Abstract
Background
Lumbar disc herniation (LDH) is a complex spinal disease, with multiple genetic polymorphisms being related to its risk. Nevertheless, the role of LINC-PINT polymorphisms in LDH risk has remained unknown. Therefore, this study aimed to investigate the association between LINC-PINT polymorphisms and LDH risk.
Methods
DNA was extracted from 504 LDH patients and 500 healthy controls. Three single nucleotide polymorphisms (SNPs) in LINC-PINT were selected and genotyped using Agena MassARRAY. We used logistic regression analysis to calculate odds ratios (ORs) and 95% confidence intervals (95% CIs) under multiple genetic models to evaluate the association between LINC-PINT polymorphisms and LDH risk. Haploview 4.2 and SNPStats software were used to evaluate the linkage strength of SNPs and the correlation between haplotypes and LDH risk. The impact of SNP-SNP interactions on LDH risk was analyzed using multi-factor dimensionality reduction (MDR).
Results
Results showed that rs157916 (G vs. A: OR = 1.23, FDR-p = 0.029) and rs7801029 (G vs. C: OR = 1.39, FDR-p = 0.006; GG vs. CC: OR = 2.34, FDR-p = 0.038; recessive: OR = 2.13, FDR-p = 0.045; additive: OR = 1.39, FDR-p = 0.030) were associated with an increased risk of LDH. Furthermore, LINC-PINT rs157916 and rs780129 were found to be significantly associated with LDH risk in males. The “GGG” haplotype was associated with increased LDH risk (OR = 1.41, FDR-p = 0.006). MDR analysis indicated that the interaction between rs7801029 and rs16873842 was associated with an increased risk of LDH (OR = 1.47, p = 0.004). Additionally, there were significant differences in C-reactive protein levels among different genotypes of rs157916 and rs780129 (p < 0.05).
Conclusion
This study suggests that LINC-PINT gene polymorphisms (rs157916 and rs7801029) are considered risk factors for LDH in the Chinese Han population and provide a scientific basis for early screening, prevention, and diagnosis of LDH.
Similar content being viewed by others
Background
Lumbar disc herniation (LDH) is a significant health concern that affects many people, particularly those leading a sedentary lifestyle [1]. As a global issue, research indicates that 80% of the population will experience LDH at least once in their lifetime [2]. Besides, 20% of individuals with LDH require surgical treatment during the course of the disease because of prolonged or aggravated leg pain [3]. Although the the pathogenesis of LDH is unclear, it may be attributed to endogenous factors (hereditary, developmental, and degenerative factors) and exogenous factors (stress, nutrition, strain, trauma and other factors) [4]. Epidemiological studies suggest that disc degeneration, including disc herniation and sciatica, may be explained primarily by genetic factors [5]. The genetics of bone diseases studies have revealed a substantial contribution of polymorphisms to the development of bone disorders [6,7,8]. Some prior studies have linked genetic variations in certain genes, such as matrix metalloproteinase, to intervertebral disc extracellular matrix that could lead to degenerative intervertebral disc disease and symptoms [9]. Additionally, many gene polymorphisms are linked to LDH, such as VDR [10], STOX1 [11], and MIR31HG [12]. Recently, research reveals that long noncoding RNAs (lncRNAs) play a critical role in biological processes, with abnormal expression linked to human diseases such as intervertebral disc degeneration, and osteoarthritis [13,14,15].
Long-chain RNA p53-induced transcript (lncRNA LINC-PINT) is a newly discovered lncRNA that plays a vital role in multiple physiological and pathological processes, including glioblastoma [16], lung cancer [17], and thyroid cancer [18]. LINC-PINT has high expression levels in bone marrow and has shown relations to various bone-related disorders. LINC-PINT is downregulated in rheumatoid arthritis (RA) tissues and TNF-α stimulated RA cells, increasing SOCS1 expression by inhibiting the activation of the ERK signaling pathway in RA synovial fibroblasts induced by TNF-α by sponging miR-155-5p [19]. Previous research has linked polymorphisms in LINC-PINT with the occurrence and development of various diseases. For instance, rs157928 in LINC-PINT was significantly associated with a decreased risk of high-altitude pulmonary edema [20]. The LINC-PINT SNP rs10228040 was associated with increased susceptibility to pemphigus foliaceus [21]. Moreover, two SNPs in LINC-PINT (rs157916 and rs16873842) was associated witn a reduced risk of steroid-induced osteonecrosis of the femoral head [22], and LINC-PINT polymorphisms (rs157916, rs16873842, and rs7801029) were associated with reduced risk liver cancer [23]. However, the association between LINC-PINT polymorphisms and risk of LDH has not been previously investigated.
Therefore, our study aimed to investigate the genetic association between LINC-PINT polymorphisms (rs157916, rs16873842, and rs7801029) and susceptibility to LDH in the Chinese Han population through a case–control study (comprising 504 LDH patients and 500 healthy controls). The findings from our study will provide new insights into the underlying mechanisms, diagnosis, and treatment of LDH.
Materials and methods
Study participants
We employed G*Power (3.1.9.7) software to estimate the sample size, and recruited 504 LDH patients who suffered from low back pain and lumbar radiculopathy and 500 controls from the Second Affiliated Hospital of Inner Mongolia Medical University. Patients with typical clinical symptoms and signs of lumbar dysfunction were diagnosed as having lumbar dysentery via computer tomography and magnetic resonance tomography. The inclusion criteria for the control group required that physical examination results showed them to be healthy and to have no recent history of infection, lumbar displacement, lumbar muscle tone, sciatica, low back pain, osteoarthritis, or RA. We excluded individuals with other spinal diseases (such as scoliosis, osteoporosis, etc.) or nervous system disease (such as epilepsy, Parkinson’s disease, etc.); individuals with significant cardiovascular, liver, and kidney diseases, or immune diseases; individuals who continuously use or abuse drugs and alcohol; and pregnant or lactating women from the study. We gathered basic information such as gender and age, as well as clinical testing information like C-reactive protein levels (CRP) from clinical charts.
Screening and genotyping of polymorphisms of LINC-PINT
We selected three single nucleotide polymorphisms (SNPs) in LINC-PINT (rs157916, rs16873842, and rs7801029) based on previous research [22, 23] The minor allele frequency (MAF) of these SNPs was greater than 5% from the global population in the 1000 Genomes Project (http://asia.ensembl.org/). Additionally, we predicted SNP functions (https://regulomedb.org/regulome-search/). The distribution of SNP genotypes in the control group was consistent with Hardy–Weinberg equilibrium (HWE) (p > 0.05). We utilized ethylene diamine tetraacetic acid (EDTA) tubes to collect peripheral blood samples (5 mL) from each participant. We extracted genomic DNA from whole blood samples using the GoldMag Mini Whole Blood Genomic DNA Purification Kit (GoldMag. Co. Ltd., Xi’an, China) according to the manufacturer’s instructions, and measured DNA concentration and purity using a spectrophotometer (NanoDrop 2000; Thermo Fisher Scientific, Waltham, MA, USA). We genotyped SNPs using Agena MassARRAY (Agena Bioscience, San Diego, CA, USA) as per instructions and operation manual [24]. The Agena Bioscience TYPER software (version 4.0) was used to manage and analyze genotyping results and ensure that SNP call rates were maintained at over 95%.
Statistical analysis
The sample characteristics and SNP genotyping data were calculated by the Excel software and SPSS 20.0 statistical software (SPSS, Chicago, IL, USA). Age of subjects was provided as mean ± standard deviation (SD), and compare the differences between cases and controls using independent t-test was used to. The differences in gender distribution between two groups were assessed using chi-square test. HWE was measured by comparing observed genotype frequency with expected genotype frequency in the control group using a chi-square test. We used logistic regression analysis adjusted for age and gender by PLINK 1.9 to evaluate the relationship between LINC-PINT SNPs and LDH risk, and calculated odds ratio (OR) and 95% confidence interval (95% CI) under multiple genetic models (Allele, Co-dominant, Dominant, Recessive, and Additive). We used Sangerbox software (version 3.0) to draw forest plots. To reduce the impact of confounding factors (e.g., gender and age) on statistical results, we performed stratified analyses. Haploview 4.2 software was used to conduct linkage disequilibrium (LD) haplotype block and the strength of linkage between each pair of SNPs was evaluated based on D’ values. SNPStats software was applied to evaluate the correlation between haplotypes in LINC-PINT and LDH risk. The impact of SNP-SNP interactions on LDH risk was analyzed using multi-factor dimensionality reduction (MDR), with the simplest model with maximum testing accuracy and cross-validation consistency (CVC) considered the optimal model. One-way analysis of variance (ANOVA) was used to evaluate the association between SNPs and CRP levels. To reduce false positives in the results, we conducted FDR correction (q = p *n/k) for p-values, with n as the total number of p-values and k as the order in which p-values are sorted from smallest to largest. All statistical analyses were two-sided, with p-values < 0.05 considered significant.
Results
Sample characteristics
The basic information about all study participants is shown in Table 1. A total of 504 patients with LDH (294 males and 210 females) and 500 controls (293 males and 207 females) were recruited for this study. The average ages of the case group and the control group were 49.15 ± 14.89 years and 48.84 ± 14.40 years, respectively. Results showed no significant difference in age (0.849) and gender (0.932) distribution between cases and controls.
Association between LINC-PINT SNPs and LDH risk (overall analysis)
Allele frequencies and basic information on three SNPs (rs157916, rs16873842, and rs7801029) in LINC-PINT are shown in Table 2. We found that all SNPs were consistent with HWE in the control group (p > 0.05), indicating that our samples satisfy random distribution and the SNP genotyping technique is reliable. We confirmed that the G allele of rs157916 was significantly associated with an increased risk of LDH compared to the A allele (OR = 1.23, 95% CI 1.47–1.03, p = 0.019, FDR-p = 0.029). Compared with the C allele, the G allele of rs7801029 was also significantly associated with an increased risk of LDH (OR = 1.39, 95% CI 1.71–1.12, p = 0.002, FDR-p = 0.006). However, no statistically significant association was found between rs16873842 and susceptibility to LDH.
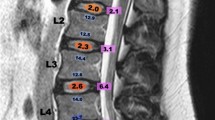
To better understand the relationship between SNPs and LDH risk, samples were divided into different groups based on different types of SNP genotypes for genetic model analysis. The genetic model analyses showed that rs7801029 had a significant association with LDH risk (Fig. 1). The “GG” genotype of rs7801029 (OR = 2.34, 95% CI 1.28–4.271.05, p = 0.005, FDR-p = 0.038) was significantly associated with an increased risk of LDH. Additionally, rs7801029 was also significantly associated with an increased risk of LDH under the recessive (GG vs. CC-GC: OR = 2.13, 95% CI 1.18–3.85, p = 0.012, FDR-p = 0.045) and additive (OR = 1.39, 95% CI 1.13–1.72, p = 0.002, FDR-p = 0.030) models. However, rs157916 was only found to be associated with an increased risk of LDH before FDR correction (GG vs. AA: OR = 1.50, 95% CI 1.05–2.14, p = 0.026; GG-GA vs. AA: OR = 1.37, 95% CI 1.00–1.70, p = 0.046; additive: OR = 1.22, 95% CI 1.02–1.46, p = 0.022). No significant association was found between rs16873842 and LDH risk.
Stratified analysis of the association between LINC-PINT SNPs and LDH risk
Age-stratified analysis (Table 3) showed that rs157916 was associated with an increased risk of LDH in participants aged > 49 before FDR correction (G vs. A: OR = 1.40, 95% CI 1.10–1.80, p = 0.008; GG vs. AA: OR = 1.98, 95% CI 1.17–3.33, p = 0.009; dominant: OR = 1.55, 95% CI 1.06–2.20, p = 0.021; recessive: OR = 1.60, 95% CI 1.01–2.53, p = 0.045; additive: OR = 1.41, 95% CI 1.09–1.81, p = 0.008). Moreover, rs780129 was found to be associated with an increased risk of LDH before FDR correction in subjects aged > 49 (G vs. C: OR = 1.41, 95% CI 1.04–1.91, p = 0.027; dominant: 1.44, 95% CI 1.00–2.07, p = 0.040; additive: OR = 1.41, 95% CI 1.04–1.91, p = 0.027) and aged ≤ 49 (G vs. C: OR = 1.37, 95% CI 1.02–1.84, p = 0.033; recessive: OR = 2.27, 95% CI 1.01–5.10, p = 0.045; additive: OR = 1.37, 95% CI 1.02–1.83, p = 0.035). Additionally, rs16873842 was found to be associated with an increased risk of LDH before FDR correction in subjects aged ≤ 49 under the recessive model (OR = 2.27, 95% CI 1.01–5.10, p = 0.045).
Gender-stratified analysis (Table 4) showed that rs157916 (G vs. A: OR = 1.40, 95% CI 1.10–1.75, p = 0.006, FDR-p = 0.027; GG vs. AA: OR = 1.87, 95% CI 1.15–3.05, p = 0.010, FDR-p = 0.026; dominant: OR = 1.57, 95% CI 1.11–2.21, p = 0.009, FDR-p = 0.027; additive: OR = 1.38, 95% CI 1.09–1.75, p = 0.006, FDR-p = 0.022) and rs780129 (G vs. C: OR = 1.54, 95% CI 1.17–2.02, p = 0.002, FDR-p = 0.036; GC vs. CC: OR = 1.49, 95% CI 1.05–2.10, p = 0.022, FDR-p = 0.044; GG vs. CC: OR = 2.69, 95% CI 1.19–6.07, p = 0.017, FDR-p = 0.038; dominant: OR = 1.59, 95% CI 1.14–2.22, p = 0.005, FDR-p = 0.030; additive: OR = 1.55, 95% CI 1.17–2.05, p = 0.002, FDR-p = 0.018) were associated with an increased risk of LDH in males. However, no significant association was found between LINC-PINT polymorphisms (rs157916, rs16873842 and rs7801029) and risk of LDH in females.
Haplotype analysis
The linkage analysis constructed a haplotype block including three LINC-PINT SNPs (rs157916, rs16873842 and rs7801029) with strong linkage disequilibrium (Fig. 2). The “GGG” haplotype in LINC-PINT was found to be associated with an increased LDH risk compared to the “AGC” haplotype (OR = 1.41, 95% CI 1.14–1.76, p = 0.002, FDR-p = 0.006) (Table 5).
SNP-SNP interaction analysis
The interactions between SNP and SNP are displayed in Fig. 3. Table 6 shows MDR analysis results of the impact of SNP-SNP interactions on LDH risk. The results showed that rs7801029 was the best single-locus model for predicting LDH risk (testing accuracy [TA] = 0.542, cross-validation consistency ([CVC]: 10/10) and the best two-locus model was rs7801029 and rs16873842 (TA = 0.547; CVC: 10/10). Because testing accuracy and CVC values of the two-locus model were the largest, it was the best loci model. And the interaction between rs7801029 and rs16873842 was associated with increased LDH risk (OR = 1.47, 95% CI 1.92–1.13, p = 0.004).
Association between LINC-PINT SNPs and CRP levels among LDH patients
We also investigated the correlation between LINC-PINT SNPs and CRP levels (Fig. 4). Significant association was observed between rs157916 genotypes (p = 0.009). Patients with the GG genotype of rs157916 had significantly higher CRP levels compared to those with the AA genotype (p = 0.017). Meanwhile, a significant association between rs7801029 and CRP levels was also identified. Patients with the CG genotype of rs7801029 had significantly higher CRP levels compared to those with the CC genotype (p = 0.018).
Discussion
In this case–control study, we investigated the association between LINC-PINT polymorphisms and the risk of LDH in the Chinese Han population. The results of our study demonstrate that rs157916 and rs7801029 in the LINC-PINT gene are significantly associated with an increased risk of LDH in overall analysis and males. The “GGG” haplotype in LINC-PINT is found to be associated with an increased LDH risk. The interaction between rs7801029 and rs16873842 is also found to be associated with an increased LDH risk. Additionally, rs157916 and rs7801029 are linked to CRP levels.
LINC-PINT is located on 7q32.3, and it is a transcript induced by p53. Currently, LINC-PINT molecular functions include RNA–protein interactions, miRNA sponging, and epigenetic regulation, which operate in different cellular environments and influence biological processes including DNA damage response, cell cycle and growth arrest, senescence, cell migration and invasion, and apoptosis [25]. Previous studies have found LINC-PINT polymorphisms to be correlated with susceptibility to certain diseases. For instance, LINC-PINT polymorphisms (rs157916 and rs16873842) are associated with reduced risk of steroid-induced osteonecrosis of the femoral head in the Chinese Han population [22]. LINC-PINT SNP rs6971499 is associated with pancreatic cancer risk in the Caucasian population [26]. LINC-PINT SNP rs10228040 is associated with increased susceptibility to sporadic pemphigus foliaceus [21]. LINC-PINT polymorphism rs157928 has a significant association with a reduced risk of high-altitude pulmonary edema [20]. However, there has hitherto been no evidence of a genetic relationship between LINC-PINT and LDH susceptibility in previous studies. This study reported for the first time that LINC-PINT polymorphisms (rs157916 and rs7801029) are significantly associated with LDH risk in the Chinese Han population. Further studies are needed to confirm our findings.
In recent years, the prevalence of LDH has been on the rise, and it is more prevalent in women than in men [27]. As age increases, the elasticity of human tissues gradually decreases, and the muscles in the lower back also begin to relax, leading to a gradual increase in the incidence of lumbar protrusion. During pregnancy and menstruation, women experience hormonal changes in their bodies, leading to more relaxed and supple ligaments, tissues, and joints. Additionally, women’s pelvis is wider, making their center of gravity unstable and more prone to lumbar muscle strain and injury. GSDMC polymorphism rs77681114 is reported to be associated with reduced LDH risk in individuals aged ≥ 49. Rs77681114 has a protective effect on female LDH patients [28]. COL2A1 polymorphism rs740024 is significantly associated with LDH risk in females, and rs6122316 in COL9A3 is correlated with LDH risk in individuals aged > 50 [29]. These findings suggest that genetic susceptibility to LDH differs by age and gender. Our stratified analysis results show that rs157916 and rs7801029 are only significantly associated with an increased risk of LDH in subjects aged > 49 and males, while there is no significant correlation in subjects aged ≤ 49 and females. Thus, we speculate that the impact of age and gender on LDH susceptibility is stronger than rs157916 and rs7801029.
CRP is a biomarker in plasma that indicates whether the human body has an inflammatory response. When inflammation occurs in the human body, the level of CRP will significantly increase. Recent studies have shown a close relationship between CRP levels and the risk of LDH. Additionally, CRP levels can reflect the degree of lumbar inflammatory response [30]. In our study, we find that patients with the GG genotype of rs157916 have significantly higher CRP levels than those with the AA genotype, and patients with the CG genotype of rs7801029 have significantly higher CRP levels than those with the CC genotype. Thus, we speculate that rs157916 and rs7801029 may affect LDH susceptibility by regulating CRP levels.
Our study has several limitations. Firstly, the samples we selected were from the same hospital and may not fully represent the general population. The geographic limitations of sample selection should not be overlooked. This study only explores for the first time the association between three SNPs in the LINC-PINT gene and LDH risk. The association between more LINC-PINT gene polymorphisms and LDH risk is unknown. Therefore, we need to collect a large sample to verify our results. Secondly, the lack of data on other environmental factors, such as lifestyle (smoking and drinking), diet, and BMI, may interfere with the relationship between LINC-PINT polymorphisms and the risk of LDH. Therefore, we need to better control the impact of other factors. Although we have determined the correlation between the LINC-PINT gene and LDH risk, the exact molecular mechanism of LDH has not been fully elucidated, presenting a challenge for future research.
In conclusion, this study reports for the first time that LINC-PINT polymorphisms (rs157916 and rs7801029) were significantly associated with an increased risk of LDH in the Chinese Han population. Our findings suggest that age and gender may influence the susceptibility to LDH more strongly than rs157916 and rs7801029. Rs157916 and rs7801029 may affect LDH susceptibility by regulating CRP levels. Further studies are needed to confirm our results and to elucidate the molecular mechanisms of LDH.
Conclusion
In conclusion, this study suggested that LINC-PINT polymorphisms (rs157916 and rs7801029) were significantly associated with an increased risk of LDH in the Chinese population. Our study may provide a scientific basis for early screening, prevention, pathogenesis, and diagnosis of LDH in the Chinese Han population.
Availability of data and materials
All data included in this study are available upon request by contact with the corresponding author.
Abbreviations
- LDH:
-
Lumbar disc herniation
- SNPs:
-
Single nucleotide polymorphisms
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- MDR:
-
Multi-factor dimensionality reduction
- lncRNAs:
-
Long noncoding RNAs
- MAF:
-
Minor allele frequency
- HWE:
-
Hardy–Weinberg equilibrium
- CRP:
-
C-reaction protein
- LD:
-
Linkage disequilibrium
- CVC:
-
Cross-validation consistency
- FDR:
-
False discovery rate
References
Benzakour T, Igoumenou V, Mavrogenis AF, Benzakour A. Current concepts for lumbar disc herniation. Int Orthop. 2019;43(4):841–51.
Liu S, Wu N, Liu J, Liu H, Su X, Liu Z, et al. Association between ADAMTS-4 gene polymorphism and lumbar disc degeneration in Chinese Han population. J Orthop Res. 2016;34(5):860–4.
Ruschel LG, Agnoletto GJ, Aragão A, Duarte JS, de Oliveira MF, Teles AR. Lumbar disc herniation with contralateral radiculopathy: a systematic review on pathophysiology and surgical strategies. Neurosurg Rev. 2021;44(2):1071–81.
Ma XL. A new pathological classification of lumbar disc protrusion and its clinical significance. Orthop Surg. 2015;7(1):1–12.
Doraisamy R, Ramaswami K, Shanmugam J, Subramanian R, Sivashankaran B. Genetic risk factors for lumbar disc disease. Clin Anatomy. 2021;34(1):51–6.
Aicale R, Tarantino D, Maccauro G, Peretti GM, Maffulli N. Genetics in orthopaedic practice. J Biol Regul Homeostat Agents. 2019;33(1):103–17.
Clos E, Pruna R, Lundblad M, Artells R, Maffulli N. ACTN3’s R577X single nucleotide polymorphism allele distribution differs significantly in professional football players according to their field position. Med Prin Practice Int J Kuwait Univ Health Sci Centre. 2021;30(1):92–7.
Pruna R, Artells R, Lundblad M, Maffulli N. Genetic biomarkers in non-contact muscle injuries in elite soccer players. Knee Surg Sports Traumatol Arthroscopy Off J ESSKA. 2017;25(10):3311–8.
Jacobsen LM, Schistad EI, Storesund A, Pedersen LM, Espeland A, Rygh LJ, et al. The MMP1 rs1799750 2G allele is associated with increased low back pain, sciatica, and disability after lumbar disk herniation. Clin J Pain. 2013;29(11):967–71.
Yang Q, Liu Y, Guan Y, Zhan X, Xiao Z, Jiang H, et al. Vitamin D Receptor gene polymorphisms and plasma levels are associated with lumbar disc degeneration. Sci Rep. 2019;9(1):7829.
Yang X, Li F, Xin D, Huang Z, Xue J, Wang B, et al. Investigation of the STOX1 polymorphism on lumbar disc herniation. Mol Genet Genomic Med. 2020;8(1): e1038.
Hu X, Hao D, Yin J, Gong F, Wang X, Wang R, et al. Association between MIR31HG polymorphisms and the risk of Lumbar disc herniation in Chinese Han population. Cell Cycle. 2022;21(19):2109–20.
Huang Y, Hao J, Liao Y, Zhou L, Wang K, Zou H, et al. Transcriptome sequencing identified the ceRNA network associated with recurrent spontaneous abortion. BMC Med Genomics. 2021;14(1):278.
Jiang SD, Lu J, Deng ZH, Li YS, Lei GH. Long noncoding RNAs in osteoarthritis. Joint Bone Spine. 2017;84(5):553–6.
Ran R, Liao H, Wang Z, Gong C, Zhou K, Zhang H. Mechanisms and functions of long noncoding RNAs in intervertebral disc degeneration. Pathol Res Pract. 2022;235: 153959.
Zhang M, Zhao K, Xu X, Yang Y, Yan S, Wei P, et al. A peptide encoded by circular form of LINC-PINT suppresses oncogenic transcriptional elongation in glioblastoma. Nat Commun. 2018;9(1):4475.
Wang S, Jiang W, Zhang X, Lu Z, Geng Q, Wang W, et al. LINC-PINT alleviates lung cancer progression via sponging miR-543 and inducing PTEN. Cancer Med. 2020;9(6):1999–2009.
Jia M, Li Z, Pan M, Tao M, Wang J, Lu X. LINC-PINT suppresses the aggressiveness of thyroid cancer by downregulating miR-767-5p to induce TET2 expression. Mol Ther Nucleic Acids. 2020;22:319–28.
Wang J, Zhao Q. LncRNA LINC-PINT increases SOCS1 expression by sponging miR-155-5p to inhibit the activation of ERK signaling pathway in rheumatoid arthritis synovial fibroblasts induced by TNF-α. Int Immunopharmacol. 2020;84: 106497.
He X, Zheng J, He Y, Wang Y, Wang L, Bai M, et al. Long non-coding RNA LINC-PINT and LINC00599 polymorphisms are associated with high-altitude pulmonary Edema in Chinese. Arch Bronconeumol. 2020;56(6):360–4.
Salviano-Silva A, Farias TDJ, Bumiller-Bini V, Castro MS, Lobo-Alves SC, Busch H, et al. Genetic variability of immune-related lncRNAs: polymorphisms in LINC-PINT and LY86-AS1 are associated with pemphigus foliaceus susceptibility. Exp Dermatol. 2021;30(6):831–40.
Sun M, Cao Y, Wang T, Liu T, An F, Wu H, et al. Association between LINC-PINT and LINC00599 gene polymorphism and the risk of steroid-induced osteonecrosis of the femoral head in the population of northern China. Steroids. 2021;173: 108886.
Yu Z, Li S, Wang K, Gong D, Qiao X, Wu C. Effects of genetic polymorphisms of LINC-PINT gene on liver cancer susceptibility in the Chinese Han population. Future oncology (London, England). 2023.
Ellis JA, Ong B. The MassARRAY(®) system for targeted SNP genotyping. Methods Mol Biol. 2017;1492:77–94.
Bukhari I, Khan MR, Hussain MA, Thorne RF, Yu Y, Zhang B, et al. PINTology: A short history of the lncRNA LINC-PINT in different diseases. Wiley Interdiscip Rev RNA. 2022;13(4):e1705.
Childs EJ, Mocci E, Campa D, Bracci PM, Gallinger S, Goggins M, et al. Common variation at 2p133, 3q29, 7p13 and 17q25.1 associated with susceptibility to pancreatic cancer. Nat Genet. 2015;47(8):911–6.
Kim YK, Kang D, Lee I, Kim SY. Differences in the incidence of symptomatic cervical and lumbar disc herniation according to age, sex and national health insurance eligibility: a pilot study on the disease’s association with work. Int J Environ Res Public Health. 2018. https://doi.org/10.3390/ijerph15102094.
Wu J, Sun Y, Xiong Z, Liu J, Li H, Liu Y, et al. Association of GSDMC polymorphisms with lumbar disc herniation among Chinese Han population. Int J Immunogenet. 2020;47(6):546–53.
Yang X, Jia H, Xing W, Li F, Li M, Sun K, et al. Multiple variants in collagen genes are associated with the susceptibility to lumbar disc herniation in the Chinese population. European Spine J Off Publ European Spine Soc European Spinal Deformity Soc European Sect Cervical Spine Res Soc. 2020;29(7):1709–16.
Gopireddy R, Rangasamy K, Goni VG, Vatsya P, Behera P, Batra YK, et al. Can high-sensitivity c-reactive protein levels predict functional outcome following epidural steroid injection in patients with lumbar disc disease? Asian spine journal. 2021;15(6):753–60.
Acknowledgements
We thank all individuals for their participation. We are grateful to the hospital staff for collecting blood samples and clinical information.
Funding
This study was supported by the Science and Technology Program of Inner Mongolia Autonomous Region (2021GG0395), the Zhiyuan Talent Program of Inner Mongolia Medical University (ZY0110019), and the Inner Mongolia Autonomous Region Higher Education Science and Technology Research Project (NJZY21603).
Author information
Authors and Affiliations
Contributions
YZ and YW conceived and supervised the study; MB, YY and YW performed the experiments; YW and MB wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the Second Affiliated Hospital of Inner Mongolia Medical University. The experiments were carried out in strict accordance with the principles of the Helsinki declaration. All participants were informed of the research procedures and objectives in written and oral form, and signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, Y., Bai, M., Yu, Y. et al. Association of LINC-PINT polymorphisms with lumbar disc herniation risk among Chinese Han population: a case control study. J Orthop Surg Res 18, 585 (2023). https://doi.org/10.1186/s13018-023-04052-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04052-5