Abstract
Background
This study aimed to systematically evaluate risk factors for post-operative recurrence after percutaneous endoscopic lumbar discectomy (PELD) in patients with lumbar disc herniation (LDH).
Methods
The eligible studies were retrieved from PubMed, Embase, and Web of Science databases. Quality assessment was performed. The effects of binary variables (sex, Modic change (MC), type 2 diabetes (T2DM), and smoking) on post-operative recurrence were evaluated as odds ratio (OR) and 95% confidence interval (CI). The effects of continuous variables (sagittal range of motion (SROM), body mass index (BMI), and age) were assessed as weighted mean difference (WMD) and 95% CI. Sensitivity analysis and publication bias were conducted to evaluate the reliability of pooled results.
Results
Eight studies were included, and their methodological quality was medium. MC (OR (95% CI) = 3.88 (2.24–6.74), P < 0.001), smoking (OR (95% CI) = 1.87 (1.45, 2.42), P < 0.001), T2DM (OR (95% CI) = 1.61 (1.12, 2.31), P = 0.010), SROM (WMD (95% CI) = 2.33 (0.95, 3.70), P = 0.001), BMI (WMD (95% CI) = 1.68 (1.37, 1.99) kg/m2, P < 0.001), and age (WMD (95% CI) = 9.95 (5.05, 14.86) years, P < 0.001) were significantly related to post-operative recurrence in patients with LDH after PELD. Significant publication bias was not observed among studies in all outcome indicators.
Conclusion
Our findings reveal that high levels of age, BMI, and SROM, history of T2DM or smoking, or more MC may be correlated with post-operative recurrence after PELD.
Highlights
-
1.
Eight studies were included in this meta-analysis.
-
2.
The methodological quality of the included studies was medium.
-
3.
MC, smoking, T2DM, SROM, BMI, and age were related to post-operative recurrence.
-
4.
There was no publication bias among studies in all outcome indicators.
Similar content being viewed by others
Background
Lumbar disc herniation (LDH) is a common spinal degenerative disease, presenting as clinical symptoms such as pain and neurological dysfunction. It often leads to the compression of nerve roots and dural sac, resulting in an inflammatory response [1]. Over 95% of LDH occurs in L4-5 and L5-S1 [2, 3], and the prevalence of LDH is 1–3% [4]. If the clinical symptoms of patients are not relieved after 6 weeks of conservative treatment, surgery is often required [5]. Over the past decades, many minimally invasive procedures have been used to treat LDH, achieving similar outcomes as the conventional open surgery [6].
As a popular minimally invasive technique, percutaneous endoscopic lumbar discectomy (PELD) has been increasingly used for LDH treatment. In comparison with the conventional open surgery, this surgery has the minimal muscle injury and blood loss [7, 8]. However, some patients experience post-operative recurrence after PELD, and the incidence of recurrent LDH (rLDH) is reported to be 5–15% [9]. rLDH often requires secondary surgery, which brings additional physical and psychological trauma for patients. To prevent post-operative recurrence after PELD, numerous studies are devoted to explore risk factors, such as age, degree of disc degeneration, sex, experience of the surgeon, smoking, body mass index (BMI), Modic change (MC), and location of herniation [10,11,12]. Nevertheless, these previous studies on risk factors have failed to reach a consistent conclusion [13,14,15,16,17]. In light of these controversies, it is necessary to conduct more research with a relatively larger sample size to explore the risk factors for recurrence after PELD.
In this study, we aimed to systematically evaluate risk factors related to post-operative recurrence after PELD by meta-analysis of existing research evidence. Our finding will offer support for the post-operative care of patients with LDH.
Methods
Search strategy
Using the pre-established search strategy, we retrieved eligible studies from Embase, PubMed, and Web of Science databases. The search keywords were as follows: “lumbar disc herniation”, “percutaneous endoscopic transforaminal discectomy”, “percutaneous endoscopic lumbar discectomy”, and “percutaneous endoscopic interlaminar discectomy”. The subject and free words were combined for retrieval, and the search procedures depended on the characteristics of different databases (Additional file 3: Tables S1–S3). The literature search was available until March 3, 2023, without language limits. To retrieve additional studies, relevant reviews and reference lists of included articles were manually retrieved. This meta-analysis was completed following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline.
Inclusion and exclusion criteria
The inclusion criteria were: (1) the study subjects were newly diagnosed LDH patients receiving PELD; (2) the outcome was recurrence; (3) the study reported the differences of sex, BMI, MC, smoking and other factors between the recurrence and non-recurrence groups; (4) the study type was prospective or retrospective cohort study.
The exclusion criteria were: (1) the study subjects were rLDH; (2) if data were repeated published or included in multiple articles, only the one that had the most complete study information was included and the rest were excluded; and (3) non-authoritative studies, such as comments, reviews, and conference abstracts.
Data extraction
The study selection was carried out independently by two investigators. They then independently extracted data from eligible studies based on the pre-designed standardized table. The data to be extracted included first author, publication year, study area, study types, basic characteristics of subjects (sample size, age, and sex), follow-up time, study number, and influencing factors. After completing data extraction work, they exchanged and reviewed extraction tables and resolved inconsistent data by discussion.
Quality assessment
The methodological qualities of cohort and case–control studies were evaluated using the Newcastle–Ottawa Scale (NOS) [18]. This scale included three aspects: object selection, comparability, and exposure (8 scoring items with a total of 9 points). Studies with cumulative scores of 7–9, 4–6, and < 4 were considered high quality, medium, and low quality.
Statistical analysis
The binary variables were expressed as odds ratio (OR) and 95% confidence interval (CI). The continuous variables were presented as weighted mean difference (WMD) and 95% CI. The Cochran’s Q test and I2 test were used to detect the heterogeneity of included studies [19]. Sensitivity analysis was performed by removing the included studies one by one to assess whether the pooled results of meta-analysis was impacted by a single included study [20]. The study publication bias was evaluated using Egger test [21]. These statistical analyses were performed using Stata12.0 software (Stata Corp, College Station, TX, USA).
Results
Study selection
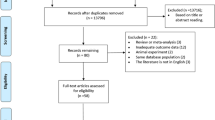
A flowchart depicting literature extraction is presented in Fig. 1. Following the search strategy, 1932 studies (PubMed (606), Embase (658), and Web of Science (668)) met the included criteria. Then, 875 duplications were excluded. After further screening titles and abstracts, 1045 studies were excluded. By full-text reading, eight studies [15,16,17, 22,23,24,25,26] were eligible. No additional studies were obtained by manual search.
Basic characteristics and quality assessment
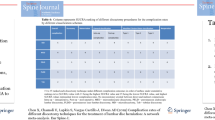
As shown in Table 1, the included studies were published between 2019 and 2023 and conducted in China, Japan, and South Korea. All included studies were retrospective cohort studies. The sample size of included studies was 102–942 cases, with a total of 4433 cases (2629 males and 1804 females). The subjects were followed up for 0.5–6.25 years, and the recurrence rate was 6.1–9.5%.
Quality assessment results showed that the NOS scores of the included studies were 5–6, and the methodological quality was medium (Table 2).
Meta-analysis results
After data extraction and collation, it was found that meta-analysis could be performed on four binary variables (sex, MC, type 2 diabetes (T2DM), and smoking) and three continuous variables (sagittal range of motion (SROM), BMI, and age).
Seven studies reported the difference in sex (male vs. female). After the heterogeneity test (I2 = 28.4%, P = 0.212), the fixed-effect model was utilized for analysis. The pooled OR was 1.07 (95% CI: 0.85–1.35, P = 0.565) (Fig. 2A). Six studies reported the difference in MC (MC vs. non-MC). The heterogeneity test showed that there was significant heterogeneity (I2 = 62.8%, P = 0.020); thus, the random-effect model was applied for analysis. The pooled OR was 3.88 (95%CI: 2.24–6.74, P < 0.001) (Fig. 2B). Six studies reported the association between smoking or T2DM and recurrence, and there was no significant heterogeneity among studies (I2 < 50%, P > 0.05). The pooled results of the fixed-effect model for smoking and T2DM were OR (95% CI) = 1.87 (1.45, 2.42) (P < 0.001, Fig. 2C) and OR (95% CI) = 1.61 (1.12, 2.31) (P = 0.010, Fig. 2D), respectively.
Three studies reported the SROM difference, and there was significant heterogeneity (I2 = 83.0%, P = 0.003). The pooled results of the random-effect model were WMD (95% CI) = 2.33 (0.95, 3.70) (P = 0.001, Fig. 3A). Four studies compared the differences in BMI and age. For BMI, no significant heterogeneity existed (I2 = 0%, P = 0.842), and the pooled result of the fixed-effect model was WMD (95% CI) = 1.68 (1.37, 1.99) kg/m2 (P < 0.001, Fig. 3B). Significant heterogeneity existed among studies reporting age (I2 = 92.3%, P < 0.001), and the pooled result of the random-effect model was WMD (95% CI) = 9.95 (5.05, 14.86) years (P < 0.001, Fig. 3C).
Sensitivity analysis
The pooled results of the above outcome indicators were not significantly affected after removing literatures one by one, suggesting that our results were stable (Additional file 1: Fig. S1A–D, Additional file 2: Fig. S2A–C).
Publication bias
The results of Egger test indicated that the included studies had no significant publication bias on all outcome indicators, including sex (P = 0.414), MC (P = 0.839), smoking (P = 0.262), T2DM (P = 0.091), SROM (P = 0.997), BMI (P = 0.254), and age (P = 0.873).
Discussion
rLDH is a common complication of PELD and leads to unsatisfactory outcomes in patients with LDH after PELD. However, the occurrence of rLDH after PELD involves a variety of complex factors, and its risk factors are controversial. Therefore, we conducted this meta-analysis to systematically assess risk factors for post-operative recurrence in patients with LDH after PELD. Herein, we found that risk factors such as age, MC, BMI, smoking, T2DM, and SROM were related to post-operative recurrence in LDH patients after PELD.
In line with previous findings [7, 27], age is revealed as a risk factor for post-operative recurrence after PELD. It is reported that age is associated with lumbar disc degeneration in the elderly, which may increase the pressure on the disc and consequently result in post-operative recurrence [28, 29]. Modic changes, manifested as alterations in the signals of the vertebral endplate and adjacent bone marrow, are found to be related to vertebral endplate fissures and disc herniation [30,31,32]. The post-operative back pain and functional status of patients with MCs after PELD show a deterioration trend with the time extension [33], suggesting the potential association between MC and risk of post-operative recurrence. High BMI is also considered as a risk factor of rLDH occurrence after PELD because high BMI can augment the spinal load of patients, which may increase disc pressure and impair nutrient supply to the disc, resulting in reduced annulus healing and accelerated disc degeneration [34]. SROM can lead to intervertebral space instability, which is a contributing factor to the increased risk of post-operative recurrence caused by SROM [35]. In addition, smoking is revealed as a risk factor for post-operative recurrence in our study. The possible reason is that nicotine can promote vasoconstriction and induce progressive disc degeneration, thereby increasing the risk of post-operative recurrence [36, 37]. In this meta-analysis, these risk factors were related to post-operative recurrence in LDH patients after PELD. Moreover, the pooled results of this meta-analysis were not significantly affected by a single included study, and no publication bias was observed among studies, indicating that the results were stable and reliable.
Despite these virtues, we should not overlook the limitations of this meta-analysis. Firstly, significant heterogeneity was observed in the included studies of MC, SROM and age. Owing to the small number of studies and insufficient information, it was impossible to explore the sources of heterogeneity by quantitative methods such as subgroup or meta-regression analyses. Secondly, all included studies were observational studies with a large number of confounding factors. The results were not adjusted for multiple factors, potentially leading to an overestimation of the differences between groups. Thirdly, many factors are related to post-operative recurrence, and the list of factors in this study may not have been comprehensive. Therefore, more studies with high quality and large samples are still needed to validate our results.
Conclusion
In conclusion, our results indicate that high levels of age, BMI, and SROM, history of T2DM or smoking, or more MC may be correlated with rLDH after PELD. It is recommended that patients with these risk factors should pay more attention to preventing post-operative recurrence.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- PELD:
-
Percutaneous endoscopic lumbar discectomy
- LDH:
-
Lumbar disc herniation
- MC:
-
Modic change
- T2DM:
-
Type 2 diabetes
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- SROM:
-
Sagittal range of motion
- BMI:
-
Body mass index
- WMD:
-
Weighted mean differences
- rLDH:
-
Recurrent LDH
- NOS:
-
Newcastle–Ottawa Scale
References
Yu P, Mao F, Chen J, Ma X, Dai Y, Liu G, et al. Characteristics and mechanisms of resorption in lumbar disc herniation. Arthritis Res Ther. 2022;24(1):205.
Deyo RA, Mirza SK. Herniated lumbar intervertebral disk. N Engl J Med. 2016;374(18):1763–72.
Benlidayi IC, Başaran S, Seydaoğlu G. Lumbosacral morphology in lumbar disc herniation: a chicken and egg issue. Acta Orthop Traumatol Turc. 2016;50(3):346–50.
Ito S, Nakashima H, Sato K, Deguchi M, Matsubara Y, Kanemura T, et al. Laterality of lumbar disc herniation. J Orthop Sci. 2022. https://doi.org/10.1016/j.jos.2022.10.003.
Wu X-B, Fan G-X, Gu X, Shen T-G, Guan X-F, Hu A-N, et al. Learning curves of percutaneous endoscopic lumbar discectomy in transforaminal approach at the L4/5 and L5/S1 levels: a comparative study. J Zhejiang Univ Sci B. 2016;17(7):553.
Kanno H, Aizawa T, Hahimoto K, Itoi E. Minimally invasive discectomy for lumbar disc herniation: current concepts, surgical techniques, and outcomes. Int Orthop. 2019;43:917–22.
Yao Y, Liu H, Zhang H, Wang H, Zhang C, Zhang Z, et al. Risk factors for recurrent herniation after percutaneous endoscopic lumbar discectomy. World Neurosurg. 2017;100:1–6.
Yin S, Du H, Yang W, Duan C, Feng C, Tao H. Prevalence of recurrent herniation following percutaneous endoscopic lumbar discectomy: a meta-analysis. Pain Physician. 2018;21(4):337.
Li Z, Yang H, Liu M, Lu M, Chu J, Hou S, et al. Clinical characteristics and risk factors of recurrent lumbar disk herniation: a retrospective analysis of three hundred twenty-one cases. Spine. 2018;43(21):1463–9.
Park CH, Park ES, Lee SH, Lee KK, Kwon YK, Kang MS, et al. Risk factors for early recurrence after transforaminal endoscopic lumbar disc decompression. Pain Physician. 2019;22(2):E133.
Kim J, Lee S, Ahn Y, Yoon D, Lee C, Lim S. Recurrence after successful percutaneous endoscopic lumbar discectomy. Min-Minim Invasive Neurosurg. 2007;50(02):82–5.
Yaman ME, Kazancı A, Yaman ND, Baş F, Giyas A. Factors that influence recurrent lumbar disc herniation. 2017.
Shi H, Zhu L, Jiang Z-L, Wu X-T. Radiological risk factors for recurrent lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: a retrospective matched case-control study. Eur Spine J. 2021;30:886–92.
Abdallah A, Güler AB. Factors associated with the recurrence of lumbar disk herniation: non-biomechanical–radiological and intraoperative factors. Neurol Res. 2023;45(1):11–27.
Jia M, Sheng Y, Chen G, Zhang W, Lin J, Lu S, et al. Development and validation of a nomogram predicting the risk of recurrent lumbar disk herniation within 6 months after percutaneous endoscopic lumbar discectomy. J Orthop Surg Res. 2021;16(1):1–10.
Ono K, Ohmori K, Yoneyama R, Matsushige O, Majima T. Risk factors and surgical management of recurrent herniation after full-endoscopic lumbar discectomy using interlaminar approach. J Clin Med. 2022;11(3):748.
Kong M, Xu D, Gao C, Zhu K, Han S, Zhang H, et al. Risk factors for recurrent L4–5 disc herniation after percutaneous endoscopic transforaminal discectomy: a retrospective analysis of 654 cases. Risk Manag Healthc Policy. 2020. https://doi.org/10.2147/RMHP.S287976.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford; 2000.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Tobias A. Assessing the influence of a single study in the meta-analysis estimate. Stata Tech Bull. 1999;47:15–7.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Hao L, Li S, Liu J, Shan Z, Fan S, Zhao F. Recurrent disc herniation following percutaneous endoscopic lumbar discectomy preferentially occurs when Modic changes are present. J Orthop Surg Res. 2020;15:1–5.
He H, Ma J, Xiong C, Wei T, Tang A, Chen Y, et al. Development and validation of a nomogram to predict the risk of lumbar disk reherniation within 2 years after percutaneous endoscopic lumbar discectomy. World Neurosurg. 2023;172:e349–56.
Kim HS, You JD, Ju CI. Predictive scoring and risk factors of early recurrence after percutaneous endoscopic lumbar discectomy. BioMed Res Int. 2019. https://doi.org/10.1155/2019/6492675.
Wang F, Chen K, Lin Q, Ma Y, Huang H, Wang C, et al. Earlier or heavier spinal loading is more likely to lead to recurrent lumbar disc herniation after percutaneous endoscopic lumbar discectomy. J Orthop Surg Res. 2022;17(1):356.
Yu C, Zhan X, Liu C, Liao S, Xu J, Liang T, et al. risk factors for recurrent L5–S1 disc herniation after percutaneous endoscopic transforaminal discectomy: a retrospective study. Med Sci Monit Int Med J Exp Clin Res. 2020;26:e919888–91.
Wu J, Zhang C, Lu K, Li C, Zhou Y. Percutaneous endoscopic lumbar reoperation for recurrent sciatica symptoms: a retrospective analysis of outcomes and prognostic factors in 94 patients. World Neurosurg. 2018;109:e761–9.
Kienzler JC, Fandino J, Van de Kelft E, Eustacchio S, Bouma GJ, Group BACRS. Risk factors for early reherniation after lumbar discectomy with or without annular closure: results of a multicenter randomized controlled study. Acta neurochirurgica. 2021;163:259–68.
McGirt MJ, Eustacchio S, Varga P, Vilendecic M, Trummer M, Gorensek M, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine. 2009;34(19):2044–51.
Schmid G, Witteler A, Willburger R, Kuhnen C, Jergas M, Koester O. Lumbar disk herniation: correlation of histologic findings with marrow signal intensity changes in vertebral endplates at MR imaging. Radiology. 2004;231(2):352–8.
Joe E, Lee JW, Park KW, Yeom JS, Lee E, Lee GY, et al. Herniation of cartilaginous endplates in the lumbar spine: MRI findings. Am J Roentgenol. 2015;204(5):1075–81.
Shan Z, Fan S, Xie Q, Suyou L, Liu J, Wang C, et al. Spontaneous resorption of lumbar disc herniation is less likely when modic changes are present. Spine. 2014;39(9):736–44.
Xu J, Li Y, Wang B, Guo-Hua L, Wu P, Dai Y, et al. Percutaneous endoscopic lumbar discectomy for lumbar disc herniation with modic changes via a transforaminal approach: a retrospective study. Pain Physician. 2019;22(6):E601.
Ren G, Liu L, Zhang P, Xie Z, Wang P, Zhang W, et al. Machine learning predicts recurrent lumbar disc herniation following percutaneous endoscopic lumbar discectomy. Glob Spine J. 2022. https://doi.org/10.1177/219256822210976.
Kim K-T, Park S-W, Kim Y-B. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine. 2009;34(24):2674–8.
Gill CS, Sandell LJ, El-Zawawy HB, Wright RW. Effects of cigarette smoking on early medial collateral ligament healing in a mouse model. J Orthop Res. 2006;24(12):2141–9.
Nemoto Y, Matsuzaki H, Tokuhasi Y, Okawa A, Uematu Y, Nishimura T, et al. Histological changes in intervertebral discs after smoking cessation: experimental study using a rat passive smoking model. J Orthop Sci. 2006;11(2):191–7.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study conception and design were done by JD; data acquisition was done by LJ and XX; data analysis and interpretation were done by LJ and XX; statistical analysis was done by LJ and XX; drafting of the manuscript was done by LJ and RFH; critical revision of the manuscript for important intellectual content was done by JD. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Figure S1
. Sensitivity analysis results showed that the pooled results of sex (A), MC (B), smoking (C), and T2DM (D) on post-operative recurrence were not significantly affected after removing literatures one by one.
Additional file 2. Figure S2
. Sensitivity analysis results showed that the pooled results of SROM (A), BMI (B), and age (C) on post-operative recurrence were not significantly affected after removing literatures one by one.
Additional file 3
. The retrieval steps and results of Pubmed, Embase, and Web of Science, respectively.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, L., Xie, X., He, R. et al. Analysis of risk factors for post-operative recurrence after percutaneous endoscopic lumbar discectomy in patients with lumbar disc herniation: a meta-analysis. J Orthop Surg Res 18, 935 (2023). https://doi.org/10.1186/s13018-023-04378-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04378-0