2024;24(1):160–76.
Wu W, Yu R, Hao H, Yang K, Jiao G, Liu H. Visible trephine-based foraminoplasty in PTED leads to asymmetrical stress changes and instability in the surgical and adjacent segments: a finite element analysis. J Orthop Surg Res. 2023;18(1):431.
Zhang F, Ye D, Zhang W, Sun Y, Guo L, Li J. Efficacy of lumbar decompression under large-channel spinal endoscope in elderly patients with segmental lumbar spinal stenosis. J Orthop Surg Res. 2024;19(1):16.
Sheng Y, Li J, Chen L, Geng M, Fen J, Sun S, Sun J. Delta large-channel technique versus microscopy-assisted laminar fenestration decompression for lumbar spinal stenosis: a one-year prospective cohort study. BMC Musculoskelet Disord. 2023;24(1):43.
Masni-Azian, Tanaka M. Biomechanical investigation on the influence of the regional material degeneration of an intervertebral disc in a lower lumbar spinal unit: a finite element study. Comput Biol Med. 2018;98:26–38.
Fan W, Guo LX. Influence of different frequencies of axial cyclic loading on time-domain vibration response of the lumbar spine: a finite element study. Comput Biol Med. 2017;86:75–81.
Srinivas GR, Kumar MN, Deb A. Adjacent disc stress following floating lumbar Spine Fusion: a finite element study. Asian Spine J. 2017;11(4):538–47.
Choi HW, Kim YE. Effect of lumbar fasciae on the stability of the lower lumbar spine. Comput Methods Biomech Biomed Engin. 2017;20(13):1431–7.
Rohlmann A, Zander T, Rao M, Bergmann G. Realistic loading conditions for upper body bending. J Biomech. 2009;42(7):884–90.
Dreischarf M, Rohlmann A, Bergmann G, Zander T. Optimised loads for the simulation of axial rotation in the lumbar spine. J Biomech. 2011;44(12):2323–7.
Dreischarf M, Rohlmann A, Bergmann G, Zander T. Optimised in vitro applicable loads for the simulation of lateral bending in the lumbar spine. Med Eng Phys. 2012;34(6):777–80.
Shim CS, Park SW, Lee SH, et al. Biomechanical evaluation of an interspinous stabilizing device. Locker Spine (Phila Pa 1976). 2008;33(22):E820–7.
Lee JH, Park WM, Kim YH, et al. A biomechanical analysis of an Artificial disc with a shock-absorbing core property by using whole-cervical spine finite element analysis. Spine (Phila Pa 1976). 2016;41(15):E893–901.
Pyles CO, Zhang J, Demetropoulos CK, et al. Material parameter determination of an L4-L5 motion segment finite element Model Under High Loading Rates. Biomed Sci Instrum. 2015;51:206–13.
Davidson Jebaseelan D, Jebaraj C, Yoganandan N, et al. Biomechanical responses due to discitis infection of a juvenile thoracolumbar spine using finite element modeling. Med Eng Phys. 2014;36(7):938–43.
DeVries Watson NA, Gandhi AA, Fredericks DC, et al. Sheep cervical spine biomechanics: a finite element study. Iowa Orthop J. 2014;34:137–43.
Sairyo K, Goel VK, Masuda A, et al. Three-dimensional finite element analysis of the pediatric lumbar spine. Part I: pathomechanism of apophyseal bony ring fracture. Eur Spine J. 2006;15(6):923–9.
Wheeldon JA, Pintar FA, Knowles S, et al. Experimental flexion/extension data corridors for validation of finite element models of the young, normal cervical spine. J Biomech. 2006;39(2):375–80.
Templeton A, Liebschner M. A hierarchical approach to finite element modeling of the human spine. Crit Rev Eukaryot Gene Expr. 2004;14(4):317–28.
Al-Barghouthi A, Lee S, Solitro GF, Latta L, Travascio F. Relationships among Bone Morphological parameters and Mechanical properties of Cadaveric Human Vertebral Cancellous Bone. JBMR Plus. 2020;4(5):e10351.
Solitro GF, Welborn MC, Mehta AI, Amirouche F. How to optimize pedicle screw parameters for the thoracic spine? A biomechanical and finite element Method Study. Global Spine J. 2024;14(1):187–94.
Shah RR, Mohammed S, Saifuddin A, et al. Radiologic evaluation of adjacent superior segment facet joint violation following transpedicular instrumentation of the lumbar spine. Spine (Phila Pa 1976). 2003;28(3):272–5.
Moshirfar A, Jenis LG, Spector LR, et al. Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine (Phila Pa 1976). 2006;31(22):2624–9.
Li XC, Huang CM, Zhong CF, et al. Minimally invasive procedure reduces adjacent segment degeneration and disease: new benefit-based global meta-analysis. PLoS ONE. 2017;12(2):e0171546.
Maruenda JI, Barrios C, Garibo F, et al. Adjacent segment degeneration and revision surgery after circumferential lumbar fusion: outcomes throughout 15 years of follow-up. Eur Spine J. 2016;25(5):1550–7.
Lee CH, Jahng TA, Hyun SJ, et al. Dynamic stabilization using the dynesys system versus posterior lumbar interbody fusion for the treatment of degenerative lumbar spinal disease: a clinical and radiological outcomes-based meta-analysis. Neurosurg Focus. 2016;40(1):E7.
Yue ZJ, Liu RY, Lu Y, et al. Middle-period curative effect of posterior lumbar intervertebral fusion (PLIF) and interspinous dynamic fixation (Wallis) for treatment of L45 degenerative disease and its influence on adjacent segment degeneration. Eur Rev Med Pharmacol Sci. 2015;19(23):4481–7.
Cappetti N, Naddeo A, Naddeo F, Solitro GF. Finite elements/Taguchi method based procedure for the identification of the geometrical parameters significantly affecting the biomechanical behavior of a lumbar disc. Comput Methods Biomech Biomed Engin. 2016;19(12):1278–85.
Volz M, Elmasry S, Jackson AR, Travascio F. Computational modeling intervertebral disc pathophysiology: a review. Front Physiol. 2022;12:750668.
Amirouche F, Solitro GF, Siemionow K, Drucker D, Upadhyay A, Patel P. Role of posterior elements in the disc bulging of a degenerated cervical spine. Int J Spine Surg. 2015;9:13.
Acknowledgements
Not applicable.
Funding
This study was support by the Xuzhou Young Reserve Medical Talent Development Project (XWRCHT20220038) and the Xuzhou Science and Technology Project (KC21210, KC23261).
Author information
Authors and Affiliations
Contributions
Wei Sun was responsible for writing the original draft, writing-review & editing, software, data compilation, and obtaining funding and was the main contributor to writing the manuscript. Duohua Li was responsible for processing the model and data compilation. Sicong Zhao was responsible for the software and validation. Hao Fu was responsible for creating the images. Jiayu Tian was responsible for data compilation and table creation. Feng Zhang analyzed the data. Dongying Wu was responsible for the writing of the original draft and concept development. Hu Feng is responsible for writing-review & editing, concept development, and supervision. All authors reviewed the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the Ethics Committee of the Second Affiliated Hospital of Xuzhou Medical University No. [2022] 080,701). Informed consent was obtained from the participants.
Consent for publication
We obtained informed consent from all participants and received their consent for publication of the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, W., Li, D., Zhao, S. et al. The effect of large channel-based foraminoplasty on lumbar biomechanics in percutaneous endoscopic discectomy: a finite element analysis. J Orthop Surg Res 19, 402 (2024). https://doi.org/10.1186/s13018-024-04870-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04870-1