Abstract
Background
Most patients with lumbar spinal stenosis improve significantly within 6 months of lumbar decompression surgery, however, unfavorable long-term disability may persist in some patients. It was unclear which potential influencing factors were more likely to be associated with disability. This study aimed to assess the association between disability and physical performance, pain, and pain-related anxiety in patients after lumbar decompression surgery.
Methods
Patients who underwent decompression for lumbar spinal stenosis were included. Participants completed the visual analog scale, Oswestry Disability Index, and Pain Anxiety Symptoms Scale-20 to collect pain intensity, disability, and pain-related anxiety information. For physical performance assessment, participants performed timed up and go (TUG), functional reach test (FRT), 6-min walking test, and modified Sorensen test, 6–12 months after lumbar decompression surgery. The associations were examined with bivariate and multivariable linear regression analyses.
Results
A total of 80 patients were included. A significant association between disability and pain-related anxiety, the FRT, and the modified Sorensen test scores was confirmed in multivariable analyses. Both bivariate (r = − 0.75) and multivariable (β = 0.60, 95% CI, 0.24, 0.54; P = 0.00) analyses confirmed that pain-related anxiety was the strongest indicator of disability. The association between disability and pain intensity, TUG, and 6-min walking test scores was not confirmed.
Conclusion
Pain-related anxiety should be considered in the rehabilitation programs after lumbar decompression surgery. The evaluation of all aspects of physical performance following lumbar decompression surgery is also recommended.
Similar content being viewed by others
Introduction
Lumbar spinal stenosis is a common source of low back pain (LBP). It refers to a central canal narrowing or foraminal stenosis leading to leg and back pain. If conservative management of lumbar spinal stenosis is unsuccessful, surgical decompression surgery may be advocated to relieve symptoms [1]. Although most patients with lumbar spinal stenosis improve markedly within 6 months following lumbar decompression surgery [2], an unfavorable long-term disability remains in some patients [3].
Lumbar spinal stenosis is an important cause of disability [1]. Disability is a core issue in LBP, affecting physical performance and aerobic fitness [4]. Many factors such as psychosocial factors, pain intensity, and functional capacity, are reported to be related to disability in LBP individuals [5,6,7]. Psychological factors such as high levels of pain-related anxiety are recognized as a predisposing factor for avoiding physical activity, which leads to disability development and pain maintenance [5].
Physical performance tests are used to assess the functional capacity of people with chronic pain and in particular LBP [8]. The objective physical performance tests use standardized methodology and provide a more comprehensive measure of a person’s function than self-reported measures of physical performance [8]. The 6-min walking test (6MWT), functional reach test (FRT), timed up and go (TUG), and modified Sorensen test are used in clinical practice to evaluate the different aspects of physical performance in individuals with LBP [9,10,11,12].
It is unclear which of the potentially influencing factors (physical performance, pain, and pain-related anxiety) could be a stronger indicator of disability in patients after lumbar decompression surgery. Understanding the association of disability with physical performance, pain, and pain-related anxiety, can be helpful in the development of interventions aimed at modifying these determinants in patients after lumbar decompression surgery.
The purpose of this study was to evaluate the association between disability and physical performance, pain, and pain-related anxiety in patients after lumbar decompression surgery.
Methods
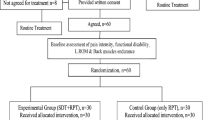
Study design
An observational cross-sectional study was performed from September 2021 to September 2022 in Tehran, Iran. The study was approved by the Ethics Committee of Iran University of Medical Sciences (IR.IUMS.REC.1398.806). All participants signed informed consent before enrollment in the study.
Participants
Participants were recruited via convenience sampling from one university hospital in Tehran, Iran. Adult patients that underwent lumbar decompression surgery without fusion for spinal stenosis by a single surgeon, were included. Evaluation of disability, pain intensity, pain-related anxiety, and physical performance was performed 6–12 months following surgical treatment.
The inclusion criteria were: adults aged 18–60 years, receiving primary lumbar decompression surgery without fusion, and being able to actively participate in the program. Exclusion criteria were: history of prior thoracic, lumbar, or lower extremity surgery, a body mass index (BMI) greater than 35, other neurological diseases, Cobb angle of > 30, pregnancy, decompression for trauma or malignancy, and more than 2-level operation.
Measures
Independent variables
Physical performance
Functional mobility was assessed using the TUG test. TUG has demonstrated acceptable reliability and validity in subjects after surgery for lumbar degenerative diseases [10]. To perform the test, participants were instructed to stand up from a chair, walk 3 m at their comfortable speed, turn, walk back toward the chair, and sit down. The duration of the test was measured in seconds using a chronometer [10].
Functional exercise capacity was measured using the 6MWT. 6MWT is a reliable and valid tool for the assessment of functional exercise capacity in chronic pain trials [9]. The test measures the distance that an individual can walk on a flat surface over a total of six minutes. The more distance traveled; the better performance is recorded [9].
Dynamic balance was assessed using the FRT. Participants were asked to stand next to the wall while keeping their arms straight at shoulder level and reach forward as far as possible, without stepping. The distance between the length of the arm and a maximal forward reach was recorded in the standing position. Longer reaching distances indicate better dynamic balance [11].
Back muscle endurance was evaluated by the modified Sorensen test which is the most widely used test in the literature for evaluating the isometric endurance of back extensor muscle. Participants were positioned prone on an examination table with the upper edges of their iliac crests aligned with the table’s edge. Both lower extremities were fixed to the examining table using three straps at the levels of the pelvis, knees, and ankles. With their arms folded across their chest, participants were instructed to hold their trunks at a horizontal position relative to the ground as long as possible. The time that the participant was able to hold the test position was measured in seconds. Maximum holding time was considered as endurance performance [12].
Pain intensity
Pain intensity was assessed using the visual analog scale (VAS). The scale is a self-administered measure, ranging from 0 points which indicates "no pain" to 10 points which indicates "maximum intensity of pain." The participants rated their current pain intensity using VAS [13].
Pain- related anxiety
Pain-related anxiety was assessed via the Persian short-form version of the Pain Anxiety Symptoms Scale-20 (PASS-20) [14]. The scale is a self-administered questionnaire with 20 items that are rated on a 6-point Likert scale (0 = never, 5 = always). Total score ranges from 0 to 100, with higher scores indicating greater pain-related anxiety. The tool indicates good reliability and validity in LBP subjects [14].
Dependent variable
Disability
Disability was evaluated by the Oswestry Disability Index (ODI). The ODI is a self-administered, 10-item questionnaire designed to assess pain-related disability in individuals with LBP. Each item is scored on a 0–5 scale, with 0 demonstrating no disability and 5 demonstrating the greatest disability. Total score ranged between 0 to 100 percent and higher scores mean higher disability. The Persian version of ODI has shown reliability and validity properties in LBP subjects [15]. According to the cut-off score of 22, participants were considered as of low and high disability [16].
Procedures
Age, sex, height, and weight were recorded at baseline. All participants completed the Persian version of the VAS, ODI, and PASS-20, to collect pain intensity, disability, and pain-related anxiety information. For physical performance assessment, participants perform TUG, FRT, 6MWT, and modified Sorensen test at the same session in a random order. A five-minute rest time was considered between each test to minimize fatigue. All tests were performed by one experienced physiotherapist.
Statistical analysis
The sample size was calculated with G*Power, version 3.1.9.2 for a linear multiple regression model. From a priori analysis, with a power of 80%, α = 0.05, the effect size of f = 2.5, and the total number of predictors and covariates as 8, the required sample size would be 69. Considering 15% dropout, 80 patients were included.
Data analysis was performed using SPSS software, version 26. Numerical data was expressed as mean and standard deviation, while categorical data was presented as frequency and percentage. The normality of the data was verified using a combination of histograms, the Shapiro‐Wilks test, and skew/kurtosis. The independent t-test was used to compare study variables between groups with high and low disability.
To evaluate the bivariate correlation between physical performance, pain-related anxiety, and disability, Pearson’s correlation was used.
A multivariable linear regression analysis was performed to evaluate the contribution of dependent variables (physical performance, pain-related anxiety, and pain intensity) with the independent variable (disability) in patients after lumbar decompression surgery. To control for demographic variables (age, gender, BMI) that could be associated with disability, these variables were selected priori as potential covariates. Only variables with significant bivariate correlation were included in the model. Before performing linear regression analysis, the required assumptions were tested: linearity (scatterplots), normality of dependent variable, and homoscedasticity were tested by plotting the residuals versus the fitted values, and the presence of multicollinearity was determined by a variance inflation factor > 3. The correlation between all independent variables used in the regression analysis was < 0.80. All variables with significant correlations with ODI score were included in a multivariable linear regression analysis. Standardized β values are presented to reflect the direction and strength of the association between each independent variable.
Finally, a stepwise regression analysis was performed with the disability as the dependent variable and only the significant independent variables from the preliminary multivariable analysis. The level of statistical significance was set at p < 0.05.
Results
Eighty individuals who underwent lumbar decompression surgery were included. According to the normality tests, the distribution of data was normal. Table 1 illustrates the comparison of demographic data and functional tests between high and low-disability individuals. The results of the independent t-test showed that there was no significant difference in age and BMI between groups. Individuals with high disability showed significantly higher TUG test time, and lower FRT scores compared to low disability individuals. Moreover, individuals with a higher disability had lower modified Sorensen test times as well. No significant between-group differences were observed for 6MWT scores. In addition, higher PASS-20 scores and greater pain intensity in both low back and lower extremity regions were observed in high-disability individuals.
Bivariate association
The results of bivariate association revealed a significant relationship between physical performance (FRT and modified Sorenson), VAS, and PASS-20 with disability, except 6MWT which showed no significant association. In addition, the strongest association was observed between disability and PASS-20 (r = − 0.75). Table 2 also shows the correlation among study variables. PASS-20 showed a strong negative relationship with FRT and modified Sorenson and a moderate positive association with VAS of leg and back pain.
Linear regression analysis
All tested assumptions met the criteria for conducting a linear regression analysis. Table 3 demonstrates the results of the multivariable linear regression analysis. The results of the preliminary multivariable linear regression analysis revealed a significant contribution of PASS-20, modified Sorensen test, and FRT, to ODI (disability); therefore, these variables were included in the second multivariable analysis. A significant overall model emerged (F = 19.25, P < 0.001), explaining around 68% of ODI variance. Among these predictors, PASS-20 was the strongest predictor of ODI.
Only the significant independent variables used in the multivariable regression analysis were included in the stepwise regression. Stepwise regression analysis (Table 4) revealed that PASS-20 (model 1) accounted for 57% of the variance score on the ODI. In addition, Sorenson and FRT, (model 3) explained up to 67% of the variance in the level of ODI (disability).
Discussion
This study aimed to describe the association between disability and physical performance, pain intensity, and pain-related anxiety among patients 6–12 months post-lumbar decompression surgery. The results revealed significant relationships between disability and pain-related anxiety, the FRT, and the modified Sorensen test scores in patients after lumbar decompression surgery. Pain-related anxiety was the strongest indicator of disability.
The findings showed that high levels of pain-related anxiety had the strongest association with disability. However, the level of pain intensity was not an indicator of disability. This might explain the importance of psychological factors as an indicator of long-term disability post-lumbar surgery. This finding is consistent with previous studies that reported a cumulative negative effect of different elevated psychosocial factors (e.g., fear of movement, catastrophizing, and depression) on long-term disability [17, 18]. Moreover, prior research suggests that pain-related anxiety is associated with disability in individuals with chronic non-specific LBP [19]. Individuals with chronic pain often experience negative emotions related to pain, as well as anxiety and worry about its negative consequences. Therefore, the individual may be more likely to avoid such aversive states by avoiding activities to cope with persistent pain and negative consequences [19].
Although the results of bivariate correlation support the association between disability and pain intensity, this association was not confirmed when other variables were entered into multivariable analyses. This finding demonstrates that high levels of pain-related anxiety, back muscle endurance (assessed by the modified Sorensen test), and dynamic balance (assessed by FRT) were more likely to be associated with disability. An assessment 6–12 months after lumbar decompression surgery may explain the lack of association between pain and disability. This may reflect that patients are experiencing symptom improvement, 6–12 months post-lumbar decompression surgery.
Disability was found to be associated with back muscle endurance (assessed by the modified Sorensen test) and dynamic balance (assessed by FRT). Also, the results of bivariate analysis revealed a strong positive association between modified Sorensen test scores and FRT scores in patients' post-lumbar decompression surgery. Performance of the Sorensen test and FRT involves trunk control and depends on back muscle endurance and strength [12, 20]. In patients who undergo lumbar decompression surgery, preoperative physical deconditioning and prolonged periods of inactivity after surgery may lead to the weakening of the back lumbar muscles [21]. Moreover, lumbar surgery can cause muscle damage and denervation, resulting in postoperative muscle atrophy [22]. Resection of the paraspinal muscles as well as changes in the paraspinal muscles' proprioception may affect trunk muscle strength and result in poor trunk control ability and postural instability [23]. A previous study found that balance improved 6–12 months after lumbar decompression surgery compared to pre-surgery. However, balance impairment was still observed compared to healthy individuals [24]. Dynamic balance control is crucial for performing upright standing tasks. Nevertheless, unstable balance control after surgery may increase the fall risk during activities of daily living [24]. Therefore, dynamic balance assessments and postoperative rehabilitation training are necessary after lumbar decompression surgery.
The results also revealed that while modified Sorensen test and FRT scores were strongly correlated with disability, TUG and 6MWT scores had no statistically significant correlation with disability. This finding aligns with previous research, which identified TUG test scores after lumbar decompression surgery was within the normal population range [25]. Modified Sorensen test and FRT examine spine-related functions and their performance depends on the endurance and strength of the back extensor muscles [12, 20] which are probably affected by surgery, whereas TUG and 6MWT provide global information regarding overall physical performance [26]. This finding highlights the importance of a comprehensive evaluation of all aspects of physical performance in patients after lumbar decompression surgery.
The results confirm that pain-related anxiety has the potential to improve disability in patients after lumbar decompression surgery; however, there is a need for additional targets to also improve back muscle endurance and dynamic balance, which are important aspects of physical performance.
Limitations
The present study has some limitations. First, despite using valid and reliable questionnaires, the self-reported nature of the questionnaires might have led to recall bias. Second, the association of other psychological factors with disability (such as kinesiophobia, fear avoidance, …) was not assessed. Finally, the cross-sectional design of the study limits the evidence level of the findings.
Conclusion
The presence of an association between disability and pain-related anxiety, and some aspects of physical performance (back muscle endurance, and dynamic balance) was supported in patients 6–12 months after lumbar decompression surgery. However, the association between disability and pain intensity, and some aspects of physical performance (functional mobility, and functional exercise capacity) could not be confirmed.
The results suggest that pain-related anxiety should be considered in the rehabilitation programs of patients after lumbar decompression surgery. Also, exercise programs that focus on back muscle endurance and dynamic balance may be crucial after lumbar decompression surgery. Moreover, a comprehensive evaluation of all aspects of physical performance is suggested in patients after lumbar decompression surgery.
Availability of data and materials
The data presented in this study are available on reasonable request from the corresponding author.
Abbreviations
- 6MWT:
-
6-Minute walking test
- BMI:
-
Body mass index
- FRT:
-
Functional reach test
- LBP:
-
Low back pain
- ODI:
-
Oswestry Disability Index
- PASS-20:
-
Pain Anxiety Symptoms Scale-20
- TUG:
-
Timed up and go
- VAS:
-
Visual analog scale
References
Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016;352: h6234.
Oba H, Takahashi J, Tsutsumimoto T, Ikegami S, Ohta H, Yui M, et al. Predictors of improvement in low back pain after lumbar decompression surgery: prospective study of 140 patients. J Orthop Sci. 2017;22(4):641–6.
Watanabe K, Otani K, Nikaido T, Kato K, Kobayashi H, Handa J, et al. Usefulness of the brief scale for psychiatric problems in orthopaedic patients (BS-POP) for predicting poor outcomes in patients undergoing lumbar decompression surgery. Pain Res Manag. 2021. https://doi.org/10.1155/2021/2589865.
Lin C-WC, McAuley JH, Macedo L, Barnett DC, Smeets RJ, Verbunt JAJP. Relationship between physical activity and disability in low back pain: a systematic review and meta-analysis. Pain. 2011;152(3):607–13.
Miki T, Higuchi D, Takebayashi T, Samukawa M. Factors associating with disability of non-specific low back pain in different subgroups: a hierarchical linear regression analysis. Sci Rep. 2021;11(1):18278.
Shanbehzadeh S, ShahAli S, Ebrahimi Takamjani I, Vlaeyen JWS, Salehi R, Jafari H. Association of pain-related threat beliefs and disability with postural control and trunk motion in individuals with low back pain: a systematic review and meta-analysis. Eur Spine J. 2022;31(7):1802–20.
Rasouli O, Shanbehzadeh S, Arab AM, ShahAli S, Sarafraz H. The Effect of respiratory phase on abdominal muscle activity during stable and unstable sitting positions in individuals with and without chronic low back pain. J Manipulative Physiol Ther. 2020;43(3):225–33.
Andersson EI, Lin CC, Smeets RJ. Performance tests in people with chronic low back pain: responsiveness and minimal clinically important change. Spine. 2010;35(26):E1559–63.
Taylor AM, Phillips K, Patel KV, Turk DC, Dworkin RH, Beaton D, et al. Assessment of physical function and participation in chronic pain clinical trials: IMMPACT/OMERACT recommendations. Pain. 2016;157(9):1836–50.
Gautschi OP, Smoll NR, Corniola MV, Joswig H, Chau I, Hildebrandt G, et al. Validity and reliability of a measurement of objective functional impairment in lumbar degenerative disc disease: the timed up and go (TUG) test. Neurosurgery. 2016;79(2):270–8.
Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192–7.
Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine. 1984;9(2):106–19.
Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45–56.
Shanbehzadeh S, Salavati M, Tavahomi M, Khatibi A, Talebian S, Khademi-Kalantari K. Reliability and validity of the pain anxiety symptom scale in Persian speaking chronic low back pain patients. Spine. 2017;42(21):E1238–44.
Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry disability index, the Roland–Morris disability questionnaire, and the Quebec back pain disability scale: translation and validation studies of the Iranian versions. Spine. 2006;31(14):E454–9.
Tonosu J, Takeshita K, Hara N, Matsudaira K, Kato S, Masuda K, et al. The normative score and the cut-off value of the Oswestry disability index (ODI). Eur Spine J. 2012;21(8):1596–602.
Westman AE, Boersma K, Leppert J, Linton SJ. Fear-avoidance beliefs, catastrophizing, and distress: a longitudinal subgroup analysis on patients with musculoskeletal pain. Clin J Pain. 2011;27(7):567–77.
Wideman TH, Sullivan MJ. Development of a cumulative psychosocial factor index for problematic recovery following work-related musculoskeletal injuries. Phys Ther. 2012;92(1):58–68.
Varela AJ, Van Asselt KW. The relationship between psychosocial factors and reported disability: the role of pain self-efficacy. BMC Musculoskelet Disord. 2022;23(1):21.
de Waroquier-Leroy L, Bleuse S, Serafi R, Watelain E, Pardessus V, Tiffreau AV, et al. The functional reach test: strategies, performance and the influence of age. Ann Phys Rehabil Med. 2014;57(6):452–64.
Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine. 1994;19(2):165–72.
Bresnahan LE, Smith JS, Ogden AT, Quinn S, Cybulski GR, Simonian N, et al. Assessment of paraspinal muscle cross-sectional area after lumbar decompression. Clin Spine Surg. 2017;30(3):E162–8.
Song J, Araghi K, Dupont MM, Shahi P, Bovonratwet P, Shinn D, et al. Association between muscle health and patient-reported outcomes after lumbar microdiscectomy: early results. Spine J. 2022;22(10):1677–86.
Wong WJ, Lai DM, Wang SF, Wang JL, Hsu WL. Changes of balance control in individuals with lumbar degenerative spine disease after lumbar surgery: a longitudinal study. Spine J. 2019;19(7):1210–20.
Stienen MN, Maldaner N, Joswig H, Corniola MV, Bellut D, Prömmel P, et al. Objective functional assessment using the “Timed Up and Go” test in patients with lumbar spinal stenosis. Neurosurg Focus. 2019;46(5):E4.
Carvalho FA, Maher CG, Franco MR, Morelhao PK, Oliveira CB, Silva FG, et al. Fear of movement is not associated with objective and subjective physical activity levels in chronic nonspecific low back pain. Arch Phys Med Rehabil. 2017;98(1):96–104.
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
SSA, SS, and KK made concept and design. MS helped in data collection. SSA and SS helped in data analysis and interpretation. MS, SSA, SS, and KK done manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in agreement with the Declaration of Helsinki and was approved by the Human Research Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.REC.1398.806). All participants signed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sahebalam, M., ShahAli, S., Komlakh, K. et al. The association between disability and physical performance, pain intensity, and pain-related anxiety in patients after lumbar decompression surgery: a cross-sectional study. J Orthop Surg Res 18, 961 (2023). https://doi.org/10.1186/s13018-023-04462-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04462-5