Abstract
Background
Rigid fixation, represented by titanium rods, is a widely used fixation technique for lumbar fusion. However, this technique carries the risk of degeneration of adjacent segments. In recent years, the semi-rigid fixation technique represented by PEEK rods has gradually matured, and its effectiveness has been verified by numerous studies. The aim of this study was to systematically evaluate the effectiveness of these two fixation modalities in posterior lumbar fusion surgery.
Methods
Studies meeting the inclusion criteria were searched in PubMed, Cochrane Library, ScienceDirect, Embase, CNKI, and Wanfang databases. After data extraction and quality assessment of included studies, meta-analysis was performed using STATA 15.1 software. The protocol for this systematic review was registered on INPLASY (2021110049) and is available in full on the inplasy.com (https://inplasy.com/inplasy-2021-11-0049/).
Results
Fifteen relevant studies were finally included, including eight prospective studies and seven retrospective studies. The results of meta-analysis showed that in ODI (P = 0.000), JOA score (P = 0.017), VAS score for lower limb pain (P = 0.027), fusion rate of bone graft at week 12 (P = 0.001), fusion rate of bone graft at last follow-up (P = 0.028), there was a statistical difference between the two groups. The PEEK rod group was superior to the titanium rod group in the above aspects. While in VAS score for LBP (P = 0.396), there was no statistical difference between the two groups.
Conclusion
Both PEEK rods and titanium rods are effective fixation materials in lumbar fusion surgery. PEEK rods may be superior to titanium rods in improving postoperative function and improving bone graft fusion rates. However, given the limitations of this study, whether these conclusions are applicable needs further research.
Similar content being viewed by others
Background
Lumbar fusion is a commonly used surgical procedure for the treatment of degenerative lumbar spine diseases. And rigid fixation represented by titanium rods is a widely used fixation method in lumbar fusion surgery. It can provide strong stability to the lumbar spine and facilitate implant fusion. However, rigid fixation can significantly alter the distribution of lumbar spine loading, leading to adjacent segment degeneration (ASD) [1,2,3].
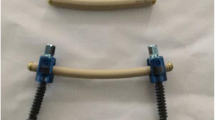
To address this problem, semi-rigid fixation systems represented by polyetheretherketone (PEEK) rods, an inert, semi-crystalline thermoplastic polymer with biocompatible properties [4], have been clinically applied with a stable chemical structure, minimal toxicity, and good mechanical properties such as high strength, good wear resistance, and fatigue properties [5,6,7]. PEEK materials were first used in spinal surgery in the form of intervertebral fusion devices [8, 9], and since 2007, PEEK rods have been used for dynamic stabilization [5, 10]. After more than a decade of development and improvement, the effectiveness and safety of PEEK rods have been validated by several biomechanical and clinical studies.
Despite these advantages, there are still few studies that systematically compare the effectiveness of PEEK rods and titanium rods in lumbar fusion surgery. Although Selim et al. [11] performed a systematic review in 2018, they included only five studies, four of which were retrospective, and the studies were conducted before 2016 with a small sample size (177 patients, 156 in the PEEK group and 21 in the titanium group). Therefore, we performed a larger sample size meta-analysis with the aim of comprehensively evaluating the effectiveness of PEEK rods versus titanium rods in posterior lumbar fusion surgery to provide stronger evidence to support clinical decision making.
Methods
This meta-analysis was performed according to the Cochrane Handbook [12], and as it is a systematic review of published studies, ethical approval is not required.
Inclusion and exclusion criteria
Studies that met the following inclusion criteria were included: (1) Published clinical prospective or retrospective controlled studies. (2) The subjects were patients who received lumbar fusion due to lumbar degenerative diseases. The age, gender and nationality of the patients were not limited. (3) PEEK rod-pedicle screw internal fixation-intervertebral bone graft fusion was used as an intervention measure, and titanium rod-pedicle screw internal fixation-intervertebral bone graft fusion was used as a control measure.
The studies were excluded according to the following criteria: (1) The subjects were combined with lumbar spine trauma, fracture, tumor, infection or combined with coagulation dysfunction, thrombosis, mental system diseases, etc. (2) The research subjects had received lumbar spine surgery. (3) Biomechanics and animal studies. (4) Non-fusion surgery, or a combination of fusion and non-fusion surgery.
Search strategies
After determining the inclusion and exclusion criteria for this study, two researchers independently searched multiple databases, including PubMed (1966–May 1, 2022), Cochrane Library (1966–May 1, 2022), ScienceDirect (1980–May 1, 2022), Embase (1980–May 1, 2022), China National Knowledge Infrastructure (CNKI) (1980–May 1, 2022) and Wanfang Database (1980–May 1, 2022).
We used the following search terms: polyetheretherketone rod, PEEK rod, Semi-rigid fixation, radiolucent spinal implant, and used the Boolean operators AND or OR. The retrieved studies were gradually screened by two researchers based on title, abstract and full text. After identifying included articles, we traced their references to identify potential articles.
Data extraction
After the initial screening and secondary screening of the literatures in strict compliance with the established inclusion and exclusion criteria, two independent researchers extracted data from the literatures that met the requirements, and sent them to a third researcher for inspection and verification after the extraction was completed. Any disagreement about the included studies was reached through discussion among all investigators. The main data extracted in this study included: first author's name, year of publication, sample size, patient sex ratio, mean age, intervention method, country, study type, follow-up time, and clinical outcomes.
Quality assessment
In this study, the Cochrane Risk of Bias Tool [13] was used to evaluate the quality of prospective studies, which included seven assessments: random sequence generation, allocation concealment, blinding of performers and outcome assessors, data integrity, whether there is selective reporting and other aspects of bias. The risk of bias for each aspect was judged as low risk, high risk, or unknown risk, indicated by symbols with different colors. This work was done by two researchers using Review Manager software (RevMan 5.3).
For included retrospective controlled studies, we used the MINORS scale for quality assessment. The scale has 12 items in total, with 0–2 points for each item, with a total score of 24 points. 0 means not reported; 1 means reported but insufficient information; 2 means reported and provided sufficient information.
Data analysis
We performed statistical analysis using STATA software (version 15.1). Continuous variables were reported as mean difference (MD) and 95% confidence interval (CI), while dichotomous variables were reported as odds ratio (OR) and 95% CI. Statistical heterogeneity was judged according to the I2 statistic. The greater the I2, the greater the heterogeneity. If there was heterogeneity in this study (I2 ≥ 50%), a random-effects model was used; otherwise, a fixed-effects model (I2 < 50%) was used. In this study, differences were considered statistically significant when P < 0.05.
Results
Search result
This meta-analysis has been reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Statement [14]. A total of 255 relevant studies were identified from the electronic database, and 178 studies were obtained after deduplication. According to the titles and abstracts of these studies, 21 studies related to this study were further obtained according to the inclusion and exclusion criteria. After careful full-text evaluation of these studies, 15 studies [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29] were finally included in the final comprehensive analysis. The literatures screening flowchart is shown in Fig. 1, and the basic characteristics of the included studies are shown in Table 1.
Quality assessment
Except for Huang et al. [22] 's study using the random number table for randomization, the remaining 7 prospective studies did not mention randomization, allocation concealment, and blinding, so the risks in these three aspects were unknown. We speculate that this may be related to the particularity of surgical treatment and ethical requirements. Before performing surgery, the patient's right to know must be guaranteed, and the patient's personal wishes must be fully listened to, so it is difficult to implement randomization, allocation concealment, and blinding. In terms of selective reporting, since the study by Li et al. [18] did not report data on the rate of bone graft fusion, it was considered high risk, and the rest of the studies were low risk. No patients were withdrawn or lost to follow-up in all studies, and the data were complete. As shown in Fig. 2.
The seven included retrospective studies did not adequately describe the coherence of included patients, the objectivity of outcome indicators, whether the sample size was estimated, and whether the control group was synchronized. Therefore, 1 point is awarded for each of these aspects. See Table 2 for details.
Results of the meta-analysis
ODI
Nine studies compared ODI scores between PEEK rods and titanium rods, as shown in Fig. 3. The heterogeneity test showed that there was significant heterogeneity between studies (P = 0.004, I2 = 64.3%), so a random-effects model was used to analyze the data. The combined results showed that the difference between two groups was statistically significant (P = 0.000).The PEEK rod group was superior to the titanium rod group.
JOA score
Eight studies compared the JOA scores between the PEEK rod group and the titanium rod group, as shown in Fig. 4. The heterogeneity test showed that there was significant heterogeneity between studies (P = 0.000, I2 = 79.5%), so a random-effects model was used for analysis. The combined results showed that the difference between the two groups was statistically significant (P = 0.017). The PEEK rod group was superior to the titanium rod group.
VAS score for LBP
Six studies compared the VAS scores for LBP between the PEEK rod group and the titanium rod group, as shown in Fig. 5. The heterogeneity test showed that the heterogeneity between studies was significant (P = 0.000, I2 = 84.8%), so a random-effects model was used for analysis. The combined results showed that the difference between the two groups was not statistically significant (P = 0.396).
VAS score for lower limb pain
Five studies compared the postoperative lower limb VAS scores between the PEEK rod group and the titanium rod group, as shown in Fig. 6. The heterogeneity test showed that the heterogeneity between studies was not significant (P = 0.306, I2 = 17.1%), so a fixed-effects model was used for analysis. The combined results showed that the difference between the two groups was statistically significant (P = 0.027). The PEEK rod group was better than the titanium rod group.
Fusion rate of bone graft at week 12
Eight studies compared the bone graft fusion rate at week 12 between PEEK rods and titanium rods, as shown in Fig. 7. The heterogeneity test showed that there was no significant heterogeneity between studies (P = 0.077, I2 = 45.3%), so a fixed-effects model was used for analysis. The combined results showed that the difference between the two groups was statistically significant (P = 0.001). The PEEK rod group was better than the titanium rod group.
Fusion rate of bone graft at last follow-up
Twelve studies compared the fusion rate of bone graft between PEEK rods and titanium rods at last follow-up, as shown in Fig. 8. The heterogeneity test showed that there was no significant heterogeneity between studies (P = 0.299, I2 = 18.1%), so a fixed-effects model was used for analysis. The combined results showed that the difference between the two groups was statistically significant (P = 0.028). The PEEK rod group was better than the titanium rod group.
Sensitivity analysis
By excluding the studies one by one, we conducted a sensitivity analysis on all the outcome indicators, and drew sensitivity analysis graphs. It can be seen from the graphs that when the studies such as Pang et al. [26], Li et al. [18], and Tang et al. [19] are excluded, the combined results changed significantly, suggesting that the three studies may be a major source of heterogeneity, as shown in Figs. 9, 10, 11, 12, 13 and 14.
Publication bias
We used Egger's method and Begg's method to detect publication bias. The test results showed that ODI (P = 0.167), JOA score (P = 0.491), VAS score for LBP (P = 0.301), VAS score for lower limb pain (P = 0.516), fusion rate of bone graft at week 12 (P = 0.138), fusion rate of bone graft at last follow -up (P = 0.426) had no publication bias (P > 0.05), as shown in Figs. 15, 16, 17, 18, 19 and 20. It indicates that there is no selective reporting and publication of positive results in the included studies.
Discussion
In this study, we identified 8 prospective studies and 7 retrospective studies including 779 patients to evaluate the effect of PEEK rods and titanium rods in lumbar fusion surgery. The results of the meta-analysis showed that there was no statistical difference between the two groups in the VAS score of LBP. There were statistical differences between the two groups in terms of ODI, JOA score, VAS score of lower limb pain, bone graft fusion rate at 12 weeks, and bone graft fusion rate at the last follow-up. In these aspects, the PEEK rod group was better than the titanium rod group.
Compared with the JOA score, in addition to the basic upper and lower extremity function evaluation, ODI also adds the evaluation of the patient's social life, sex, sleep, travel, etc., and the evaluation of the living ability is more detailed and comprehensive. Compared with rigid fixation with titanium rods, semi-rigid fixation with PEEK rods allows a greater ROM of the lumbar spine. Finite element analysis [30] showed that the ROM values of PEEK rods in axial rotation, lateral bending and buckling were increased by 3.7, 7.2 and 2.15 times compared with titanium rods, respectively. This helps to reduce the stiffness and restraint of postoperative patients during daily activities such as putting on and taking off clothes, standing, walking, washing, etc., which is beneficial to improve the comfort of patients, and also reduces the difficulty of postoperative rehabilitation training.
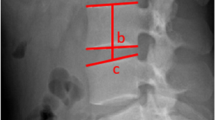
In terms of bone graft fusion rate, our study showed that the bone graft fusion rate of PEEK rod group was higher than that of titanium rod group at the 12th week after operation or at the last follow-up, indicating that semi-rigid fixation may be more beneficial to bone graft fusion. This is contrary to our intuition, because in our perception, the strong fixation of titanium rods seems to represent a higher implant fusion rate. Since the elastic modulus (3.2 GPa) of PEEK material is between cortical bone and cancellous bone and significantly lower than that of titanium (114 GPa) [31], it is more mechanically compliant to the spine. It can better mimic the load distribution in the physiological environment of the lumbar spine. Under physiological loading conditions, the PEEK rod structure can increase the front column load by about 75% compared with the titanium rod [32]. Increased loading of the anterior column creates greater stress on the bone graft area and also allows for greater contact between the endplate and the bone graft. Coupled with the micro-motion generated by the elastic rod in the bone graft area, it may be the reason why PEEK rods promote the fusion of the bone graft [33,34,35].
In terms of VAS for LBP, there was no statistical difference between the two groups, indicating that semi-rigid immobilization may not bring more pain in the surgical area while increasing the ROM of the lumbar spine after surgery. The PEEK rod group appeared to be superior to the titanium rod group in VAS for lower limb pain, which was not explained in all included studies. Qi et al. [21] believed that there is no difference in the degree of intervertebral space height loss between PEEK rods and titanium rods, and both can meet the requirements of intervertebral space height. Biswas et al. [30] believed that for pedicle screw fixation, no matter what kind of rod was used, the height of the intervertebral foramen did not change significantly, and it would not interfere with the nerve root. We believe that this may be related to the greater lumbar ROM and better spinal compliance afforded by the PEEK rods. We believe that a more comfortable postoperative feeling will encourage patients to perform more rehabilitation and daily activities, which will help promote the reduction of nerve edema and inflammation, thus reducing postoperative lower extremity pain.
Reducing the incidence of ASD is the main purpose for which PEEK rods were created. This mechanism can be broadly explained in two ways: one is the increase of fixed segment activity, which reduces the compensatory overactivity of adjacent segments; the other is the load distribution pattern that is closer to the physiological state [1,2,3]. Unfortunately, none of the studies we included reported the occurrence of ASD, which we believe may be related to the short follow-up period. Of the 15 included studies, only Sun et al. [16] had a follow-up time of 4 years, and the follow-up time of the rest of the studies was within 3 years. In our opinion, this does not seem to be enough to observe the occurrence of ASD.
In terms of screw stability, according to the study of Gornet et al. [32], the PEEK rods can reduce the load of the bone-screw interface by about 25% while increasing the load of the anterior column, reducing the stress shielding, thereby reducing the risk of screw loosening, especially in osteoporotic bone [36]. Wu et al. [37] observed denser and thicker trabecular bone around the screw in the PEEK rod group in the sheep cervical fusion model, and believed that the PEEK rod could produce better biomechanical distribution and promote the growth of trabecular bone around the screw. In terms of strength and durability, although it has been suggested [38] that the ratio of peak stress to material yield stress of PEEK rods in physiological state is higher than that of titanium rods, which will increase the risk of rod fracture. But more studies hold the exact opposite view. Study of Agarwal et al. [39]showed that the motion data of PEEK rods before and after fatigue were not significantly different from those of titanium rods with significantly higher motion after fatigue than before. Moreover, studies [40]have shown that PEEK rods can withstand static and fatigue angular displacements that exceed five times that of the cadaveric test recommendations without fracture, torsion, yield and plastic deformation in static and dynamic compression bending tests and torsional tests. Wang et al. [35] tested PEEK rods of various diameters in a canine model, and the results showed that even the thinnest PEEK rod (2.0 mm, 197N) had a significantly higher yield load than the lumbar spine stress (17.5N). In addition to the above studies, there are several biomechanical studies that suggest that the stability provided by PEEK rods in posterior lumbar fusion is not significantly different from that of titanium rods [30, 32, 41]. Moreover, PEEK materials can also customize stiffness through carbon fiber reinforcements, which may have advantages over conventional materials [42].
In terms of adverse events, Hirt et al. [43] reviewed 462 patients and showed that the PEEK rod group was less likely to be readmitted due to adverse events. Ross et al. [44] reviewed 108 patients and also showed a lower complication rate. None of the 15 studies we included reported any adverse events such as loosening of internal fixation, rupture, nerve injury, and infection. However, despite these advantages, PEEK is not a perfect material for internal fixation. First, its radiolucency, while reducing artefacts in CT scans and making radiological follow-up easier, may fail to detect damage in the event of a breakage. Another disadvantage is cost, PEEK material is more expensive than titanium. Therefore, use without indications may result in a substantial increase in the cost of surgery [21, 34]. It has also been suggested [36] that although PEEK rods can promote bone graft fusion, there is a risk of cage subsidence and injury. In addition, PEEK rods have no spinal correction effect [21].
Limitation
Our meta-analysis has the following limitations. First, the number of studies that met the criteria was small and they were all limited to one country, and their quality was not high enough. Secondly, there is a lack of indicators to evaluate subjective feelings such as patient comfort and satisfaction. Moreover, the included studies were heterogeneous, which may be related to the large differences in surgical operation habits, surgical segments, and follow-up time of different investigators. Finally, the follow-up time of the included studies was not long enough, the long-term efficacy, incidence of adverse events, and degeneration of adjacent segments between the two groups remain to be tested and compared.
Conclusion
In conclusion, both PEEK rods and titanium rods can provide reliable fixation in lumbar fusion surgery. PEEK rods may be better than titanium rods in improving postoperative dysfunction, reducing lower limb pain, and improving bone graft fusion rate. However, given the limitations of this study, the applicability of these conclusions remains to be further investigated. Our work contributes to a more rational view of PEEK materials and the semi-rigid fixation represented by PEEK rods in lumbar fusion surgery.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information file.
Abbreviations
- PEEK:
-
Polyetheretherketone
- MD:
-
Mean differences
- OR:
-
Odds ratios
- CI:
-
Confidence intervals
- JOA:
-
Japanese Orthopaedic Association
- VAS:
-
Visual Analog Scale
- LBP:
-
Low back pain
- ODI:
-
Oswestry Disability Index
- ASD:
-
Adjacent segment degeneration
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- CNKI:
-
China National Knowledge Infrastructure
- ROM:
-
Range of motion
- DH:
-
Disc space height
References
De Iure F, Bosco G, Cappuccio M, Paderni S, Amendola L. Posterior lumbar fusion by peek rods in degenerative spine: preliminary report on 30 cases. Eur Spine J. 2012;21(Suppl 1):S50–4. https://doi.org/10.1007/s00586-012-2219-x.
Turner JL, Paller DJ, Murrell CB. The mechanical effect of commercially pure titanium and polyetheretherketone rods on spinal implants at the operative and adjacent levels. Spine (Phila Pa 1976). 2010;35(21):E1076–82. https://doi.org/10.1097/BRS.0b013e3181df1b85.
Ogrenci A, Koban O, Yaman O, Yilmaz M, Dalbayrak S. Polyetheretherketone rods in lumbar spine degenerative disease: mid-term results in a patient series involving radiological and clinical assessment. Turk Neurosurg. 2019;29(3):392–9. https://doi.org/10.5137/1019-5149.JTN.24320-18.2.
Toth JM, Wang M, Estes BT, Scifert JL, Seim HB 3rd, Turner AS. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials. 2006;27(3):324–34. https://doi.org/10.1016/j.biomaterials.2005.07.011.
Kurtz SM, Devine JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials. 2007;28(32):4845–69. https://doi.org/10.1016/j.biomaterials.2007.07.013.
Vadapalli S, Sairyo K, Goel VK, Robon M, Biyani A, Khandha A, Ebraheim NA. Biomechanical rationale for using polyetheretherketone (PEEK) spacers for lumbar interbody fusion-a finite element study. Spine (Phila Pa 1976). 2006;31(26):E992–8. https://doi.org/10.1097/01.brs.0000250177.84168.ba.
Rivard CH, Rhalmi S, Coillard C. In vivo biocompatibility testing of peek polymer for a spinal implant system: a study in rabbits. J Biomed Mater Res. 2002;62(4):488–98. https://doi.org/10.1002/jbm.10159.
Boriani S, Biagini R, Bandiera S, Gasbarrini A, De Iure F. Reconstruction of the anterior column of the thoracic and lumbar spine with a carbon fiber stackable cage system. Orthopedics. 2002;25(1):37–42.
Brantigan JW, McAfee PC, Cunningham BW, Wang H, Orbegoso CM. Interbody lumbar fusion using a carbon fiber cage implant versus allograft bone. An investigational study in the Spanish goat. Spine (Phila Pa 1976). 1994;19(13):1436–44. https://doi.org/10.1097/00007632-199407000-00002.
Ormond DR, Albert L Jr, Das K. Polyetheretherketone (PEEK) rods in lumbar spine degenerative disease: a case series. Clin Spine Surg. 2016;29(7):E371–5. https://doi.org/10.1097/BSD.0b013e318277cb9b.
Selim A, Mercer S, Tang F. Polyetheretherketone (PEEK) rods for lumbar fusion: a systematic review and meta-analysis. Int J Spine Surg. 2018;12(2):190–200. https://doi.org/10.14444/5027.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10:ED000142. https://doi.org/10.1002/14651858.ED000142.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Zhang J, Chai MX, Lu T, Sun XH, Jia JL. Lumbar spinal stenosis treated with polyetheretherketone pedicle screw fixation combined with interbody fusion: a follow-up assessment focusing on bone fusion rate. Chin J Tissue Eng Res. 2016;20(12):1684.
Sun ZG, Lu LS, Wang H, Wu QK, Sun JG, Yuan H, Fu YW. Clinical application of polyetheretherketone rod semi rigid fixation system in multi segmental in degenerative lumbar disease. Chin J Clin (Electron Ed). 2016. https://doi.org/10.3877/cma.j.issn.1674-0785.2016.19.008.
Wang HZ, Liu Y, Tan JF. Clincal application of polyetheretherketone rod semi-rigid fixation system in lumbar fusion. Chin J Trad Med Traum Orthop. 2020;28(4).
Li MH, Liu Y, Wang CM, Zhang M, Xu F. Therapeutic effects of polyetheretherketone rod-based dynamic spine internal fixation system versus traditional rigid internal fixation on lumbar degenerative diseases. Chin J Clin (Electron Ed). 2019. https://doi.org/10.3877/cma.j.issn.1674-0785.2019.11.011.
Tang B, Zhang Q, Xiong M. Clinical comparison of non-fusion of polyetheretherketone rod pedicle screw and transforaminal lumbar interbody fusion in the treatment of lumbar degenerative diseases. Chin J Clin. 2020;48(07):846–9. https://doi.org/10.3969/j.issn.2095-8552.2020.07.029.
Ding L, Li J, Zhang J, Sha YS. Clinical study of pedicle screw implantation with polyether ether copper biomaterial combined with intervertebral fusion in elderly patients with lumbar stenosis. J Pract Med. 2020. https://doi.org/10.3969/j.issn.1006-5725.2020.01.017.
Qi L, Li M, Zhang S, Xue J, Si H. Comparative effectiveness of PEEK rods versus titanium alloy rods in lumbar fusion: a preliminary report. Acta Neurochir (Wien). 2013;155(7):1187–93. https://doi.org/10.1007/s00701-013-1772-3.
Huang WM, Yu XC, Liang J, Song RX, Zhou K, Han ZW. Clinical outcome of PEEK rod pedicle screw system for senile lumbar degenerative disease. Chin J Geriatr Orthop Rehabil (Electron Ed). 2016;2(04):211–6.
Li FX, Cui GH, Li JH, Shen XK, Li XL, Li G, Wang WS, Shi CH. Efficacy of PEEK rod and titanium rod in the treatment of lumbar degenerative diseases with pedicle screw internal fixation. Reg Anat Oper Surg. 2015;24(05):513–6.
Han Y, Abdulwali AK. Clinical observation of elastic fixation rod in lumbar spine surgery. Med Inf. 2016;29(35):103–5. https://doi.org/10.3969/j.issn.1006-1959.2016.35.073.
Lu BT, Liu YJ, Xia N. The clinical application of polyether ether ketone semi-rigid fixation system in multi-segment degeneration lumbar spine disease. Health Wellness Guide. 2017;39:19. https://doi.org/10.3969/j.issn.1006-6845.2017.39.015.
Pang WF, Zhang SJ, Li K, Li HJ. Application of polyetheretherketone resin rod internal fixation system in lumbar degeneration. Shanxi Med J. 2020;49(14):1833–5.
Yang HJ, Fan Y, Wu ZX, Yang C, Zeng YP, Lei W, Sang HX. The clinical outcomes of a novel PEEK rod semi-rigid fixation system in the treatment of lumbar degenerative disease. Chin J Spine Spinal Cord. 2015;25(09):826–31.
Yu XC, Huang WM, Zhou Y, Liang J, Wang B, Zhang JT. Pedical dynamic internal fixation using polyetheretherketone rods for the treatment of degenerative Iumbar diseases. Chin J Biomed Eng. 2012;05:395–8.
Xu HG, Song JX, Wang H, Liu P, Wang LT, Chen XW, Yang XM, Zhang Y, Li YF, Yu HX. Clinical observation of pedicle screw-based PEEK dynamic stabilization system in lumbar degenerative diseases. Chin J Anat Clin. 2012;17(03):181–5.
Biswas JK, Rana M, Majumder S, Karmakar SK, Roychowdhury A. Effect of two-level pedicle-screw fixation with different rod materials on lumbar spine: a finite element study. J Orthop Sci. 2018;23(2):258–65. https://doi.org/10.1016/j.jos.2017.10.009.
Ahn YH, Chen WM, Lee KY, Park KW, Lee SJ. Comparison of the load-sharing characteristics between pedicle-based dynamic and rigid rod devices. Biomed Mater. 2008;3(4):044101. https://doi.org/10.1088/1748-6041/3/4/044101.
Gornet MF, Chan FW, Coleman JC, Murrell B, Nockels RP, Taylor BA, Lanman TH, Ochoa JA. Biomechanical assessment of a PEEK rod system for semi-rigid fixation of lumbar fusion constructs. J Biomech Eng. 2011;133(8):081009. https://doi.org/10.1115/1.4004862.
Kotani Y, Cunningham BW, Cappuccino A, Kaneda K, McAfee PC. The role of spinal instrumentation in augmenting lumbar posterolateral fusion. Spine Phila Pa (1976). 1996;21(3):278–87. https://doi.org/10.1097/00007632-199602010-00005.
Chou D, Lau D, Skelly A, Ecker E. Dynamic stabilization versus fusion for treatment of degenerative spine conditions. Evid Based Spine Care J. 2011;2(3):33–42. https://doi.org/10.1055/s-0030-1267111.
Wang N, Xie H, Xi C, Zhang H, Yan J. A study to compare the efficacy of polyether ether ketone rod device with titanium devices in posterior spinal fusion in a canine model. J Orthop Surg Res. 2017;12(1):40. https://doi.org/10.1186/s13018-017-0543-x.
Mavrogenis AF, Vottis C, Triantafyllopoulos G, Papagelopoulos PJ, Pneumaticos SG. PEEK rod systems for the spine. Eur J Orthop Surg Traumatol. 2014;24(Suppl 1):S111–6. https://doi.org/10.1007/s00590-014-1421-4.
Wu J, Shi L, Liu D, Wu Z, Gao P, Liu W, Li X, Guo Z. Evaluating screw stability after pedicle screw fixation with PEEK rods. Glob Spine J. 2021;4:2192568221996692. https://doi.org/10.1177/2192568221996692.
Fan W, Guo LX, Zhang M. Biomechanical analysis of lumbar interbody fusion supplemented with various posterior stabilization systems. Eur Spine J. 2021;30(8):2342–50. https://doi.org/10.1007/s00586-021-06856-7.
Agarwal A, Ingels M, Kodigudla M, Momeni N, Goel V, Agarwal AK. Adjacent-level hypermobility and instrumented-level fatigue loosening with titanium and PEEK rods for a pedicle screw system: an in vitro study. J Biomech Eng. 2016;138(5):051004. https://doi.org/10.1115/1.4032965.
Ponnappan RK, Serhan H, Zarda B, Patel R, Albert T, Vaccaro AR. Biomechanical evaluation and comparison of polyetheretherketone rod system to traditional titanium rod fixation. Spine J. 2009;9(3):263–7. https://doi.org/10.1016/j.spinee.2008.08.002.
Yeager MS, Cook DJ, Cheng BC. In vitro comparison of dynesys, PEEK, and titanium constructs in the lumbar spine. Adv Orthop. 2015;2015:895931. https://doi.org/10.1155/2015/895931.
Bruner HJ, Guan Y, Yoganandan N, Pintar FA, Maiman DJ, Slivka MA. Biomechanics of polyaryletherketone rod composites and titanium rods for posterior lumbosacral instrumentation. Presented at the 2010 joint spine section meeting. laboratory investigation. J Neurosurg Spine. 2010;13(6):766–72. https://doi.org/10.3171/2010.5.SPINE09948.
Hirt D, Prentice HA, Harris JE, Paxton EW, Alexander J, Nagasawa DT, Khosla D, Kurtz SM. Do PEEK rods for posterior instrumented fusion in the lumbar spine reduce the risk of adjacent segment disease? Int J Spine Surg. 2021;15(2):251–8. https://doi.org/10.14444/8034.
Ross DA, Ross MN. Lumbar fusion with polyetheretherketone rods use for patients with degenerative disease. Fed Pract. 2021;38(Suppl 1):S9–16. https://doi.org/10.12788/fp.0119.
Acknowledgements
Not applicable.
Funding
No funds were received in support of this research.
Author information
Authors and Affiliations
Contributions
LWH designed the study and contributed to the draft writing. ZH contributed to the data analysis and solved technical problems in software. LCH, GJB, LT participated in literature screening and data extraction. YX and YYD participated in the design of this research and provided guidance and troubleshooting. All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is a meta-analysis and does not require ethical approval and consent to participate.
Consent for publication
This research is a meta-analysis of other studies and does not contain any personal information and data, such as name, gender, age, images or video, etc., so no individual consent is required.
Competing interests
The authors declare that they have no competing interests in this section.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, W., Zhao, H., Li, C. et al. Polyetheretherketone (PEEK) rods versus titanium rods for posterior lumbar fusion surgery: a systematic review and meta-analysis. J Orthop Surg Res 18, 348 (2023). https://doi.org/10.1186/s13018-023-03817-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03817-2