Abstract
Trp3 allele in COL9A3 gene has been widely studied in populations with intervertebral disc disease. We identified a novel pathogenic variant in COL9A3 gene in a pedigree with multiple lumbar disc herniation (LDH). The proband was a 14-year-old boy who developed LDH at the L4/5 and L5/S1 spinal segments. His father, paternal aunt and grandfather were diagnosed with LDH at an age of 35, 30 and 23, respectively. By applying whole exome sequencing, a heterozygous missense variant (c.1150C > T, p.Arg384Trp) in COL9A3 was identified. According to the ACMG guidelines, this variant is predicted to be pathogenic. In addition, prediction tools found COL9A3 protein of this variant a reduced stability, some changed charge properties, and an altered spatial conformation. Findings expanded the mutational spectrum of LDH and contributed to the understanding of COL9A3 in the pathogenesis of LDH.
Similar content being viewed by others
Introduction
Lumbar disc herniation (LDH) is a common lumbar spinal disorder that leads to back and leg pain [1]. Reportedly, the incidence rate of LDH is 1–3% in general populations, adding heavy socio-economical burdens in communities [2]. Etiological studies revealed that LDH is a genetically predominant disorder [3]. A number of genes related to disc structural components, inflammatory factors, and matrix remodelling proteases have been found to be associated with the occurrence of LDH [4, 5]. For example, COL9A3 gene (Collagen type IX α3) has been repeatedly identified in different populations [6].
Collagen IX is a heterotrimeric protein encoded by COL9A1, COL9A2, and COL9A3 genes [7]. It serves as an organizing bridge, crosslinking collagens and non-collagenous components in articular cartilage and disc extracellular matrix (ECM) [8]. COL9A3 gene locates in chromosome 20q13.3 and encodes the α3 (IX) chain of collagen IX, which is a component of nucleus pulposus (NP) [9]. An early study of COL9A3 on disc diseases found that patients with the Trp3 (tryptophan) allele, also known as c.307C > T, p.Arg103Trp (rs61734651), had 2.7-fold higher risks of being diagnosed with lumbar spinal disease [10]. The minor allele frequency (MAF) of this single nucleotide polymorphism (SNP) was less than 0.05 in multiple datasets, GnomAD_exome (0.047), ExAC (0.048) and 1000 Genomes (0.022). Later on, while some independent studies demonstrated that Trp3 was statistically associated with the increased risk of lumbar disc diseases [11, 12], some others failed to relate it with disc diseases. For instance, the Trp3 allele in COL9A3 was found not clustered in lumbar disc degeneration [13], and the genotype of Trp3 allele was not related to clinical symptoms [14]. In addition, a number of meta-analysis studies did not observe the association between the COL9A3 Trp3 polymorphism and disc degeneration [15].
Since previous population-based case–control studies on COL9A3 gene have obtained inconsistent results [11,12,13,14,15], the underlying pathogenic mechanism of COL9A3 is not fully understood to date. Here, we reported a clinical pedigree of LDH with significant genetic characteristics and involvement of multiple lumbar discs. By applying whole exome sequencing (WES), we identified a novel pathogenic single nucleotide variant (SNV) of COL9A3. Our findings provide insights of understanding the function of COL9A3 in the pathogenesis of LDH.
Materials and methods
Case reports
The proband in this study was a 14-year-old boy who had low back pain and numbness in the lower extremities for half a year. The father, who accompanied for his son’s consultation, had radiculopathy in the left lower extremity for over two decades. The proband’s paternal aunt and grandfather were also clinically diagnosed with symptomatic LDH, with available MR images for confirmation. No other skeletal abnormality was observed in this family on radiological images. Written consent for each family member was obtained. This study was approved by the authors’ institutional ethic board.
Whole exome sequencing, variant identification and validation
After blood sample collection, genomic DNA of the proband, his father, paternal aunt and grandfather were extracted using the Blood Genome Column Medium Extraction Kit (Kangweishiji, China). The extracted DNA samples were subjected to quality controlling using Qubit 2.0 fluorimeter and electrophoresis with 0.8% agarose gel. Whole exome library was constructed using Roche Nimble Gen Seq EZ Exome Enrichment Kit V2.0 and Seq EZ Exome Enrichment Kit V2.0 capture probes (Roche, USA). High-throughput sequencing was performed on a Novaseq 6000 instrument (CHIGENE, Beijing, China) [16]. Quality control of whole exome sequencing data, variants calling and variant annotation was performed in the same institution.
Variant prioritization was performed based on guidelines released by ACMG (The American College of Medical Genetics and Genomics). First, co-segregation analysis was performed to exclude SNVs contradictory to the phenotypic data. SNVs were analysed under the assumptions of Mendelian dominant inheritance, recessive inheritance and sex-linked inheritance. Second, only rare variants with MAF < 1% were included for further selection [17, 18]. Candidate variants were selected based on the 1000 Genomes (https://www.internationalgenome.org), the Exome Sequencing Project (ESP), the Exome Aggregation Consortium (ExAC, http://exac.broadinstitute.org), Allele Frequency Aggregator (ALFA) and the Genome Aggregation Database (gnomAD, https://gnomad.broadinstitute.org). Third, synonymous variants and non-coding region variants were excluded. In silico prediction tools were applied to analyse pathogenicity of identified missense variants (Sorting Intolerant From Tolerant (SIFT), Polymorphism Phenotyping v2 (Polyphen2), Multivariate Analysis of Protein Polymorphism (MAPP), Mutation Taster, Mendelian Clinically Applicable Pathogenicity (M-CAP), Rare Exome Variant Ensemble Learner (REVEL) and Combined Annotation Dependent Depletion (CADD)) [19,20,21,22,23,24,25]. The deleterious effects of splice variants were predicted by MaxEntScan and dbscSNV [26, 27]. Next, evolutionary conservatism was analysed by phastCONS, phyloP and Genetic Evolutionary Rate Profiling (GERP) [28,29,30]. At last, protein function, GO (Gene ontology) annotations, tissue-specific distribution and existing literature were searched to evaluate the remaining SNVs.
Sanger sequencing was performed to validate the identified candidate variants. Sanger sequencing was performed with these primers:
Forward primer 5′-CAGGCGTCCCTGTGAGTATC-3′,
Reverse primer 5′-CATCAAGGCAACCAAATGCCA-3′.
The RefSeq accession numbers of the transcript and the corresponding protein isoform of COL9A3 we used for mutation nomenclature were NM_001853.4 and NP_001844.3, respectively.
Results
Clinical characterization of the pedigree with multiple lumbar disc herniation
The proband (height 1.65 m, weight 55.6 kg) is a 14-year-old Chinese boy suffering from low back pain and numbness in the lower limbs for 6 months before consultation. Magnetic resonance (MR) imaging revealed LDH at L4/5 and L5/S1 spinal segments (Fig. 1A). Growth and development of the proband were normal in adolescence. The proband did not experience waist trauma or excessive physical labour within 6 months before the onset of clinical symptoms. Blood biochemistry measurements and radiographs of limbs did not present any abnormality on the proband. A follow-up investigation of the LDH-related clinical symptoms and radiographs was carried out on the proband’s immediate family members. The proband’s father, who suffered from left lower limb radiculopathy for decades, had L3/4 and L4/5 LDH based on his lumbar spine MR images (Fig. 1B). The proband’s father, paternal aunt and grandfather had back pain and radicular leg pain, which were consistent with MR findings. They were clinically diagnosed with LDH at an age of 35, 30 and 23, respectively (Fig. 1C). None of them reported a history of waist injury before the onset of LDH‐related symptoms nor any other abnormality in the musculoskeletal system, except for the proband’s grandfather, who had degenerative kyphosis after 60 years old.
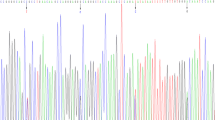
Magnetic resonance (MR) characteristics, pedigree chart and sequencing results of the proband and family members. A MR imaging of the proband: disc herniation at L4/5 and L5/S1 spinal segments. B MR imaging of the proband’s father: disc herniation at L3/4 and L4/5 spinal segments. C Pedigree chart: the proband’s paternal aunt and grandfather were diagnosed with lumbar disc herniation at an age of 30 and 23, respectively. D Summary of exome sequencing of the pedigree: the identified SNV (c.1150C > T, p.Arg384Trp) is located at COL9A3, a gene encoding one of the three alpha chains of type IX collagen. E Sanger sequencing: the heterozygous COL9A3 missense variant (c.1150C > T, p.Arg384Trp) was confirmed
Identification of a novel COL9A3 missense variant in the LDH family
We performed WES from four members (proband III-I, affected father II-2 and paternal aunt II-1, and unaffected mother II-3) to identify the candidate gene for the phenotypic manifestation of LDH. The work flow is summarized in Fig. 1D. A total of 3624 SNVs were identified after exclusion of non-genic and polymorphic variants. SNVs which did not co-segregate with the phenotype and were more than 1% frequency in the public genomes databases were excluded. Under the assumption of Mendelian dominant inheritance, 179 SNVs were identified. Synonymous variants and variants in non-coding region were then excluded, resulting in 69 SNVs. Besides, several in silico prediction tools invariably predicted that seven of the SNVs might cause damage to the protein, and no SNV near splice site had deleterious effects on the protein. In view of the protein function, GO annotations, tissue-specific distribution and the facts in published literatures, a novel heterozygous missense variant (c.1150C > T, p.Arg384Trp) in COL9A3 was identified, and further confirmed by Sanger sequencing (Fig. 1E).
The MAF of this SNP was less than 0.01 in different databases, ESP (0.00), 1000 Genomes (0.00), ALFA (0.00), GnomAD_exome (0.00004) and ExAC (0.00003). This variant was predicted to be pathogenic by in silico prediction tools, Provean (3.16), SIFT (0.005), Polyphen2_HDIV (1.0), MutationTaster (0.999494), M-CAP (0.705) and REVEL (0.725). In addition, with a CADD score > 20, this variant was also evaluated to be deleterious in GERP, phyloP and phastCons software. According to the variant interpretation guideline of ACMG (PM2, PP1, PP2, PP3 and PP4), this variant (c.1150C > T) was classified as “likely pathogenic” variant [31].
Change of charge properties and instability of COL9A3 protein with p.Arg384Trp variant
The p.Arg384Trp variant is situated within the collagenous domain, resulting in the substitution of arginine with tryptophan in amino acid sequence (Fig. 2A). Protein sequence alignment revealed that this locus is highly conserved among common species (Fig. 2B). Furthermore, the impacts of the p.Arg384Trp variant on the structure, function, and stability of COL9A3 were analysed using Swiss-Model (Fig. 2C) [32,33,34]. According to the prediction, the variant at this site changed the charge property and hydrophilicity of COL9A3 protein due to the substitution of arginine (Basic amino acid) with tryptophan (Aromatic hydrophobic amino acid). In addition, the prediction result in I-Mutant2.0 revealed a decreased stability of COL9A3 protein (Fig. 2D) [35].
An illustration of COL9A3 protein structure, Pathogenic variants, Sequence alignment among multiple species and Prediction results of COL9A3 missense variant (c.1150C > T, p.Arg384Trp). A The identified COL9A3 variant (c.1150C > T, p.Arg384Trp, Red) locates within the third collagenous region, resulting in the substitution of arginine (Arg) with tryptophan (Trp) in the amino acid sequence. Previously identified variant (p.Arg103Trp) were marked in black. B Multiple species sequence alignment using MEGA11 software shows that this variant is highly conserved among common species. C Protein structure predicted by Swiss-Model reveals an altered protein structure and a charge property change by the replacement of 384th Arg residue. The 384th amino acid is mutated from a basic amino acid (Arg, Blue) to an aromatic hydrophobic amino acid (Trp, White). D The I-Mutant v2.0 software reveals that the variant can result in decreased COL9A3 protein stability at optimal pH and temperature. SP: Signal peptide; TC: Triple-helical collagenous region; NC: Non-helical collagenous region; WT: Amino acid in Wild-Type Protein; NEW: New Amino acid with the variant; RI: Reliability Index; pH: − log [H+]; T: Temperature in Celsius degrees.
Discussion
Pedigree-based screening can identify pathogenic genes for heritable LDH. In this study, LDH patients were characterized by early-aged onset, multi-segment disc involvement, dominant inheritance, and the absence of extra-discal deformities in the musculoskeletal system. The clinical significance of the identified COL9A3 variant (c.1150C > T, p.Arg384Trp) has not been previously reported. Our findings suggested that this variant is disease-causing rather than a susceptibility factor for LDH.
Collagen IX plays an important role in forming and stabilizing the collagen matrix in the disc. SNPs that result in tryptophan polymorphisms in collagen IX genes, such as Trp2 allele (p.Gln326Trp) in COL9A2 and Trp3 allele in COL9A3, have been linked to an increased risk of lumbar disc disease in different populations [10, 36]. We summarized the phenotypes, sampling regions, sample sizes and statistical results of COL9A3 pathogenic variants in intervertebral disc diseases (Table 1) and found that results from different studies were inconsistent. In previous research, Trp3 variant (c.307C > T, p.Arg103Trp) was the only pathogenic variant site identified in COL9A3 among populations (Fig. 2A).
To date, various mechanisms have been proposed to explain COL9A3 dysfunction leading to disc disease. For example, Trp3 allele in COL9A3 increases the proportion of tryptophan in the collagen, which subsequently alters the triple helical structure of the protein. This substitution may also disrupt the process of lysyl oxidase-catalysed crosslinking, increase the risk of disc instability, and eventually lead to the occurrence of disc diseases [37]. Also, silencing the expression of COL9A3 can activate the MAPK pathway and downstream apoptosis-related factors, resulting in attenuated NP cells proliferation and promoted cell apoptosis [51]. In animal models, Col9a3 deficient mice exhibit abnormalities in the disc and cartilage, including shortened body height, impaired maturation of articular cartilage, and calcified epiphyseal cartilage [52]. In addition, absence of collagen IX may be related to premature disc degeneration with annular lesions through disrupting the Ihh-PTHrP pathway in ageing mice [53].
Although COL9A3 gene has been repeatedly studied, the underlying mechanism and its effects on the pathogenesis of LDH remain unclear. Results of this study further evidenced that COL9A3 plays an important role in LDH. A new genetic variant was identified in this report, but further studies are needed to explore the pathogenesis of LDH with the COL9A3 pathogenic variant (c.1150C > T, p.Arg384Trp) and develop possible treatment strategies.
Conclusions
In this report, we identified a novel missense pathogenic variant, which is conserved among common species, in a family with multi-segment LDH. The identified COL9A3 variant was predicted to have detrimental effects on the structure and stability of COL9A3. We provided new evidence to support an association between COL9A3 pathogenic variants and LDH, and extended the mutational spectrum of LDH.
Availability of data and materials
Not applicable.
References
Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP. Low back pain. Lancet. 2021;398(10294):78–92. https://doi.org/10.1016/s0140-6736(21)00733-9.
Jordan J, Konstantinou K, O’Dowd J. Herniated lumbar disc. BMJ Clin Evid. 2011;2011:1118.
Ravichandran D, Pillai J, Krishnamurthy K. Genetics of intervertebral disc disease: a review. Clin Anat. 2022;35(1):116–20. https://doi.org/10.1002/ca.23803.
Aicale R, Tarantino D, Maccauro G, Peretti GM, Maffulli N. Genetics in orthopaedic practice. J Biol Regul Homeost Agents. 2019;33(2 Suppl. 1):103–17.
Ou-Yang DC, Kleck CJ, Ackert-Bicknell CL. Genetics of intervertebral disc degeneration. Curr Osteoporos Rep. 2023;21(1):56–64. https://doi.org/10.1007/s11914-022-00769-0.
Huang D, Deng X, Ma K, Wu F, Shi D, Liang H, et al. Association of COL9A3 trp3 polymorphism with intervertebral disk degeneration: a meta-analysis. BMC Musculoskelet Disord. 2018;19(1):381. https://doi.org/10.1186/s12891-018-2297-y.
Luo Y, Sinkeviciute D, He Y, Karsdal M, Henrotin Y, Mobasheri A, et al. The minor collagens in articular cartilage. Protein Cell. 2017;8(8):560–72. https://doi.org/10.1007/s13238-017-0377-7.
Eyre DR, Pietka T, Weis MA, Wu JJ. Covalent cross-linking of the NC1 domain of collagen type IX to collagen type II in cartilage. J Biol Chem. 2004;279(4):2568–74. https://doi.org/10.1074/jbc.M311653200.
Trefilova VV, Shnayder NA, Petrova MM, Kaskaeva DS, Tutynina OV, Petrov KV, et al. The role of polymorphisms in collagen-encoding genes in intervertebral disc degeneration. Biomolecules. 2021. https://doi.org/10.3390/biom11091279.
Paassilta P, Lohiniva J, Göring HH, Perälä M, Räinä SS, Karppinen J, et al. Identification of a novel common genetic risk factor for lumbar disk disease. JAMA. 2001;285(14):1843–9. https://doi.org/10.1001/jama.285.14.1843.
Zhu Y, Wu JJ, Weis MA, Mirza SK, Eyre DR. Type IX collagen neo-deposition in degenerative discs of surgical patients whether genotyped plus or minus for COL9 risk alleles. Spine (Phila Pa 1976). 2011;36(24):2031–8. https://doi.org/10.1097/BRS.0b013e3181ffdd61.
Toktaş ZO, Ekşi M, Yılmaz B, Demir MK, Özgen S, Kılıç T, et al. Association of collagen I, IX and vitamin D receptor gene polymorphisms with radiological severity of intervertebral disc degeneration in Southern European Ancestor. Eur Spine J. 2015;24(11):2432–41. https://doi.org/10.1007/s00586-015-4206-5.
Wu H, Wang S, Chen W, Zhan X, Xiao Z, Jiang H, et al. Collagen IX gene polymorphisms and lumbar disc degeneration: a systematic review and meta-analysis. J Orthop Surg Res. 2018;13(1):47. https://doi.org/10.1186/s13018-018-0750-0.
Karppinen J, Pääkkö E, Paassilta P, Lohiniva J, Kurunlahti M, Tervonen O, et al. Radiologic phenotypes in lumbar MR imaging for a gene defect in the COL9A3 gene of type IX collagen. Radiology. 2003;227(1):143–8. https://doi.org/10.1148/radiol.2271011821.
Xie G, Liang C, Yu H, Zhang Q. Association between polymorphisms of collagen genes and susceptibility to intervertebral disc degeneration: a meta-analysis. J Orthop Surg Res. 2021;16(1):616. https://doi.org/10.1186/s13018-021-02724-8.
Dai Y, Liang S, Dong X, Zhao Y, Ren H, Guan Y, et al. Whole exome sequencing identified a novel DAG1 mutation in a patient with rare, mild and late age of onset muscular dystrophy-dystroglycanopathy. J Cell Mol Med. 2019;23(2):811–8. https://doi.org/10.1111/jcmm.13979.
Han P, Wei G, Cai K, Xiang X, Deng WP, Li YB, et al. Identification and functional characterization of mutations in LPL gene causing severe hypertriglyceridaemia and acute pancreatitis. J Cell Mol Med. 2020;24(2):1286–99. https://doi.org/10.1111/jcmm.14768.
Zhang R, Chen S, Han P, Chen F, Kuang S, Meng Z, et al. Whole exome sequencing identified a homozygous novel variant in CEP290 gene causes Meckel syndrome. J Cell Mol Med. 2020;24(2):1906–16. https://doi.org/10.1111/jcmm.14887.
Vaser R, Adusumalli S, Leng SN, Sikic M, Ng PC. SIFT missense predictions for genomes. Nat Protoc. 2016;11(1):1–9. https://doi.org/10.1038/nprot.2015.123.
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7(4):248–9. https://doi.org/10.1038/nmeth0410-248.
Chao EC, Velasquez JL, Witherspoon MS, Rozek LS, Peel D, Ng P, et al. Accurate classification of MLH1/MSH2 missense variants with multivariate analysis of protein polymorphisms-mismatch repair (MAPP-MMR). Hum Mutat. 2008;29(6):852–60. https://doi.org/10.1002/humu.20735.
Schwarz JM, Rödelsperger C, Schuelke M, Seelow D. MutationTaster evaluates disease-causing potential of sequence alterations. Nat Methods. 2010;7(8):575–6. https://doi.org/10.1038/nmeth0810-575.
Jagadeesh KA, Wenger AM, Berger MJ, Guturu H, Stenson PD, Cooper DN, et al. M-CAP eliminates a majority of variants of uncertain significance in clinical exomes at high sensitivity. Nat Genet. 2016;48(12):1581–6. https://doi.org/10.1038/ng.3703.
Ioannidis NM, Rothstein JH, Pejaver V, Middha S, McDonnell SK, Baheti S, et al. REVEL: an ensemble method for predicting the pathogenicity of rare missense variants. Am J Hum Genet. 2016;99(4):877–85. https://doi.org/10.1016/j.ajhg.2016.08.016.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46(3):310–5. https://doi.org/10.1038/ng.2892.
Houdayer C, Dehainault C, Mattler C, Michaux D, Caux-Moncoutier V, Pagès-Berhouet S, et al. Evaluation of in silico splice tools for decision-making in molecular diagnosis. Hum Mutat. 2008;29(7):975–82. https://doi.org/10.1002/humu.20765.
Jian X, Boerwinkle E, Liu X. In silico prediction of splice-altering single nucleotide variants in the human genome. Nucleic Acids Res. 2014;42(22):13534–44. https://doi.org/10.1093/nar/gku1206.
Siepel A, Bejerano G, Pedersen JS, Hinrichs AS, Hou M, Rosenbloom K, et al. Evolutionarily conserved elements in vertebrate, insect, worm, and yeast genomes. Genome Res. 2005;15(8):1034–50. https://doi.org/10.1101/gr.3715005.
Pollard KS, Hubisz MJ, Rosenbloom KR, Siepel A. Detection of nonneutral substitution rates on mammalian phylogenies. Genome Res. 2010;20(1):110–21. https://doi.org/10.1101/gr.097857.109.
Davydov EV, Goode DL, Sirota M, Cooper GM, Sidow A, Batzoglou S. Identifying a high fraction of the human genome to be under selective constraint using GERP++. PLoS Comput Biol. 2010;6(12):e1001025. https://doi.org/10.1371/journal.pcbi.1001025.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24. https://doi.org/10.1038/gim.2015.30.
Studer G, Tauriello G, Bienert S, Biasini M, Johner N, Schwede T. ProMod3—a versatile homology modelling toolbox. PLoS Comput Biol. 2021;17(1):e1008667. https://doi.org/10.1371/journal.pcbi.1008667.
Waterhouse A, Bertoni M, Bienert S, Studer G, Tauriello G, Gumienny R, et al. SWISS-MODEL: homology modelling of protein structures and complexes. Nucleic Acids Res. 2018;46(W1):W296-303. https://doi.org/10.1093/nar/gky427.
Bienert S, Waterhouse A, de Beer TA, Tauriello G, Studer G, Bordoli L, et al. The SWISS-MODEL repository-new features and functionality. Nucleic Acids Res. 2017;45(D1):D313–9. https://doi.org/10.1093/nar/gkw1132.
Capriotti E, Fariselli P, Casadio R. I-Mutant2.0: predicting stability changes upon mutation from the protein sequence or structure. Nucleic Acids Res. 2005;33(Web Server issue):W306–10. https://doi.org/10.1093/nar/gki375.
Jim JJ, Noponen-Hietala N, Cheung KM, Ott J, Karppinen J, Sahraravand A, et al. The TRP2 allele of COL9A2 is an age-dependent risk factor for the development and severity of intervertebral disc degeneration. Spine (Phila Pa 1976). 2005;30(24):2735–42. https://doi.org/10.1097/01.brs.0000190828.85331.ef.
Solovieva S, Lohiniva J, Leino-Arjas P, Raininko R, Luoma K, Ala-Kokko L, et al. COL9A3 gene polymorphism and obesity in intervertebral disc degeneration of the lumbar spine: evidence of gene-environment interaction. Spine (Phila Pa 1976). 2002;27(23):2691–6. https://doi.org/10.1097/00007632-200212010-00008.
Matsui Y, Wu JJ, Weis MA, Pietka T, Eyre DR. Matrix deposition of tryptophan-containing allelic variants of type IX collagen in developing human cartilage. Matrix Biol. 2003;22(2):123–9. https://doi.org/10.1016/s0945-053x(02)00102-6
Noponen-Hietala N, Kyllönen E, Männikkö M, Ilkko E, Karppinen J, Ott J, Ala-Kokko L. Sequence variations in the collagen IX and XI genes are associated with degenerative lumbar spinal stenosis. Ann Rheum Dis. 2003;62(12):1208–14. https://doi.org/10.1136/ard.2003.008334
Kales SN, Linos A, Chatzis C, Sai Y, Halla M, Nasioulas G, et al. The role of collagen IX tryptophan polymorphisms in symptomatic intervertebral disc disease in Southern European patients. Spine (Phila Pa 1976). 2004;29(11):1266–70. https://doi.org/10.1097/00007632-200406010-00017
Solovieva S, Lohiniva J, Leino-Arjas P, Raininko R, Luoma K, Ala-Kokko L, et al. Intervertebral disc degeneration in relation to the COL9A3 and the IL-1ss gene polymorphisms. Eur Spine J. 2006;15(5):613–9. https://doi.org/10.1007/s00586-005-0988-1
Higashino K, Matsui Y, Yagi S, Takata Y, Goto T, Sakai T, et al. The alpha2 type IX collagen tryptophan polymorphism is associated with the severity of disc degeneration in younger patients with herniated nucleus pulposus of the lumbar spine. Int Orthop. 2007;31(1):107–11. https://doi.org/10.1007/s00264-006-0117-8
Virtanen IM, Karppinen J, Taimela S, Ott J, Barral S, Kaikkonen K, et al. Occupational and genetic risk factors associated with intervertebral disc disease. Spine (Phila Pa 1976). 2007;32(10):1129–34. https://doi.org/10.1097/01.brs.0000261473.03274.5c
Karppinen J, Daavittila I, Solovieva S, Kuisma M, Taimela S, Natri A, et al. Genetic factors are associated with modic changes in endplates of lumbar vertebral bodies. Spine (Phila Pa 1976) 2008;33(11):1236–41. https://doi.org/10.1097/BRS.0b013e318170fd0e
Lim EC, Wong W, Ng GB, Chan L, Tan S, Tow P, et al. Distribution of COL9A2 and COL9A3 Gene Polymorphism in Male Chinese Singaporean–A Pilot Observational Study. Int J Hun Genet. 2011;11(3):193–8.
Rathod TN, Chandanwale AS, Gujrathi S, Patil V, Chavan SA, Shah MN. Association between single nucleotide polymorphism in collagen IX and intervertebral disc disease in the Indian population. Indian J Orthop. 2012;46(4):420–6. https://doi.org/10.4103/0019-5413.97261
Toktaş ZO, Ekşi MŞ, Yılmaz B, Demir MK, Özgen S, Kılıç T, et al. Association of collagen I, IX and vitamin D receptor gene polymorphisms with radiological severity of intervertebral disc degeneration in Southern European Ancestor. Eur Spine J. 2015;24(11):2432–41. https://doi.org/10.1007/s00586-015-4206-5
Bagheri MH, Honarpisheh AP, Yavarian M, Alavi Z, Siegelman J, Valtchinov VI. MRI Phenotyping of COL9A2/Trp2 and COL9A3/Trp3 Alleles in Lumbar Disc Disease: A Case-control Study in South-Western Iranian Population Reveals a Significant Trp3-Disease Association in Males. Spine (Phila Pa 1976). 2016;41(21):1661–7. https://doi.org/10.1097/BRS.0000000000001617
Theodore N, Ahmed AK, Fulton T, Mousses S, Yoo C, Goodwin CR, et al. Genetic Predisposition to Symptomatic Lumbar Disk Herniation in Pediatric and Young Adult Patients. Spine (Phila Pa 1976). 2019;44(11):E640–9. https://doi.org/10.1097/BRS.0000000000002949
Yang X, Jia H, Xing W, Li F, Li M, Sun K, et al. Multiple variants in collagen genes are associated with the susceptibility to lumbar disc herniation in the Chinese population. Eur Spine J. 2020;29(7):1709–16. https://doi.org/10.1007/s00586-020-06299-6
Zhang P, Chang BG. Inhibitory effect on the apoptosis of disc nucleus pulposus cells in rats by silencing COL9A3 gene to mediate MAPK signaling pathway: a study on the function and mechanism. Eur Rev Med Pharmacol Sci. 2020;24(17):8653–64. https://doi.org/10.26355/eurrev_202009_22802.
Wilson R, Norris EL, Brachvogel B, Angelucci C, Zivkovic S, Gordon L, et al. Changes in the chondrocyte and extracellular matrix proteome during post-natal mouse cartilage development. Mol Cell Proteomics. 2012;11(1):M111.014159. https://doi.org/10.1074/mcp.M111.014159.
Kamper M, Paulsson M, Zaucke F. Absence of collagen IX accelerates hypertrophic differentiation in the embryonic mouse spine through a disturbance of the Ihh-PTHrP feedback loop. Cell Tissue Res. 2017;367(2):359–67. https://doi.org/10.1007/s00441-016-2501-z.
Funding
The authors received no financial support for the research, authorship and publication of this article.
Author information
Authors and Affiliations
Contributions
Substantial contributions to research design or the acquisition was done by QH and ZY; analysis or interpretation of data was done by LJ and CW; drafting the paper or revising it critically was done by LJ and CW; approval of the submitted and final versions was done by QH. All authors have read and approved the final submitted manuscript. LJ and CW contribute equally to the article.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics board at The Fourth Affiliated Hospital of Zhejiang University School of Medicine (Approval number: K2022154).
Consent for publication
Informed consent to participate in the study and have their data published in a journal article was obtained from all the participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, L., Wang, C., Ye, Z. et al. A novel missense COL9A3 variant in a pedigree with multiple lumbar disc herniation. J Orthop Surg Res 19, 19 (2024). https://doi.org/10.1186/s13018-023-04481-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04481-2