Abstract
Background
To compare the clinical and radiological outcomes of monoplanar screws (MSs) versus hybrid fixed axial and polyaxial screws (HSs) in percutaneous short-segment intermediate screw fixation (PSISF) for traumatic thoracolumbar burst fractures (TTBFs) in patients without neurologic impairment.
Methods
A consecutive series of 100 patients with single-segment TTBFs and no neurologic impairment who underwent PSISF with 6 monoplanar screws (MS group) or correct were retrospectively enrolled. The demographic data, radiologic evaluation indicators, perioperative indicators and clinical assessment indicators were analysed between the MS group and HS group.
Results
The demographic data and perioperative indicators were not significantly different in the two groups (P > 0.05). The postoperative anterior vertebral height ratio (AVHR), kyphosis Cobb angle (KCA), vertebral wedge angle (VWA) and spinal canal encroachment rate (SCER) were significantly improved in both groups (*P < 0.05). The MS group obtained better correction than the HS group in terms of improvement in the AVHR, KCA and VWA after surgery (*P < 0.05). At the last follow-up, the MS group had less correction loss of AVHR, KCA and VWA (*P < 0.05). The MS group presented greater improvement in the SCER at the last follow-up (*P < 0.05). The visual analogue scale (VAS) score and Oswestry Disability Index (ODI) score of all patients were significantly better postoperatively than those preoperatively (*P < 0.05), and the scores collected at each follow-up visit did not differ significantly between the two groups (P > 0.05). In the MS group, no internal fixation failure was observed during the follow-up period, but, in the HS group, two cases of internal fixation failure were observed at the last follow-up (one case of rod loosening and one case of screw breakage).
Conclusions
Both MSs and HSs fixation are effective treatments for TTBFs and have comparable clinical outcomes. In contrast, MSs fixation can improve the correction effect, better improve the SCER, and further reduce correction loss as well as reduce the incidence of instrumentation failure. Therefore, MSs fixation might be a better option for treating TTBFs in patients without neurological deficits.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Traumatic spinal fracture accounts for approximately 5–14% of all fractures and is usually caused by high-energy violent injuries such as unintentional falls and traffic accidents [1,2,3,4,5]. A traumatic spinal fracture can compromise the stability of the spine, compress the spinal cord and cause spinal nerve damage [3, 5]. The thoracolumbar junction (T11–L2) is the area at which stress is concentrated, thereby making it prone to fractures, accounting for 71.69% of all traumatic spine fractures [2, 6]. In recent years, percutaneous short-segment intermediate screw fixation (PSISF) has been increasingly performed for the treatment of traumatic thoracolumbar burst fractures (TTBFs) [7,8,9]. PSISF for the treatment of TTBFs involves inserting screws in the fractured segment and two adjacent segments, forming a 6-screw structure [10]. Previous biomechanical studies have demonstrated that the 6-screw structure clearly increased the stiffness and stability of the internal fixation system during flexion‐extension and lateral bending compared with the traditional 4-screw construct [11, 12]. Similarly, clinical studies have shown that PSISF achieved superior correction and maintenance of the correction compared with percutaneous pedicle screw fixation (PPSF) with 4 screws [13,14,15].
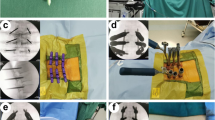
Since the PPSF technique was first reported by Magerl, several pedicle screws have been introduced in PPSF including fixed axial screw (Fig. 1c), polyaxial screw (Fig. 1d) and monoplanar screw (MS) (Fig. 1a) [16, 17]. Polyaxial screw is widely utilized in PSISF because of their convenience for rod insertion [18, 19]. Nevertheless, polyaxial screw fixation performed poor results in correcting deformities and maintaining reduction compared to the fixed axial screw and monoplanar screw [18,19,20]. Fixed axial screw helps improve rigidity due to their structural properties, which is more conducive for restoring the injured vertebral height and correcting kyphosis [21]. However, if the ipsilateral fixed axial screws are not highly aligned in PSISF, percutaneous insertion of the rod becomes difficult [22]. Recently, an innovative MS screw has been developed which combined the advantages of fixedaxial screw and polyaxial screw [18].
Three pedicle screws and the two new types of fixation methods. a MS can swivel freely in the coronal view and can be fixed in the sagittal view. b Three robust MSs can provide rigidity in the sagittal view and can smoothly accomplished installation of the connecting rod. c Fixed axial screw can be fixed in both the sagittal view and the coronal view. d Polyaxial screw can swivel freely in both the coronal view and the sagittal view. e Fixed axial screws of the upper and lower can provide firm fixation, and intermediate fixation with polyaxial screw is convenient for rod implantation
To better correct the kyphotic deformity, reduce the loss of reduction, and reserve the convenience of installing the connecting rod, some propose percutaneous MSs fixation of TTBFs [17, 18] (Fig. 1b). Some have suggested that hybrid fixed axial and polyaxial screws (HSs) fixation (Fig. 1e) may be a better option [23]. No relevant studies have reported whether there are differences between both treatments. The purpose of our study is designed to compare the clinical outcomes of MSs versus HSs fixation of TTBFs.
Methods
Demographics
From January 2017 to June 2021, a consecutive series of 100 patients with single-segment TTBFs without neurological deficits who underwent PSISF with 6 MSs (MS group) or hybrid 4 fixed axial screws and 2 polyaxial screws (HS group) were retrospectively enrolled. Sex, age, cause of injury, fracture level, AO Spine Injury Classification (AO classification) [24], Thoracolumbar Injury Classification and Severity Score (TLICS score) [25], Load Sharing Classification (LSC score) [26], number of spinal canal encroachment and time of last follow-up were recorded.
Inclusion criteria: (1) between 18 and 60 years of age; (2) with a single-segment vertebral fracture of the thoracolumbar spine involving T11-L2; (3) fresh traumatic fracture; (4) TLICS score greater than or equal to 4; (5) underwent all preoperative, postoperative and follow-up imaging examinations in our hospital; (6) intact pedicles of the injured vertebra; and (7) patients who signed informed consent forms.
Exclusion criteria: (1) time from trauma to surgery more than 14 days; (2) pathological fractures (including tuberculosis, primary or metastatic tumours, etc.); (3) infection; (4) prior spine surgery; (5) congenital spinal deformities; (6) osteoporosis; and (7) incomplete clinical data.
The study was reviewed and approved by the Ethics Committee of General Hospital of Central Theater Command ([2022]060-01) and was performed in conformity with the Declaration of Helsinki. Observational studies were reported using STROBE guidelines [27].
Surgical procedures
All operations were performed by the same team, and the chief surgeon was an experienced deputy chief physician in the same department. The patients were placed in the prone position on the Jackson surgical table, and the abdomen was suspended, the operating table was bent into a V shape, manual reduction was performed by applying firm pressure on the spinous process adjacent to the injured vertebra. After marking the puncture points approximately 1.5 cm lateral to the markers positioned at the pedicles of the injured vertebra and two adjacent vertebrae, 6 Jamshidi needles were inserted into the corresponding pedicle with proper orientation and to the appropriate depth. After successful puncture, the needle core was withdrawn. After the long guide wire was placed into the anterior medial third of the vertebral body, the screw was implanted. In the MS group, 6 MSs (Shanghai SANYOU, China) were implanted parallel to the upper endplate of the injured vertebra and two adjacent vertebrae. In the HS group, 4 fixed axial screws (Shandong WEGAO, China) were implanted parallel to the upper endplate of the adjacent vertebrae of the injured vertebra, and 2 intermediate short polyaxial screws (Shandong WEGAO, China) were implanted parallel to the pedicle of the injured vertebrae. The connecting rod, with an appropriate length and radians, was inserted after insertion of all 6 screws. In the MS group, during the distraction process, the intermediate MSs were exerted an upward force on the upper endplate of the injured vertebra, aiming to better restore the anterior and middle columns. In the HS group, indirect reduction of the restoration of the anterior column of the injured vertebra by applying appropriate compression to the fixed axial screw-rod system at both ends. All pedicle screws were placed via a minimally invasive percutaneous and inserted into the corresponding segment vertebral body. All above operations were conducted under the guidance of C-arm fluoroscopy.
Postoperative management and follow-up schedule
For all patients, functional exercises for both lower limbs were started 1 day after surgery. They were encouraged to regularly ambulate 3 days after surgery. All participants were followed up postoperatively for at least 12 months.
Radiologic evaluation and clinical assessment
Radiologic evaluation indicators, perioperative indicators, and clinical assessment indicators were recorded and assessed.
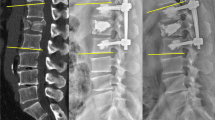
Radiologic evaluation indicators included the anterior vertebral height ratio (AVHR), kyphosis Cobb angle (KCA), vertebral wedge angle (VWA) and spinal canal encroachment rate (SCER). The AVHR, KCA and VWA were measured on lateral images of the thoracolumbar spine (Fig. 2a). The SCER was measured on CT images (Fig. 2b). Anteroposterior and lateral radiographs, as well as CT, were obtained for the thoracolumbar spine before surgery, at 1 week and 3 months after surgery, and during the final follow-up at our hospital for all patients. Additionally, MRI of the thoracolumbar spine were conducted before surgery and at 1 week after surgery for all patients. The effect of correction was compared and analysed in terms of AVHR, KCA, VWA and SCER. Changes in the corrective effect were evaluated on all lateral radiographs and CT of the thoracolumbar spine after the surgery.
Measurement of radiologic evaluation indicators. a AVHR = h2/ [(h1 + h3)/2] × 100%, the KCA was measured between the upper endplate of the adjacent superior vertebra of the injured vertebra and the lower endplate of the adjacent inferior vertebra of the injured vertebra, the VWA was measured between the upper endplate of the injured vertebra and the lower endplate of the injured vertebra. b SCER = w2/ [(w1 + w3)/2] × 100%
Perioperative indicators included the time from admission to surgery, operation time, intraoperative bleeding volume, time to ambulation after surgery and length of hospital stay.
Clinical assessment indicators included the visual analogue scale (VAS) score, Oswestry Disability Index (ODI) score and complications (spinal cord or nerve root injury, wound haematoma, infection, internal fixation failure, etc.). Pain from the lower back was evaluated using the VAS score and functional outcome was evaluated using the ODI score. The VAS score and ODI score were calculated preoperatively, 1 week and 3 months postoperatively and at the last follow-up. Complications, including intraoperative and postoperative complications, were recorded. Loosening, breakage and pulling out of internal fixation (including screw, rod and locking cap) were defined as failure.
All measured and evaluated data were performed by two experienced physicians in spine surgery respectively. The final values were determined as the average of the measurements performed by the two physicians.
Statistical analyses
All of the statistical analyses were conducted with SPSS 26.0 (IBM, New York, USA). The categorical variables that were reported as numbers were compared by using the χ2 test or Fisher’s exact test. The variables with continuous data were reported as the mean ± standard deviation. Comparisons between two groups were evaluated by independent sample t tests, and comparison of before–after changes in each group was using paired-samples t test. A P value < 0.05 indicated statistical significance.
Results
Demographic data
In the study, a total of 100 patients were recruited with an average age of 46.11 ± 12.3 years. Fifty-one patients underwent fixation with 6 MSs (MS group) and 49 patients underwent fixation with hybrid 4 fixed axial screws and 2 polyaxial screws (HS group). In terms of sex, age, cause of injury, fracture level, AO classification, TLICS score, LSC score, number of spinal canal encroachment and time of last follow-up were not statistically different between the MS group and the HS group (P > 0.05, Table 1).
Perioperative indicators
No statistically significant differences in the time from admission to surgery, operation time, intraoperative bleeding volume, time to ambulation after surgery or length of hospital stay were found between the MS and HS groups (P > 0.05, Table 2).
Radiologic and clinical outcomes
As shown in Table 3, no significant differences in the AVHR, KCA, VWA or SCER were found between the two groups preoperatively (P > 0.05). One week postoperatively, 3 months postoperatively and at the last follow-up, the AVHR, KCA, VWA and SCER were obviously improved in the two groups. A significant difference between the preoperative and postoperative values were found at every time point (*P < 0.05). The MS group had better correction in the AVHR, KCA and VWA than the HS group after surgery (*P < 0.05). During the follow-up period, correction loss of AVHR, KCA and VWA was found between two groups and correction loss was clearly observed in the HS group at the last follow-up (*P < 0.05). The MS group presented greater improvement in the SCER than the HS group at the last follow-up (*P < 0.05).
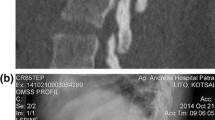
Compared to those preoperatively, the postoperative VAS and ODI scores were significantly improved in all the patients in both groups (*P < 0.05), and the scores collected at each follow-up visit did not differ significantly between the two groups (P > 0.05) (Table 4). In the HS group, two cases of internal fixation failure were observed at the last follow-up and the overall failure rate was 4.1%. There was 1 case of rod loosening that developed 13 months after surgery, and one case of screw breakage developed 12 months postoperatively. In two cases, good fracture healing and correction maintenance were found. After implant removal no more problems occurred. There were no severe complications such as spinal cord or nerve root injury, wound haematoma or infection, in either group. Typical case images of the MSs fixation were shown in (Fig. 3).
A 46-year-old female patient with L1 burst fracture was treated with MSs fixation. a–d Preoperative lumbar radiographs (a, b) and CT (c, d) demonstrated a L1 AO type A3 fracture with spinal canal encroachment. e MRI showed a fresh fracture of the L1 vertebrae. f–i One-week postoperative radiographs (f–g) and CT (h–i) showed satisfactory injury vertebral height restoration and kyphosis correction. j One-week postoperative MRI show the spinal canal encroachment decreased. k–l Radiography at the last follow-up at 12 months after surgery showed that the internal fixation systems were stable with good positioning and good morphology. m–o And CT showed that spinal canal encroachment was remarkably relieve
Discussion
The objective of surgical treatment of TTBFs is effective fixation with pedicle screws to restore the injured vertebral height, correct kyphosis, and prevent late-onset kyphosis of the spine and secondary nerve compression [28]. In a clinical setting, PSISF that can be used to provide effective support of the anterior, middle and posterior columns for the vertebral bodies has become one of the most commonly used surgical options for treating TTBFs in patients without neurological function deficits [29,30,31].
As PSISF requires 6-screw fixation, the insertion of longitudinal rods would become difficult if the 3 ipsilateral screws were not highly aligned, especially using fixed axial screws [22]. Thus, proper choice of pedicle screw appears to be critical for the treatment of TTBFs. There are several options of pedicle screws for PSISF, including fixed axial screw, polyaxial screw, and MS [32]. Polyaxial screw has been used widely in PSISF [33]. Benefiting from the well-orchestrated coupling device, polyaxial screw can increase the capacity of angular motion and offer convenience for rod implantation without increasing overmuch stress [17, 34]. However, polyaxial screw reduce the compression and bending strength in the sagittal plane, which results in insufficient restoration of vertebral height, inadequate correction of kyphotic and inadequate maintenance of rigid fixation [17, 18].
Percutaneous MSs and HSs fixation were proposed to solve the abovementioned problems of polyaxial screw [23, 35]. Because MS is fixed in the sagittal view and allows free swivelling in the coronal view, 6 MSs fixation do not compromise the rigidity in the sagittal view and allow smooth installation of the connecting rod [35]. Owing to fixed axial screw endows stronger leverage, HSs fixation can better improve the correction, stability of the instrumentations and buckling and compressive strengths than polyaxial screw fixation alone. The injured vertebra fixation with 2 polyaxial screws convenient for rod implantation [33, 34]. Whether there was a difference between the two in terms of specific clinical outcome was not reported. To compare the clinical outcomes of MSs versus HSs fixation for TTBFs, we conceived and designed this study.
In this study we observed that the AVHR, KCA, VWA and SCER were significantly improved in both groups immediately after surgery, which suggested that both MSs and HSs fixation are safe and effective approaches in the treatment of TTBFs. This is consistent with previous studies [23, 35, 36]. We also found that the MS group had better correction in terms of the AVHR, KCA and VWA after surgery. Although there were no significant differences in the short‐term postoperative outcomes, we found that the MS group had less correction loss in terms of the AVHR, KCA and VWA and greater improvement in the SCER than the HS group at the last follow-up. We contemplated that the reasons were related to the following factors. In the MS group, one is that MS had strong strength in the sagittal plane to achieve effective reduction, immobilization, and stabilization, which thereby ensured long-term stability and potentially decreased the spinal canal encroachment. The other is that intermediate fixation with MS that were inserted parallel to the upper endplate of the injured vertebra can circumvent the anterior vertebral fracture regions and use relatively longer screws, allowing better restoration of the anterior vertebral height and the upper endplate of the injured vertebra. Similarly, a clinical study by Huang et al. [37] indicated that MSs fixation achieved better correction effect and less correction loss than polyaxial screw fixation alone. According to Ye et al. [38] MS probably a superior option to reduce the incidence of degeneration of the injured vertebral adjacent segment than fixed axial screw.
Additionally, no significant differences in any of the perioperative indicators were found between the two groups. Our results showed that both MSs and HSs fixation are work well, highly efficient and less traumatic. Postoperative VAS and ODI scores of all patients had improved obviously, indicating a significant decrease in pain. The pain scores were further decrease between the two groups during an extended follow-up; the VAS and ODI scores were no significant difference in both group at the last follow-up. This suggests that the two surgical methods showed favourable clinical results. Furthermore, two cases of instrumentation failure were observed at the last follow-up in the HS group and not in the MS group. This indicates that the MSs fixation system could sustain higher loads than the HSs fixation system and have advantages in the prevention of internal fixation failure. Yin et al. [39] observed that HSs fixation can cause more correction loss but no instrumentation failure events. According to the study by Liu et al. [19], fixed axial screw was implanted at the lowest segment led to a greater predisposition to adjacent segmental degeneration, particularly at the one level above the injured vertebra.
To the best of our knowledge, this is the first study to compare MSs versus HSs fixation for the treatment of TTBFs. Our study provides evidence that both MSs and HSs fixation can be used for treating TTBFs. MSs fixation can achieve better correct results, less correction loss, greater improvement of the SCER and fewer instrumentation failures.
Limitations of this study
There were several limitations of this study. First, its retrospective design and lack of randomization could potentially lead to selection bias. Therefore, our findings should be confirmed in additional prospective studies. Second, the study sample size was relatively small. Thus, multicentre relevant studies are needed. Third, we did not assess results of correction loss, functional outcome, and degeneration of adjacent segment of the injured vertebra after removing the internal fixation. As such, further research in this area is warranted.
Conclusions
Both MSs and HSs fixation are effective treatments for TTBFs and have comparable clinical outcomes. In contrast, MSs fixation can improve the correction effect, better improve the SCER, and further reduce correction loss as well as reduce the incidence of instrumentation failure. Therefore, MSs fixation might be a better option for treating TTBFs in patients without neurological deficits.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MS:
-
Monoplanar pedicle screw
- HSs:
-
Hybrid fixed axial and polyaxial pedicle screws
- PSISF:
-
Percutaneous short-segment intermediate screw fixation
- TTBFs:
-
Traumatic thoracolumbar burst fractures
- AVHR:
-
Anterior vertebral height ratio
- KCA:
-
Kyphosis Cobb angle
- VWA:
-
Vertebral wedge angle
- SCER:
-
Spinal canal encroachment rate
- VAS:
-
Visual analogue scale
- ODI:
-
Oswestry Disability Index
- PPSF:
-
Percutaneous pedicle screw fixation
- AO classification:
-
AO spine injury classification
- TLICS:
-
Thoracolumbar injury classification and severity
- LSC:
-
Load sharing classification
- ASIA:
-
American Spinal Injury Association
References
Liu P, Yao Y, Liu MY, Fan WL, Chao R, Wang ZG, Liu YC, Zhou JH, Zhao JH. Spinal trauma in mainland China from 2001 to 2007: an epidemiological study based on a nationwide database. Spine. 2012;37(15):1310–5.
Tian Y, Zhu Y, Yin B, Zhang F, Liu B, Chen W, Zhang Y. Age- and gender-specific clinical characteristics of acute adult spine fractures in China. Int Orthop. 2016;40(2):347–53.
den Ouden LP, Smits AJ, Stadhouder A, Feller R, Deunk J, Bloemers FW. Epidemiology of spinal fractures in a level one Trauma Center in the Netherlands: a 10 years review. Spine. 2019;44(10):732–9.
Zileli M, Sharif S, Fornari M. Incidence and epidemiology of thoracolumbar spine fractures: WFNS spine committee recommendations. Neurospine. 2021;18(4):704–12.
Bigdon SF, Saldarriaga Y, Oswald K, Muller M, Deml MC, Benneker LM, Albers CE. Epidemiologic analysis of 8000 acute vertebral fractures: evolution of treatment and complications at 10-year follow-up. J Orthop Surg Res. 2022;17(1):270.
Bruno AG, Burkhart K, Allaire B, Anderson DE, Bouxsein ML. Spinal loading patterns from biomechanical modeling explain the high incidence of vertebral fractures in the Thoracolumbar region. J Bone Miner Res. 2017;32(6):1282–90.
Cheng LM, Wang JJ, Zeng ZL, Zhu R, Yu Y, Li C, Wu ZR. Pedicle screw fixation for traumatic fractures of the thoracic and lumbar spine. Cochrane Db Syst Rev. 2013;5:CD9073.
Dahdaleh NS, Smith ZA, Hitchon PW. Percutaneous pedicle screw fixation for thoracolumbar fractures. Neurosurg Clin N Am. 2014;25(2):337–46.
Trungu S, Ricciardi L, Forcato S, Piazza A, D’Andrea G, Polli FM, Cimatti M, Frati A, Miscusi M, Raco A. Percutaneous pedicle screw fixation without arthrodesis of 368 thoracolumbar fractures: long-term clinical and radiological outcomes in a single institution. Eur Spine J. 2023;32(1):75–83.
Norton RP, Milne EL, Kaimrajh DN, Eismont FJ, Latta LL, Williams SK. Biomechanical analysis of four- versus six-screw constructs for short-segment pedicle screw and rod instrumentation of unstable thoracolumbar fractures. Spine J. 2014;14(8):1734–9.
Baaj AA, Reyes PM, Yaqoobi AS, Uribe JS, Vale FL, Theodore N, Sonntag VK, Crawford NR. Biomechanical advantage of the index-level pedicle screw in unstable thoracolumbar junction fractures. J Neurosurg Spine. 2011;14(2):192–7.
Bartanusz V, Harris J, Moldavsky M, Cai Y, Bucklen B. Short segment spinal instrumentation with index vertebra pedicle screw placement for pathologies involving the anterior and middle vertebral column is as effective as long segment stabilization with cage reconstruction: a biomechanical study. Spine. 2015;40(22):1729–36.
Sun C, Guan G, Liu X, Zhang H, Wang B. Comparison of short-segment pedicle fixation with versus without inclusion of the fracture level in the treatment of mild thoracolumbar burst fractures. Int J Surg. 2016;36(Pt A):352–7.
Deng L, Zhang J, Zhou Q, Zheng Y, Hua X, Hu X, Liu H, Qian Z. Effect of the intermediate pedicle screws and their insertion depth on sagittal balance and functional outcomes of lumbar fracture. Front Surg. 2022;9:905946.
Luo ZW, Liao WJ, Sun BL, Wu JB, Zhang N, Zhang Y, Huang SH, Liu ZL, Zhang ZH, Liu JM. Short-segment fixation and transpedicular bone grafting for the treatment of thoracolumbar spine fracture. Front Surg. 2022;9:1039100.
Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat. 1984;189:125–41.
Schroerlucke SR, Steklov N, Mundis GJ, Marino JF, Akbarnia BA, Eastlack RK. How does a novel monoplanar pedicle screw perform biomechanically relative to monoaxial and polyaxial designs? Clin Orthop Relat. 2014;472(9):2826–32.
Ye B, Yan M, Zhu H, Duan W, Hu X, Ye Z, Luo Z. Novel screw head design of pedicle screw for reducing the correction loss in the patients with thoracolumbar vertebral fractures: a biomechanical study. Spine. 2017;42(7):E379–84.
Liu H, Wang H, Liu J, Li C, Zhou Y, Xiang L. Biomechanical comparison of posterior intermediate screw fixation techniques with hybrid monoaxial and polyaxial pedicle screws in the treatment of thoracolumbar burst fracture: a finite element study. J Orthop Surg Res. 2019;14(1):122.
Kubosch D, Kubosch EJ, Gueorguiev B, Zderic I, Windolf M, Izadpanah K, Sudkamp NP, Strohm PC. Biomechanical investigation of a minimally invasive posterior spine stabilization system in comparison to the Universal Spinal System (USS). Bmc Musculoskel Dis. 2016;17:134.
Yao W, Zhou T, Huang K, Dai M, Mo F, Xu J, Cao Z, Lai Q, Xie B, Guo R, Zhang B. A comparison of monoaxial pedicle screw versus polyaxial pedicle screw in short-segment posterior fixation for the treatment of thoracolumbar fractured vertebra. Ann Transl Med. 2021;9(8):669.
Chung WH, Eu WC, Chiu CK, Chan C, Kwan MK. Minimally invasive reduction of thoracolumbar burst fracture using monoaxial percutaneous pedicle screws: surgical technique and report of radiological outcome. J Orthop Surg-Hong K. 2020;28(1):615549265.
Wang H, Zhao Y, Mo Z, Han J, Chen Y, Yu H, Wang Q, Liu J, Li C, Zhou Y, Xiang L. Comparison of short-segment monoaxial and polyaxial pedicle screw fixation combined with intermediate screws in traumatic thoracolumbar fractures: a finite element study and clinical radiographic review. Clinics. 2017;72(10):609–17.
Reinhold M, Audige L, Schnake KJ, Bellabarba C, Dai LY, Oner FC. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J. 2013;22(10):2184–201.
Vaccaro AR, Lehman RJ, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG, Fisher C, Zeiller SC, Anderson DG, Bono CM, Stock GH, Brown AK, Kuklo T, Oner FC. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30(20):2325–33.
McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine. 1994;19(15):1741–4.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
Sharif S, Shaikh Y, Yaman O, Zileli M. Surgical techniques for thoracolumbar spine fractures: WFNS spine committee recommendations. Neurospine. 2021;18(4):667–80.
Wood KB, Li W, Lebl DR, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014;14(1):145–64.
Narain AS, Hijji FY, Duhancioglu G, Haws BE, Khechen B, Manning BT, Colman MW, Singh K. Patient perceptions of minimally invasive versus open spine surgery. Clin Spine Surg. 2018;31(3):E184–92.
Yang M, Zhao Q, Hao D, Chang Z, Liu S, Yin X. Comparison of clinical results between novel percutaneous pedicle screw and traditional open pedicle screw fixation for thoracolumbar fractures without neurological deficit. Int Orthop. 2019;43(7):1749–54.
Li J, Zhang LC, Li J, Zhang H, Zhao JX, Zhang W. A hybrid uniplanar pedicle screw system with a new intermediate screw for minimally invasive spinal fixation: a finite element analysis. Biomed Res Int. 2020;2020:5497030.
Shim JH, Seo EM. Efficacy and radiographic analysis of minimally invasive posterior mono-axial pedicle screw fixation in treating thoracolumbar burst fractures. J Clin Med. 2022;11:3.
Wang X, Aubin CE, Crandall D, Labelle H. Biomechanical comparison of force levels in spinal instrumentation using monoaxial versus multi degree of freedom postloading pedicle screws. Spine. 2011;36(2):E95–104.
Cao S, Zhang YB, Tao XS, Li Y, Xuan T, Yu RZ. Clinical study on the treatment of thoracolumbar fractures with single plane screw percutaneous internal fixation. Eur Rev Med Pharmacol. 2022;26(24):9187–94.
Claireaux HA, Searle HK, Parsons NR, Griffin XL. Interventions for treating fractures of the distal femur in adults. Cochrane Db Syst Rev. 2022;10(10):CD10606.
Huang L, Xiong C, Guo Z, Yu Q, Xu F, Kang H. Comparison of monoplanar and polyaxial screw fixation systems in percutaneous intermediate fixation for thoracolumbar fractures. Bmc Musculoskel Dis. 2022;23(1):172.
Ye B, Ye Z, Yan M, Huang P, Tu Z, Wang Z, Luo Z, Hu X. Effection of monoplanar pedicle screw on facet joint degeneration in thoracolumbar vertebral fractures. Bmc Musculoskel Dis. 2022;23(1):407.
Yin N, Du L, Pan M, Xue F, Shen Y, Ding L. Minimally invasive technique of monoaxial percutaneous screws and instrumentational maneuvers in thoracolumbar and lumbar fractures. Injury. 2022;53(12):4028–32.
Funding
We were received following financial support for the research, authorship, and publication of this article: This work was supported by the Medical Youth Top Talent Project of Hubei Province (No. [2019]48#), the Training Plan for Young and Middle-Aged Medical Backbone Talents in Wuhan (No. [2017]51#) and the Health Commission of Hubei Province Scientific Research Project (No. WJ2023Q091).
Author information
Authors and Affiliations
Contributions
HK and LH designed the study protocol. YH and GZ collected and analysed the clinical data of patients. YH and JM wrote the first draft of the manuscript. HK and LH provided revision for intellectual content and final approval. The authors read and approved the final manuscript of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study has been reviewed and approved by the Ethics Committee of General Hospital of Central Theater Command ([2022]060-01) and was performed in conformity with the Declaration of Helsinki. All patients signed a written informed consent.
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
We declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Han, Y., Ma, J., Zhang, G. et al. Percutaneous monoplanar screws versus hybrid fixed axial and polyaxial screws in intermediate screw fixation for traumatic thoracolumbar burst fractures: a case–control study. J Orthop Surg Res 19, 85 (2024). https://doi.org/10.1186/s13018-024-04547-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04547-9