Abstract
Background
The effects of the timing of surgical repair on the outcomes of traumatic and non-traumatic rotator cuff injuries (RCI) remain elusive. Thus, this study aimed to compare differences in outcomes following the repair of traumatic and non-traumatic RCI at varying time points.
Methods
The study population comprised 87 patients with traumatic and non-traumatic RCI who underwent arthroscopic rotator cuff repair and were followed up for a minimum of 6 months. Next, the trauma and the non-trauma groups were stratified into subgroups according to the time of injury (early repair: occurring within 3 months; delayed repair: occurring after 3 months). Measurements before and after surgical interventions were compared to evaluate the effect of the duration of RCI on the functional status of patients in the trauma and non-trauma groups. Primary evaluation indices included the Visual Analog Scale (VAS) pain score, American Shoulder and Elbow Surgeons (ASES) score, Constant shoulder function score, and the University of California, Los Angeles (UCLA) shoulder score. Secondary evaluation indices consisted of shoulder range of motion (ROM), postoperative rotator cuff retear rate, and incidence of joint stiffness.
Results
Among the 40 patients in the trauma group, 22 underwent early repair, whereas the remaining 18 underwent delayed repair. In the non-trauma group consisting of 47 patients, 18 underwent early repair, whereas the remaining 29 underwent delayed repair. The minimum clinical follow-up time was 6 months, with an average follow-up time of 10.2 months. During postoperative follow-up, 1 and 6 patients who underwent early and delayed repair experienced re-tear in the trauma group, respectively. Contrastingly, 3 and 8 patients who underwent early and delayed repair presented with re-tear in the non-trauma group, respectively.
Conclusion
Early repair of traumatic RCI yielded superior outcomes, including improved range of motion, lower pain symptoms, and lower risk of postoperative re-tears compared to delayed repair. Additionally, non-surgical treatment is recommended as the preferred approach for patients with non-traumatic RCI.
Similar content being viewed by others
Background
Rotator cuff injury (RCI) is a prevalent condition characterized by shoulder pain and dysfunction in adults, particularly the elderly [1,2,3]. Mounting evidence indicates [4] that among individuals aged over 60 years, 36% of individuals experience shoulder pain, and 16.9% of asymptomatic individuals develop shoulder tears. Notably, the causes of rotator cuff injuries are multifaceted, including intrinsic (nontraumatic) and extrinsic (traumatic) causes, and social factors. The degeneration of tendon tissue in RCI is a gradual process, exacerbated by the vulnerable location of the rotator cuff, rendering the cuff susceptible to friction and impingement, ultimately leading to partial or complete tendon tears [5]. While some patients respond to conservative treatment [6,7,8,9], those with severe tears often necessitate arthroscopic rotator cuff repair [10,11,12]. At present, total arthroscopic rotator cuff repair [13] is the most common surgical approach that involves single-row, double-row, or suture-bridge techniques based on tear severity [14,15,16]. Previous studies [17, 18] documented that patients with traumatic rotator cuff injuries generally exhibit better surgical outcomes, possibly attributable to improved tendon repair and a shorter injury-to-surgery interval. However, the influence of the duration of injury on postoperative outcomes in surgically repaired traumatic and nontraumatic patients remains to be elucidated, with the ideal timing for surgery in RCI being controversial [19, 20]. Therefore, evidence-based insights into the surgical management of traumatic and non-traumatic rotator cuff repairs are essential for achieving optimal patient outcomes.
This study aimed to compare the influence of the timing of surgical intervention on postoperative functional and clinical outcomes in patients with traumatic and non-traumatic rotator cuff injuries. We hypothesized that early repair results in greater improvements in range of motion (ROM) and clinical outcomes. Elucidating the effect of the timing of surgical intervention on postoperative outcomes of patients with rotator cuff repair with different tear etiologies may assist in preoperative counseling and shared clinical decision-making.
Methods
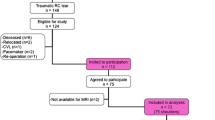
Participants
This retrospective study enrolled patients attending Lu’an Hospital of Traditional Chinese Medicine, affiliated with Anhui University of Traditional Chinese Medicine, between June 2021 and June 2023. It was approved by our Institutional Review Board, and the requirement for informed consent was waived by the committee owing to the retrospective nature of the study. All procedures were performed by the same experienced sports medicine physician and two assistants. The inclusion criteria were as follows: (1) patients aged above 18 years with a minimum follow-up duration of 6 months; (2) preoperative magnetic resonance imaging (MRI) was used for the diagnosis of rotator cuff injury; (3) patients undergoing primary arthroscopic rotator cuff repair. The exclusion criteria were: (1) comorbid shoulder osteoarthritis, shoulder instability, or fracture; (2) a history of shoulder surgery on the same side.
Study design
The clinical data of patients were acquired from chart review, including age, gender, affected limb side, smoking status, history of hypertension and diabetes mellitus, and mode of repair. Clinical data were recorded during preoperative and postoperative follow-up. The VAS score, American Shoulder and Elbow Surgeons (ASES) score, Constant Shoulder Function score, and the University of California at Los Angeles scoring system (UCLA) were assessed via questionnaires and physical examination. Meanwhile, shoulder mobility ROM was evaluated through active movement, comprising shoulder forward flexion (FF), external rotation (ER), and internal rotation (IR). Based on MRI images and intraoperative exploration of tendon integrity and involved tendons, tear type was categorized as either total or partial, and the morphology of the acromion and the performance of acromioplasty were evaluated to select the appropriate repair modality (single-row suture, double-row suture, and suture bridge technique) (Fig. 1). Postoperative complications following rotator cuff repair were documented during clinical follow-up visits, and final outcomes, including the incidence of rotator cuff retear and joint stiffness, were recorded at the 6th month. Shoulder stiffness was defined as a forward elevation of less than 120°, external rotation of less than 30°, and internal rotation of the back of less than L3. All imaging data were blindly assessed by two senior radiologists.
Study cohorts
Based on the history of trauma events and the presence of muscle edema in magnetic resonance images, patients were categorized into either the trauma group or the non-trauma group. Subsequently, each group was further stratified into early repair and delayed repair subgroups, resulting in a total of four groups. Within the trauma group, patients were classified into the early repair subgroup if the interval between shoulder cuff injury and surgery was within 3 months, whereas those with an interval exceeding 3 months were assigned to the delayed repair subgroup. Likewise, patients in the non-trauma group were categorized into the early repair subgroup if the duration of reported pain was less than 3 months and into the delayed repair subgroup if the duration exceeded 3 months. Comparisons were made between preoperatively and postoperative values at final follow-up within each cohort and between cohorts.
Statistical analysis
Variables following a normal distribution were expressed as mean ± standard deviation (SD), and the normality of the data was evaluated using the Kolmogorov-Smirnov test. Normally distributed data were analyzed using the t-test, whilst non-normally distributed data were compared using the Mann-Whitney U-test and expressed as the median and interquartile range (IQR). Categorical variable comparisons were performed using the chi-square test (X²) or Fisher’s exact test, depending on the distribution of the data. Statistical analyses were performed using SPSS Statistics 24.0 (Version 20.0, IBM Corporation, Armonk, NY), and differences were considered statistically significant at p < 0.05.
Results
Patient selection
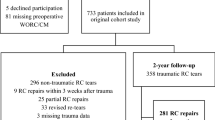
Ultimately, among the 106 rotator cuff injury patients whose charts were reviewed, 87 met the inclusion criteria (Fig. 2). Among patients with traumatic RCI, 22 patients underwent early repair, and 18 patients underwent delayed repair. Amongst patients with non-traumatic RCI, 18 patients underwent early repair, and 29 patients underwent delayed repair. In the traumatic group, gender (p = 0.751), age (p = 0.854), side of the affected limb (p = 0.737), the proportion of smokers (p = 0.731), hypertensive patients (p = 0.300), and diabetes patients (p = 0.680), as well as tear area (p = 0.409), duration of surgery (p = 0.546), type of repair (p = 0.748), number of full-layer tears (p = 0.750), and proportion of patients undergoing preoperative physical therapy (p = 0.185) and acromioplasty (p = 0.339) were comparable between the early and delayed repair groups. Similarly, in the non-traumatic group, gender (p = 0.760), age (p = 0.889), side of the affected limb (p = 0.869), the proportion of smokers (p = 0.673), hypertensive patients (p = 0.901), and diabetes patients (p = 0.788), as well as tear area (p = 0.775), duration of surgery (p = 0.742), type of repair (p = 0.948), number of full-layer tears (p = 0.345), and proportion of patients who received preoperative physical therapy (p = 0.055) and acromioplasty (p = 0.493) were comparable between the early and delayed repair groups (Table 1).
Imaging evaluation
In terms of involved tendons, there were no significant differences between the early repair subgroup and the delayed repair subgroup in the trauma and non-trauma groups (Table 2).
Functionality rating
Preoperative VAS score (p = 0.531), ASES score (p = 0.787), Constant score (p = 0.948), and UCLA score (p = 0.316) were comparable between patients undergoing early and delayed repair in the trauma group. Likewise, there was no significant difference in preoperative VAS score (p = 0.291), ASES score (p = 0.504), Constant score (p = 0.205), or UCLA score (p = 0.528) between early and delayed repair patients in the non-trauma group. However, during postoperative follow-up, functional scores such as VAS scores (1.18 ± 0.91 vs. 1.83 ± 1.04, p = 0.041), ASES scores (82.89 ± 2.67 vs. 76.49 ± 4.00, p < 0.001), Constant scores (81.73 ± 4.62 vs. 77.28 ± 4.71, p = 0.005), and UCLA scores (31.14 ± 1.52 vs. 28.56 ± 2.25, p < 0.001) were higher in the trauma group of patients undergoing early repair than those undergoing delayed repair. On the other hand, during the follow-up of patients undergoing early and delayed repair in the non-trauma group, no statistically significant differences were observed in VAS scores (p = 0.746), ASES scores (p = 0.624), Constant scores (p = 0.259), and UCLA scores (p = 0.091) (Table 3; Fig. 3).
Comparison of visual analog scale (VAS) score, American Shoulder and Elbow Surgeons (ASES) score, Constant shoulder function score, and University of California Shoulder Score (UCLA) between patients undergoing early repair and delayed repair in the trauma and non-trauma groups. A-D, Comparison of functional scores between patients undergoing early and delayed repair in the trauma group. E-H, Comparison of functional scores between patients undergoing early and delayed repair in the non-trauma group. Early repair in the trauma group resulted in better functional outcomes at 6 months than delayed repair. In the non-trauma group, no significant difference between early and delayed repair 6 months postoperatively was observed
Range of motion (ROM)
The range of motion of shoulder flexion (FF), external rotation (ER), and internal rotation (IR) were compared before and during follow-up across the 4 groups. The results revealed that the postoperative range of motion of patients undergoing early repair was superior to that of patients with delayed repair in the trauma group (FF, 149.55 ± 15.89 vs. 139.44 ± 12.10, p = 0.032; ER, 55.86 ± 5.93 vs. 49.44 ± 5.91, p = 0.002; IR, 41.36 ± 8.50 vs. 36.11 ± 6.98, p = 0.038). In comparison, early repair only outperformed delayed repair in terms of ER (55.56 ± 8.56 vs. 48.62 ± 14.26, p = 0.043) in the non-trauma group (Table 3).
Postoperative complication
During postoperative follow-up, 2 (9.1%) patients undergoing early repair and 3 (16.7%) patients undergoing delayed repair in the trauma group, as well as 2 (11.1%) patients undergoing early repair and 6 (20.7%) patients undergoing delayed repair in the non-trauma presented with joint stiffness; however, no statistically significant differences were noted between the two groups. Notably, these patients displayed improvements in joint stiffness during subsequent doctor-directed passive and active activities. At the same time, the incidence of rotator cuff re-tears was lower in patients undergoing early repair compared with those undergoing delayed repair in the trauma group (4.5% in 1 case vs. 33.3% in 6 cases, p = 0.033), whereas no statistical difference was noted in the non-trauma group (16.7% in 3 cases vs. 27.6% in 8 cases, p = 0.492) (Table 3; Fig. 4).
Postoperative follow-up of a 63-year-old patient with traumatic rotator cuff injury who underwent early repair, namely supraspinatus tendon repair and acromioplasty. A and B T2-weighted coronal magnetic resonance imaging illustrating the satisfactory positioning of the two anchors, partial healing of the supraspinatus tendon, and unresolved edema of the greater tuberosity of the humerus
Discussion
To the best of our knowledge, this is the first study to investigate differences in early and delayed repair among Chinese patients with both traumatic and non-traumatic RCI. Our findings exposed that surgical repair of traumatic RCI within 3 months post-injury yielded superior functional outcomes and patient satisfaction compared to repairs performed 3 months after injury. However, in the non-trauma group, early repair only demonstrated a significant improvement in external rotation of the shoulder compared to delayed repair, with no significant differences observed in other functional outcomes. The results of this study support our initial hypothesis that early repair of traumatic RCI results in better ROM and functional scores compared to delayed repair.
Arthroscopic rotator cuff repair has shown effectiveness in alleviating patient pain and improving function. A study examining [21] 188 arthroscopic repairs of isolated supraspinatus tendon tears reported that tendon healing alone did not fully account for subjective satisfaction among patients during follow-up beyond 1 year. This result may be ascribed to patients having high expectations regarding pain relief and functional improvement. Notably, in this study, patients in the trauma group who underwent early repair had superior outcomes, reporting higher subjective satisfaction scores on postoperative VAS, ASES, Constant, and UCLA scores compared to those undergoing delayed repair. Gutman [22] et al. examined 206 (150 males and 56 females) patients with traumatic rotator cuff tear repairs with a minimum of 24 months of postoperative follow-up. Interestingly, patients who underwent surgery within 4 months of injury achieved better functional recovery, consistent with the results of the present study. It is worthwhile emphasizing that Gutman et al. reported that patients who underwent repair within 2 to 4 months after injury were more likely to be young and had superior outcomes following tendon tear repair; this demographic difference may have influenced clinical outcomes post-surgery. Conversely, no statistical difference in age was observed between patients in the trauma and non-trauma groups who underwent early and delayed repair herein. Despite the diverse mechanisms underlying shoulder injuries, traumatic cases typically involve direct external forces acting on the shoulder joint, as evidenced by their greater tear size and pain scores [18]. Of note, a novel scoring system for assessing rotator cuff healing, pioneered by Kwon et al., implies that tear size is correlated with tendon involvement, with larger tear areas associated with higher postoperative re-tear rates [23]. Furthermore, a study undertaken by Lähteenmäki et al. suggested [24] that repairing a rotator cuff tear before it exceeds 2 cm² is associated with improved postoperative clinical outcomes, with a defined threshold of 2.5 cm². In the current study, patients in the trauma group undergoing early repair had tear areas of 4.14 ± 1.19 cm², while those undergoing delayed repair had tear areas of 3.86 ± 0.81 cm². Despite the higher tear size in patients undergoing early repair, their postoperative VAS, Constant, ASES, and UCLA scores were better than patients undergoing delayed repair. The improved postoperative functional scores may hold significant implications, considering the patients’ preoperative tear area and muscle degenerative changes.
Numerous studies have established [24, 25] the benefits of early surgical repair, particularly for traumatic tears, aiming to mitigate the detrimental effects of muscle atrophy and fat infiltration on the repair process. However, tailored treatments should be applied to each patient, taking into account their clinical conditions and comorbidities. While many physicians understand the difference between traumatic and non-traumatic causes of rotator cuff injuries, this disparity may not be well understood by novice rehabilitation therapists and patients. Consequently, it is crucial for healthcare professionals to identify the optimal timing for rotator cuff repair surgery. Following a traumatic event, some patients with traumatic injuries may postpone surgical intervention due to financial constraints or personal medical preferences, instead opting for conservative treatment. On the one hand, prolonged conservative management often results in unsatisfactory outcomes and delays the optimal window for repair. On the other hand, non-surgical protocols combined with appropriate physical therapy lead to better outcomes for patients with non-traumatic injuries [26, 27].
Studies focusing on the outcomes of non-operative treatment of non-traumatic rotator cuff injuries have reported conflicting results. Lambers Heerspink [28] et al. observed no difference in functional outcomes after 1 year of follow-up in a group of patients with non-traumatic rotator cuff injury who received either conservative treatment or surgical repair. In addition, Kuhn [7] et al. investigated 452 patients with nontraumatic rotator cuff injuries who were initially treated conservatively and showed satisfactory scoring results at weeks 6 and 12, yet a proportion (26%) of patients opted for surgery within 2 years of follow-up. Herein, patients in the non-trauma group typically experienced shoulder-associated symptoms for an average of 12.3 months before undergoing surgery, which was markedly longer than the trauma group. Most of these patients underwent an average of 3 months of conservative treatment before opting for surgery. Surprisingly, early surgical repair in the non-trauma group did not yield superior outcomes in terms of pain relief and functional improvement compared to delayed repair.
Tear size and chronicity, number of implicated tendons, level of fatty infiltration, and muscle atrophy have all been identified as significant indicators of functional outcome and repair integrity. Tear etiology (traumatic vs. atraumatic) may play a pivotal role in predicting functional outcomes. Moreover, patients with non-traumatic RCI are at a higher risk of developing muscle atrophy and fatty infiltration, which substantially influence post-repair functional outcomes. Earlier studies have uncovered that [25, 29] the average time from the onset of shoulder pain to surgical intervention in patients undergoing delayed repair in the non-trauma group was 13 months. However, muscular degradations span over the years. This prolonged timeframe is potentially a factor contributing to the lack of statistical differences in postoperative functional outcomes between patients undergoing early repair and delayed repair in the non-trauma group. An increasing number of experienced physicians recommend a trial of conservative treatment before considering surgical intervention for non-traumatic rotator cuff injuries. Additionally, they recommend surgical repair for cases not successfully managed by non-surgical approaches. Therefore, careful consideration of both non-operative and surgical treatment options is essential in the management of non-traumatic rotator cuff injuries.
Nevertheless, this study has several limitations that merit acknowledgment. To begin, this was a retrospective cohort study, and the findings were only able to establish correlation but not causation. Secondly, the mean age of traumatic injury patients included in this study was 59 years, and the possibility of asymptomatic degenerative tears being present before the trauma cannot be excluded, considering that the prevalence of asymptomatic tears is markedly higher in older adults than in younger adults [1, 5]. Thirdly, despite our rigorous screening of patients who experienced a traumatic event and our strict definition of “traumatic rotator cuff injury,” the subjective nature of trauma based on the mechanism of injury might have introduced potential bias. Fourthly, our study sample size was small, and the absence of preliminary power calculation; therefore, further studies with a large sample size are needed to confirm these results. Lastly, the follow-up period was relatively short, warranting further long-term assessments to evaluate the clinical outcomes of repair at various time points for both traumatic and non-traumatic rotator cuff injuries.
Conclusions
In this study, early repair of traumatic rotator cuff injuries demonstrated superior outcomes in restoring range of motion, attenuating pain, and reducing the risk of postoperative re-tear compared to delayed repair. Therefore, early arthroscopic surgical repair remains the preferred approach for managing traumatic rotator cuff injuries. Conversely, for non-traumatic rotator cuff injuries, premature repair did not lead to improved clinical outcomes in postoperative joint function and complications. Consequently, early physiotherapy and non-surgical interventions are recommended as initial treatment approaches for patients with non-traumatic rotator cuff injuries. Taken together, these findings contribute to preoperative consultations regarding patient expectations and functional outcomes, considering tear etiology and timing of surgery, thereby enhancing our understanding of surgical outcomes.
Data availability
No datasets were generated or analysed during the current study.
References
Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604.
Keener JD, Patterson BM, Orvets N, Chamberlain AM. Degenerative rotator cuff tears: Refining Surgical indications based on natural History Data. J Am Acad Orthop Surg. 2019;27(5):156–65.
Long Z, Nakagawa K, Wang Z, Amadio PC, Zhao C, Gingery A. Age-related cellular and microstructural changes in the rotator cuff enthesis. J Orthop Res. 2022;40(8):1883–95.
Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elb Surg. 2010;19(1):116–20.
Ruderman L, Leinroth A, Rueckert H, Tabarestani T, Baker R, Levin J, Cook CE, Klifto CS, Hilton MJ, Anakwenze O. Histologic differences in human rotator cuff muscle based on tear characteristics. J Bone Joint Surg Am. 2022;104(13):1148–56.
Boorman RS, More KD, Hollinshead RM, Wiley JP, Brett K, Mohtadi NG, Nelson AA, Lo IK, Bryant D. The rotator cuff quality-of-life index predicts the outcome of nonoperative treatment of patients with a chronic rotator cuff tear. J Bone Joint Surg Am. 2014;96(22):1883–8.
Kuhn JE, Dunn WR, Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elb Surg. 2013;22(10):1371–9.
Ryösä A, Laimi K, Äärimaa V, Lehtimäki K, Kukkonen J, Saltychev M. Surgery or conservative treatment for rotator cuff tear: a meta-analysis. Disabil Rehabil. 2017;39(14):1357–63.
Ainsworth R, Lewis JS. Exercise therapy for the conservative management of full thickness tears of the rotator cuff: a systematic review. Br J Sports Med. 2007;41(4):200–10.
Franceschi F, Papalia R, Vasta S, Leonardi F, Maffulli N, Denaro V. Surgical management of irreparable rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):494–501.
Henry P, Wasserstein D, Park S, Dwyer T, Chahal J, Slobogean G, Schemitsch E. Arthroscopic repair for chronic massive rotator cuff tears: a systematic review. Arthroscopy. 2015;31(12):2472–80.
Ghodadra NS, Provencher MT, Verma NN, Wilk KE, Romeo AA. Open, mini-open, and all-arthroscopic rotator cuff repair surgery: indications and implications for rehabilitation. J Orthop Sports Phys Ther. 2009;39(2):81–9.
Dang A, Davies M. Rotator Cuff Disease: Treatment options and considerations. Sports Med Arthrosc Rev. 2018;26(3):129–33.
Hein J, Reilly JM, Chae J, Maerz T, Anderson K. Retear Rates after arthroscopic Single-Row, Double-Row, and suture Bridge Rotator Cuff Repair at a Minimum of 1 year of imaging Follow-up: a systematic review. Arthroscopy. 2015;31(11):2274–81.
Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, Kinoshita M. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011;39(10):2091–8.
Hantes ME, Ono Y, Raoulis VA, Doxariotis N, Venouziou A, Zibis A, Vlychou M. Arthroscopic single-row Versus double-row suture bridge technique for Rotator Cuff tears in patients younger than 55 years: a prospective comparative study. Am J Sports Med. 2018;46(1):116–21.
Abechain JJK, Godinho GG, Matsunaga FT, Netto NA, Daou JP, Tamaoki MJS. Functional outcomes of traumatic and non-traumatic rotator cuff tears after arthroscopic repair. World J Orthop. 2017;8(8):631–7.
Paul S, Yadav AK, Goyal T. Comparison of tear characteristics, outcome parameters and healing in traumatic and non-traumatic rotator cuff tear: a prospective cohort study. Musculoskelet Surg. 2022;106(4):433–40.
Duncan NS, Booker SJ, Gooding BW, Geoghegan J, Wallace WA, Manning PA. Surgery within 6 months of an acute rotator cuff tear significantly improves outcome. J Shoulder Elb Surg. 2015;24(12):1876–80.
Björnsson HC, Norlin R, Johansson K, Adolfsson LE. The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears: structural and clinical outcomes after repair of 42 shoulders. Acta Orthop. 2011;82(2):187–92.
Nabergoj M, Bagheri N, Bonnevialle N, et al. Arthroscopic rotator cuff repair: is healing enough? Orthop Traumatol Surg Res. 2021;107(8S):103100.
Gutman MJ, Joyce CD, Patel MS, Kirsch JM, Gutman BS, Abboud JA, Namdari S, Ramsey ML. Early repair of traumatic rotator cuff tears improves functional outcomes. J Shoulder Elb Surg. 2021;30(11):2475–83.
Kwon J, Kim SH, Lee YH, Kim TI, Oh JH. The Rotator Cuff Healing Index: a New Scoring System to Predict Rotator Cuff Healing after Surgical Repair. Am J Sports Med. 2019;47(1):173–80.
Lähteenmäki HE, Virolainen P, Hiltunen A, Heikkilä J, Nelimarkka OI. Results of early operative treatment of rotator cuff tears with acute symptoms. J Shoulder Elb Surg. 2006;15(2):148–53.
Petersen SA, Murphy TP. The timing of rotator cuff repair for the restoration of function. J Shoulder Elb Surg. 2011;20(1):62–8.
Narvani AA, Imam MA, Godenèche A, Calvo E, Corbett S, Wallace AL, Itoi E. Degenerative rotator cuff tear, repair or not repair? A review of current evidence. Ann R Coll Surg Engl. 2020;102(4):248–55.
Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T, Aärimaa V. Treatment of non-traumatic rotator cuff tears: a randomised controlled trial with one-year clinical results. Bone Joint J. 2014;96–B(1):75–81.
Lambers Heerspink FO, van Raay JJ, Koorevaar RC, et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elb Surg. 2015;24(8):1274–81.
Godshaw BM, Hughes JD, Boden SA, Lin A, Lesniak BP. Comparison of functional outcomes after arthroscopic rotator cuff repair between patients with traumatic and atraumatic tears. Orthop J Sports Med. 2022;10(10):23259671221126551.
Acknowledgements
Not applicable.
Funding
This project was supported by USTC Research Funds of the Double First-Class Initiative (grant number YD9110002070).
Author information
Authors and Affiliations
Contributions
Aixin Liu and Baorui Zhang were responsible for statistical analysis and manuscript writing. Tong Lai, Mingxing Wang, and Gongyi Wu were involved in editing and revising the manuscript. Tao Zhang and Shilin Liu were responsible for the study design and the critical revision of the manuscript. All authors have contributed to and have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This retrospective study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Lu’an Hospital of Traditional Chinese Medicine affiliated of Anhui University of Traditional Chinese Medicine (protocol code LASZYY-LL-2024006).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, A., Zhang, B., Lai, T. et al. Comparison of functional outcomes following early and delayed arthroscopic repair for traumatic and non-traumatic rotator cuff injuries. J Orthop Surg Res 19, 368 (2024). https://doi.org/10.1186/s13018-024-04858-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04858-x