Abstract
Background
In revision surgery with significant segmental acetabular defects, adequate implant selection and fixation methods are critical in determining successful bony ingrowth. Commercially available total hip prosthesis manufacturers generally offer additional multi-hole options of acetabular shells with identical designs for use in revision THAs where screw holes configurations vary from product to product. This study aims to compare the mechanical stability of the two types of acetabular screw constructs for the fixation of acetabular components: spread-out and pelvic brim-focused configurations.
Methods
We prepared 40 synthetic bone models of the male pelvis. In half of the samples with acetabular defects, identical curvilinear bone defects were manually created using an oscillating electrical saw. On the right side, multi-hole-cups in which the direction of the screw holes are centered on the pelvic brim (brim-focused) and, on the left side, multi-hole-cups with the direction of the screw hole spread throughout the acetabulum (spread-out) were implanted into the pelvic synthetic bones. Coronal lever-out and axial torsion tests were performed with a testing machine, measuring load versus displacement.
Results
The average torsional strengths were significantly higher in the spread-out group over the brim-focused group regardless of the presence of the segmental defect of the acetabulum (p < 0.001). But for the lever-out strength, the spread-out group exhibited significantly higher average strength over the brim-focused group for the intact acetabulum (p = 0.004), whereas the results were reversed in the brim-focused group when the defects were generated (p < 0.001). The presence of acetabular defects reduced the average torsional strengths of the two groups by 68.66% versus 70.86%. In comparison, the decrease in the average lever-out strength was less significant for the brim-focused group than the spread-out group (19.87% vs. 34.25%) (p < 0.001).
Conclusion
Constructs of multi-hole acetabular cups with the spread-out screw holes configuration exhibited statistically better axial torsional strength and coronal lever-out strength. With the presence of posterior segmental bone defects, the spread-out constructs demonstrated significantly better tolerance to axial torsional strength. Still, they exhibited inverted results of higher lever-out strength in the pelvic brim-focused constructs.
Similar content being viewed by others
Introduction
Successful acetabular cup fixation in cementless total hip arthroplasty (THA) is achieved by the initial mechanical stability of the implant and subsequent long-term osseointegration. It requires limited micromotion of < 40 μm of the acetabular cup to prevent the formation of fibrocartilaginous membrane and promote adequate membranous bone formation at the bone-implant interface [1]. The initial stability of the acetabular cup in primary THA is gained mainly through press-fitting an implant, with optional augmentation using trans-acetabular screws. The necessity of optional augmentation with trans-acetabular screws remains still controversial [2,3,4,5,6,7,8].
The data from the National Inpatient Sample registry in the USA demonstrated a 28.50% increase in patients receiving revision THA from the years 2006 to 2014 [9]. As the demands for THA have been increasing, a 43–70% increase in revision THA frequency from 2014 to 2030 is anticipated [9,10,11,12,13]. Surgeons often encounter a very challenging situation when performing revision THA and are required to make wise decisions within the limited surgery timeframe. Sufficient fixation is often challenging to achieve, especially in revision THAs with large acetabular bone defects [14]. In situations where the initial stability cannot be gained through press-fitting, rigid construct stiffness aided by additional screw insertion is believed to reduce excessive cup-bone interfacial micromotion, supporting bony ingrowth [15]. In the longer term, threads of the acetabular screw also act as an effective structure for the bony ingrowth to occur [16, 17].
In revision surgery with significant segmental acetabular defects, adequate implant selection and fixation methods are critical in determining successful bony ingrowth. Commercially available total hip prosthesis manufacturers generally offer additional multi-hole options of acetabular shells with identical designs for use in revision THAs where screw hole configurations vary from product to product. Apart from acetabular reconstruction cages with flanges or optional metal augments, the configurations provided are diverse from radially symmetrical configuration [18, 19] to holes concentrated in particular directions [20,21,22] with or without additional rim holes [23]. Still, biomechanical studies regarding the configuration of screw placement are relatively scarce [8, 21, 23].
Therefore, this study aims to compare the mechanical stability of the two types of acetabular screw constructs for the fixation of acetabular components: spread-out and pelvic brim-focused configurations. Using pelvic synthetic bone models, the two types of constructs were tested and compared against models with or without artificially created segmental acetabular defects in terms of axial torsional strength and coronal lever-out strength (Fig. 1).
Materials and methods
Specimen preparation: synthetic bone models
Forty synthetic bone models (Sawbones model 3415–1, Pacific Research Laboratories, Vashon, WA) of the whole pelvis consisting of a short fiber-filled epoxy cortical shell and a 17 pound per cubic feet (PCF) solid rigid polyurethane foam cancellous core were used in this study (Fig. 2). The 4th generation composite synthetic bone model is known to embody the physical properties of human bone in terms of reaming, broaching, and implant fixation. The synthetic bone specimens were divided into two groups: twenty synthetic bone models without acetabular defects and twenty synthetic bone samples with acetabular defects created in the laboratory.
Synthetic bone models of the whole pelvis with bone defects. Among forty synthetic bone specimens, both acetabuli of twenty specimens were cut with an electrical saw to generate posterior segmental defects (a), with a maximum width of 20 mm in the posterior 9’o-clock direction (yellow dotted line). The anterior view of the pelvis shows visible posterior bone defects (b), and the posterior view with implants inserted is demonstrated with the posterior overhang of the acetabular shells (c)
Specimen preparation: acetabular cup fixation and defect generation
Acetabular reaming was done by a senior high-volume arthroplasty surgeon. The reaming size was raised to 59 mm then an acetabular cup with an outer diameter size of 58 mm was inserted, establishing one-millimeter over-reaming to intentionally exclude press-fitting of the acetabular cup. In this manner, forty acetabular cups were implanted into twenty synthetic bone specimens without any acetabular defects. For the preparation of forty acetabuli in half the samples with acetabular defects, identical curvilinear bone defects were manually created using an oscillating electrical saw (Fig. 2a, b). This segmental defect (Paprosky classification type II) was designed to have a maximum width of 20 mm at the posterior side of the acetabular wall, which ends with 10 mm width defects at 12’ o-clock (superior) and 6` o-clock (inferior) directions (Fig. 2a).
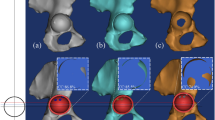
On each right acetabulum, multi-hole acetabular cups (G7® Acetabular System OsseoTi Multi-hole, Zimmer Biomet, Warsaw, IN, USA) with screw holes in the spread-out configuration were implanted (Fig. 3a) with four conventional acetabular screws from the same manufacturer with following lengths: 20 mm, 30 mm, 30 mm, 30 mm. For each right acetabulum of all 40 synthetic bone specimens, multi-hole acetabular cups (Bencox® Hybrid cup, Corentec, Cheonan, Korea) in which the direction of the screw holes are focused on the superior central areas of the cup or the pelvic brim were fixed using four acetabular screws vice versa (Fig. 3b): 30 mm, 30 mm, 35 mm, 40 mm. The resulting acetabular screw configuration was confirmed under the image intensifier (Fig. 3c). Detailed specifications of the two multi-hole cups used in the study are described in Table 1.
Acetabular cup fixation methods for the preparation for mechanical testing. After creating intentional defects to both acetabuli of the sawbones, four trans-acetabular screws were inserted in the configuration as seen above. Acetabular components containing spread-out configuration screw holes were inserted with screws to the acetabulum (a), and acetabular components containing brim-focused configuration screw holes to the left acetabulum (b). The resulting screw configuration was confirmed using the image intensifier in the laboratory (c)
Biomechanical testing: axial torsional strength
Utilizing the mechanical testing machine (MTS 858, MTS system Corp., MN, USA), the coronal lever-out and axial torsion tests were performed to measure the lever-out and torsional load required to displace the fixed implant. Testing was conducted in a controlled environment of 37 °C room temperature and 30% humidity. Axial torsional strength and coronal lever-out tests were done with and without the acetabular defect for each specimen.
To perform the axial torsional strength test, specimens were firmly mounted on the testing machine to place the acetabular cup perpendicular to the vertical axis (Fig. 4a, b). 500 N of Compressive load (= pre-load, for structural stabilization) is applied. The test was conducted by applying a torsional load at a speed of 0.038 rad/min (2.18/min). As a result, maximum sustained torque was obtained. The results were recorded into load–displacement or torque–angle curves (Fig. 6a, b). The maximum sustained torque (N m) was determined from the curves for each implant specimen.
Biomechanical testing: coronal lever-out test
In an identical environment to the torsional strength test, the coronal lever-out tests were conducted using the mechanical testing machine. The specimen was firmly mounted, and a jig was connected to the center of the fixed implant (Fig. 5a, b). The load was applied at the other side of the jig at a point 200 mm distant from the center of the implant. The degree (θ) of displacement was calculated by the arctangent of displacement length over the moment arm, where the moment of force is the product of the moment arm, and the magnitude of the force applied. Variables were recorded into a load–displacement curve and then converted into a moment-angular displacement curve to establish an implant’s lever-out strength (N m) (Fig. 6c, d).
Representative results of the torque–angle curve and moment-angular displacement. To establish the axial torsional strength, torque–angle curves were recorded for each of the brim-focused constructs (a) and the spread-out constructs (b) which were implanted in acetabuli with the posterior segmental defect. Likewise, to establish the lever-out strength, moment-angular displacement curves were recorded for each of the brim-focused constructs (c) and spread-out constructs (d)
Statistical analyses
Paired data were gained from each synthetic bone pelvis that contains two acetabuli implanted with a spread-out configuration cup for one acetabulum and a brim-focused configuration cup for the other. Observation data were grouped by defect status, and test types were then tested for normality using the Kolmogorov–Smirnov test and the Shapiro–Wilk test. Paired T-tests were used for all groups of continuous variables: the torsional and lever-out strength. p values under 0.05 were considered statistically significant. All statistical analyses were conducted using SPSS (version 26.0, SPSS Inc., Chicago, IL, USA).
Results
Among 40 synthetic bone specimens (80 acetabuli), 38 synthetic bone specimens (76 acetabuli) were adequately tested for recording and eligible for statistical analyses. Two specimens (four acetabuli) were damaged by trial and error, which rendered then unsuitable. One model without defect was cracked during an acetabular cup fixation, and the other specimen was unfit for testing due to excess damage that occurred while creating the defect.
The results of recordings from the tests for the comparison of spread-out and brim-focused acetabular screw configuration in each setting are as in Table 2.
The average torsional strengths were significantly higher in the spread-out group over the brim-focused group regardless of the presence of the segmental defect of the acetabulum (p < 0.001). But for the lever-out strength, the spread-out group exhibited significantly higher average strength over the brim-focused group for the intact acetabulum (p = 0.004); conversely, the brim-focused group with the defects exhibited higher sustained torque (p < 0.001).
Both the torsional strength and the lever-out strength drastically declined with the relatively poor fixation power of the acetabular cup. The percent reductions by the presence of acetabular defects were similar for the average torsional strengths of the two groups (68.66% vs. 70.86%). In comparison, the decrease in the average lever-out strength was less significant for the brim-focused group than the spread-out group (19.87% vs. 34.25%) (p < 0.001).
Discussion
Increasing revision THA urges surgeons to often cope with challenging situations and make difficult decisions to achieve the long-term stability of an acetabular component successfully. Nevertheless, there have been promising reports of gaining osseointegration from cementless porous-coated implants for revision THA with an 88–98% 10-year survivorship [24,25,26,27,28]. But it is often difficult to obtain initial stability in resulting revision settings, particularly with acetabular bone defects, where supplemental screw fixations can play an essential role in maximizing the stability and enhancing the contact of the host bone-implant interface [29].
Although it is recommended that same-size or line-to-line reaming with additional screw fixation is adequate for revisional THAs with limited or fragile bone stock [30, 31], sufficient press-fitting is often unachievable. Besides, both generic acetabular components used in this study were manufactured using the same porous titanium plasma spray coating for the surface treatment; differences in the microscopic specification, as well as the number of screw holes, result in a discrepancy in the effective surface area even with the identical outer diameter of 58 mm. Thus, in this study, one-millimeter over-reaming was done prior to screw fixation of all samples to minimize the effect of press-fitting on mechanical cup stability and focus on the comparison of spread-out and brim-focused screw constructs. Even if it can be vaguely thought that the more significant number of effective acetabular screws inserted, the better stability we can gain, clarifying configurations with superior stability in certain conditions would help aid successful revision surgery.
In a biomechanical study, Hsu et al. [20] reported that an acetabular cup with pelvic brim-focused screw hole configuration induces a very stable region at the superior central region, though having little effect on reducing the peak micromotion at the opposite rim edge. In another study, a revision cup with eccentric screw holes provided stability by decreasing the hip rotation center, aiding better biomechanical function [21]. Similarly, by using the Stryker Orthopaedic Modeling and Analytics (SOMA) database [32], Faizan et al. [23] suggested that a modified eccentric jumbo shell with an offset center of rotation exhibit several advantages over generic acetabular shells, which includes providing adjunctive screw holes to the superior rim directed into the posterior column of the pelvis. The acetabular screws in the posterior column or inferior ischium are known to provide better stability than acetabular dome screws alone [24]. But to our knowledge, a direct comparison between two generic acetabular components with different modes of screw hole configuration has yet to be reported.
As observed in the results of this study, mechanical testing for the implants inserted into intact acetabuli demonstrated that the spread-out configuration cup showed significantly better stability over the pelvic brim-focused configuration cup by 15.1% (26.27 ± 2.12 vs. 22.82 ± 1.81, p < 0.001) in axial torsional strength and 23.8% (8.23 ± 1.26 vs. 6.65 ± 1.58, p < 0.001) in coronal lever-out strength. But surprisingly, the presence of posterior segmental defect exhibited mixed results for the two cups. The spread-out construct was significantly more stable in axial torsional strength by 16.5% (p = 0.004), whereas the brim-focused construct was significantly better in coronal lever-out strength by 4.5% (p < 0.001). In other words, while a spread-out construct is generally an excellent choice for the intact acetabulum, selecting an acetabular cup with a brim-focused screw hole configuration might become a feasible option when a substantial posterior segmental bone defect is present. Likewise, the percent reduction in average coronal lever-out strength (19.87% vs. 34.25%) by the presence of the defect was also reduced in the brim-focused group.
In this study, the spread-out configuration of acetabular screw placement showed superior stability than the pelvic brim-focused configuration in the absence of segmental bone defects. However, when planning revision THA with significant segmental acetabular defects or insufficient bone stock, it would be reasonable to consider using acetabular cups with brim-focused screw hole configuration rather than adhering to the use of cups with spread-out configuration. Nevertheless, buttress graftings such as adjunctive metal buttress augment or bone block allografting for the bone deficit should be considered first to increase the chances of successful surgery.
The limitation of this study is that it is an in vitro biomechanical study using synthetic bone model samples of a limited number of samples. Second, the lengths of the four acetabular screws used to fix the components differ between the two groups, which would considerably affect the discrepancies between the initial stability. This is because when the same length was used, the screw pierced the cortex. The choice of screw length was to insert the most extended screw within the limit of not penetrating the cortex. Nevertheless, this study is not to clarify the effects of the configuration of constructs in the same condition but to compare the mechanical stability of suitable constructs for each generic acetabular shell. Effects of the number of screws, their length, and directions would be dealt with in future studies using computational analysis utilizing the finite element models. Additional biomechanical and cadaveric investigations are required to examine the impacts that vary with the size and location of the bone defects, as well as to compare alternative shell designs that feature an eccentric configuration or supplementary screw holes in the superior rim.
Conclusion
In this biomechanical study, for synthetic bone models with intact acetabuli, constructs of multi-hole acetabular cups with the spread-out screw holes configuration exhibited statistically better axial torsional strength and coronal lever-out strength over the pelvic brim-focused constructs. In the presence of posterior segmental bone defects, the spread-out constructs demonstrated statistically better tolerance to axial torsional strength. However, the brim-focused constructs showed higher lever-out strength than the spread-out constructs. Therefore, in planning revision THA in a hip with significant acetabular segmental bone defects, adjunctive brim-focused screws may aid initial mechanical stability regarding lever-out strength, in addition to essential torsional stability gained by the spread-out configuration of acetabular screws.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Burke D, Bragdon C, Lowenstein J. Mechanical aspects of the bone-porous surface interface under known amounts of implant motion: an in vivo canine study. Trans 39th Annu ORS. 1993;18:470.
Hadjari MH, Hollis JM, Hofmann OE, Flahiff CM, Nelson CL. Initial stability of porous coated acetabular implants: the effect of screw placement, screw tightness, defect type, and oversize implants. Clin Orthop Relat Res. 1994;307:117–23.
Richard Illgen I, Rubash HE. The optimal fixation of the cementless acetabular component in primary total hip arthroplasty. JAAOS-J Am Acad Orthop Surg. 2002;10:43–56.
Otten VT, Crnalic S, Röhrl SM, Nivbrant B, Nilsson KG. Stability of uncemented cups—long-term effect of screws, pegs and HA coating: a 14-year RSA follow-up of total hip arthroplasty. J Arthroplasty. 2016;31:156–61.
García-Rey E, García-Cimbrelo E, Cruz-Pardos A. Cup press fit in uncemented THA depends on sex, acetabular shape, and surgical technique. Clin Orthop Relat Res. 2012;470:3014–23.
Clarke HJ, Jinnah RH, Warden KE, Eng MB, Cox QG, Curtis MJ. Evaluation of acetabular stability in uncemented prostheses. J Arthroplasty. 1991;6:335–40.
Perona PG, Lawrence J, Paprosky WG, Patwardhan AG, Sartori M. Acetabular micromotion as a measure of initial implant stability in primary hip arthroplasty: an in vitro comparison of different methods of intial acetabular component fixation. J Arthroplasty. 1992;7:537–47.
Hsu J-T, Chang C-H, Huang H-L, Zobitz ME, Chen W-P, Lai K-A, et al. The number of screws, bone quality, and friction coefficient affect acetabular cup stability. Med Eng Phys. 2007;29:1089–95.
Patel I, Nham F, Zalikha AK, El-Othmani MM. Epidemiology of total hip arthroplasty: demographics, comorbidities and outcomes. Arthroplasty. 2023;5:1–9.
Kremers HM, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Jt Surg Am. 2015;97:1386.
Singh JA, Yu S, Chen L, Cleveland JD. Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J Rheumatol. 2019;46:1134–40.
Schwartz AM, Farley KX, Guild GN, Bradbury TL Jr. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79–85.
Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. JBJS. 2018;100:1455–60.
Volpin A, Konan S, Biz C, Tansey R, Haddad F. Reconstruction of failed acetabular component in the presence of severe acetabular bone loss: a systematic review. Musculoskelet Surg. 2019;103:1–13.
Park B, Liporace F, Marwin S. Managing acetabular defects in total hip arthroplasty. Bull NYU Hosp Jt Dis. 2017;75:37.
Pidhorz LE, Urban RM, Jacobs JJ, Sumner DR, Galante JO. A quantitative study of bone and soft tissues in cementless porous-coated acetabular components retrieved at autopsy. J Arthroplasty. 1993;8:213–25.
Sumner DR, Jasty M, Jacobs JJ, Urban RM, Bragdon CR, Harris WH, et al. Histology of porous-coated acetabular components: 25 cementless cups retrieved after arthroplasty. Acta Orthop Scand. 1993;64:619–26.
Jauregui JJ, Pierce TP, Elmallah RK, Cherian JJ, Delanois RE, Mont MA. Dual mobility cups: an effective prosthesis in revision total hip arthroplasties for preventing dislocations. Hip Int. 2016;26:57–61.
Höch A, Reise R, Pieroh P, Heyde C-E, Fakler JKM, Schleifenbaum S. Primary stability of multi-hole cups compared to plate osteosynthesis in osteoporotic anterior column and posterior hemi-transverse acetabular fractures—a biomechanical comparison. PLoS ONE. 2022;17:e0270866.
Hsu J-T, Lai K-A, Chen Q, Zobitz ME, Huang H-L, An K-N, et al. The relation between micromotion and screw fixation in acetabular cup. Comput Methods Programs Biomed. 2006;84:34–41.
Zhang Y, Ma H, Liu Y, Shen J, Zhang B, Zhou Y. The optimal screw-hole positions of the eccentric revision cup based on a morphological study. J Orthop Surg Res. 2022;17:386.
Civinini R, Lepri AC, Carulli C, Matassi F, Villano M, Innocenti M. Patients following revision total hip arthroplasty with modular dual mobility components and cobalt-chromium inner metal head are at risk of increased serum metal ion levels. J Arthroplasty. 2020;35:S294–8.
Faizan A, Black BJ, Fay BD, Heffernan CD, Ries MD. Comparison of head center position and screw fixation options between a jumbo cup and an offset center of rotation cup in revision total hip arthroplasty: a computer simulation study. J Arthroplasty. 2016;31:307–11.
Meneghini RM, Stultz AD, Watson JS, Ziemba-Davis M, Buckley CA. Does ischial screw fixation improve mechanical stability in revision total hip arthroplasty? J Arthroplasty. 2010;25:1157–61.
Della Valle CJ, Berger RA, Rosenberg AG, Galante JO. Cementless acetabular reconstruction in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;420:96–100.
Templeton JE, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Revision of a cemented acetabular component to a cementless acetabular component: a ten to fourteen-year follow-up study. JBJS. 2001;83:1706–11.
Hallstrom BR, Golladay GJ, Vittetoe DA, Harris WH. Cementless acetabular revision with the Harris-Galante porous prosthesis: results after a minimum of ten years of follow-up. JBJS. 2004;86:1007–11.
Sternheim A, Abolghasemian M, Safir OA, Backstein D, Gross AE, Kuzyk PR. A long-term survivorship comparison between cemented and uncemented cups with shelf grafts in revision total hip arthroplasty after dysplasia. J Arthroplasty. 2013;28:303–8.
Latimer HA, Lachiewicz PF. Porous-coated acetabular components with screw fixation. Five to ten-year results. J Bone Jt Surg. 1996;78:975–81.
Tabata T, Kaku N, Hara K, Tsumura H. Initial stability of cementless acetabular cups: press-fit and screw fixation interaction—an in vitro biomechanical study. Eur J Orthop Surg Traumatol. 2015;25:497–502.
Kwong LM, O’Connor DO, Sedlacek RC, Krushell RJ, Maloney WJ, Harris WH. A quantitative in vitro assessment of fit and screw fixation on the stability of a cementless hemispherical acetabular component. J Arthroplasty. 1994;9:163–70.
Banerjee S, Faizan A, Nevelos J, Kreuzer S, Burgkart R, Harwin SF, et al. Innovations in hip arthroplasty three-dimensional modeling and analytical technology (SOMA). Surg Technol Int. 2014;24:288–94.
Funding
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea government (MSIT) (No. 2018R1C1B6002653). Also, the APC was supported by the Technology Innovation Program (Project No. 20012931) funded By the Ministry of Trade, Industry & Energy (MOTIE), Korea.
Author information
Authors and Affiliations
Contributions
HJN, WLJ, JHB, YWL, SYK, HCP, and SMA made substantial contributions to research design, or the acquisition, analysis or interpretation of data. HJN, JHB, and YWL contributed to drafting the paper or revising it critically. HJN, WLJ, JHB, YWL, SYK, HCP, and SMA involved in approval of the submitted and final versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since this is basic research, it did not receive ethical approval.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nam, HJ., Lim, YW., Jo, WL. et al. Is the construct stability of the acetabular cup affected by the acetabular screw configuration in bone defect models?. J Orthop Surg Res 18, 354 (2023). https://doi.org/10.1186/s13018-023-03845-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03845-y