Abstract
Introduction
The weight-adjusted waist circumference index (WWI) is a novel obesity evaluation indicator that appears to be superior to body mass index (BMI) and waist circumference (WC) in evaluating muscle and fat mass. The purpose of this study was to investigate the association between WWI and fractures among adults.
Methods
In this cross-sectional study, multivariate logistic regression and smoothed curve fitting were used to investigate linear and nonlinear associations between WWI and fractures, based on data from 28,679 adult participants in the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018.
Results
After adjusting for all covariates, the prevalence of hip/wrist/spine fractures among all participants was 1.09%, 8.87%, and 1.97%, respectively. A 1-unit increase in WWI was associated with a 5% increase in the odds of hip fractures [1.05 (1.01, 1.10)], and a 9% increase in the odds of spine fractures [1.09 (1.06, 1.13)], but not with the prevalence of wrist fractures [0.97 (0.94, 1.06)].
Conclusions
Higher WWI was associated with an increased prevalence of hip fracture and spine fracture, but not wrist fracture.
Similar content being viewed by others
Introduction
Osteoporosis is a systemic skeletal disease marked by low bone mass and architectural degeneration, accompanied by increased bone fragility and fracture risk [1, 2]. In the United States alone, osteoporotic fractures currently account for more than 500,000 hospitalizations [3], and this number is increasing as the population ages [4, 5]. Therefore, early prevention of fractures and exploration of risk factors is critical [6], and advances in population-based studies have led to more accurate assessments of fracture risk and expanded the range of options available for fracture prevention [7, 8].
Obesity is a complex metabolic disease [9]. The prevalence of obesity has increased dramatically over the past few decades and is now at an unprecedented level: nearly one-third of the global population is obese [10, 11]. Although it has long been known that obesity may protect against osteoporosis and fractures [12,13,14], a significant amount of research has emerged in recent years that refutes this theory [15,16,17,18,19]. Body mass index (BMI) and waist circumference (WC), two commonly used obesity markers, fail to differentiate between muscle mass and fat mass [20], while body composition and body fat distribution have been proposed to more accurately reflect adverse metabolic characteristics [21, 22].
The weight-adjusted waist circumference index (WWI), originally proposed by Park et al. [23], was shown to be associated with age-related changes in body composition, such as loss of muscle mass and retention or gain of fat mass [24]. In addition, several studies have shown a significant positive association between WWI and cardiovascular disease [25,26,27], chronic kidney disease [28], and all-cause mortality [29].
However, no studies have assessed the association between WWI and fractures. As a result, we performed a cross-sectional study to investigate the relationship between WWI and fractures using data from the National Health and Nutrition Examination Survey (NHANES) 1999–2018.
Methods
Study population
The NHANES, a program of the National Center for Health Statistics, is a well-known, nationally representative, cross-sectional survey that is performed across the United States [30, 31]. The National Center for Health Statistics (NCHS) Research Ethics Review Board approved the study procedure. At the time of recruitment, all participants provided written consent. The survey was conducted during 10 survey cycles over two decades (1999–2018). We excluded 32,949 participants without fractures questionnaire data, 23,796 participants with missing BMI or WC data, and 31,452 participants younger than 20 years old. The study eventually included 28,679 participants (Fig. 1).
Study variables
WWI is an index to evaluate body fat mass and muscle mass, calculated by dividing WC (cm) by the square root of body weight (kg) [32]. At the mobile examination center, certified health technicians measured participants' weight and waist circumference. Participants' weights were determined by removing shoes and heavy clothing, and waist circumference was determined by drawing a horizontal line above the highest lateral border of the right iliac bone to plot the right mid-axillary line and placing a tape measure at the intersection of the two lines [33]. For the purpose of the participant's current fracture or fracture history diagnosis, participants were asked to recall whether they had previously been diagnosed with a hip/wrist/spine fracture by a professional orthopedic surgeon. An affirmative answer was identified as a current fracture or fracture history at the specific site [34, 35]. Covariates included demographic variables [age, sex, education levels, income-to-poverty ratio (PIR), and race]; examination variables [bone mineral density (BMD), waist circumference, and BMI]; laboratory variables [LDL-C (low-density lipoprotein cholesterol), total 25 (OH) D (25-hydroxy vitamin D), total calcium, and triglycerides]; dietary variables [dietary inflammatory index (calculated from 45 nutrient intakes)]; questionnaire variables [smoking status (Never/Ever/Current) [36], diabetes (Yes/No), use of hormone therapy (Yes/No)]. Comprehensive guidance regarding the collection methods of variables can be accessed from the NHANES Survey Methods (https://wwwn.cdc.gov/nchs/nhanes).
Statistical analysis
As NHANES uses complex multi-stage sampling, we included appropriate weights in all statistical analyses in accordance with official guidelines [37, 38]. The study evaluated the characteristics of participants by dividing them into quartiles based on the WWI and employing chi-square and t-tests for analysis. Weighted multivariate logistic regression analysis was utilized to explore the linear relationship between WWI and fracture, and three models were developed to examine the association. Model 1 had no adjusted variables, Model 2 adjusted for age, gender, and race, and Model 3 adjusted for age, gender, race, smoking, dietary inflammatory index, diabetes, PIR, total 25 (OH) D, total calcium, use of hormone therapy, triglycerides, BMD, and LDL-C [39]. The association's strength was estimated using the odds ratio (OR) and its associated 95% confidence interval (CI) for the multivariate model. To assess the linear relationship between WWI and fracture, the researchers transformed WWI from a continuous variable to a categorical variable (quartiles) and analyzed trends using trend tests. Subgroup analyses were carried out to examine the association between WWI and fracture in individuals of varying gender, race, education, and diabetes status. Interaction tests were conducted to determine if the association was consistent across subgroups. For all results from multiple logistic regression analyses and subgroup analyses, we used the estimates from the fully adjusted model (Model 3) for interpretation. The researchers utilized smoothing curve fitting to explore the nonlinear relationship between WWI and fracture [40,41,42,43]. All analyses were performed using R (version 4.2) or Empowerstats (version 5.0), and a p-value < 0.05 was deemed statistically significant.
Results
Baseline characteristics
The mean (SD) age and mean WWI (SD) of the 28,679 participants were 49.99 (18.02) years and 11.02 (0.84), respectively. Of these, 48.01% were male and 51.36% were non-Hispanic white. The prevalence of hip/wrist/spine fractures was 1.09%, 8.87%, and 1.97%, respectively. Compared with the bottom WWI quartile, participants in the top WWI quartile were more likely to be female, Mexican American, and elderly; in terms of socioeconomic status, participants with higher WWI were more likely to have lower education and income; in terms of lifestyle, participants with higher WWI had higher rates of smoking and higher dietary inflammatory potential; in addition, participants with higher WWI typically had a higher prevalence of diabetes and fractures; had higher BMI, waist circumference, and lipid levels, and lower BMD, total 25 (OH) D, and total calcium (Table 1).
Association between WWI and fractures
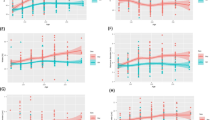
Table 2 shows the associations between WWI and fractures. The results showed a significant positive linear association between WWI with hip fracture and spine fracture, while a non-significant negative association existed between WWI and wrist fracture. After adjusting for all covariates, each unit increase in WWI was associated with a 5% increase in the odds of hip fracture [1.05 (1.01, 1.10)] and an 9% increase in the odds of spine fracture [1.09 (1.06, 1.13)]. This significant positive association was maintained even when WWI was transformed into a categorical variable, with participants in the highest quartile of WWI having a 68% and 32% increased odds of hip fracture [1.68 (1.11, 2.01)] and spine fracture [1.32 (1.05, 1.55)], respectively. In addition, the results of the smoothed curve fitting further validated the nonlinear positive associations between WWI with hip fracture and spine fracture (Fig. 2).
The nonlinear associations between weight-adjusted waist index and fractures. The solid red line represents the smooth curve fit between variables. Blue bands represent the 95% of confidence interval from the fit. A. WWI and hip fracture; B WWI and wrist fracture; C WWI and spine fracture. WWI, weight-adjusted waist index
Subgroup analyses
We conducted subgroup analysis and interaction tests stratified by age, gender, race, BMI, and diabetes to assess whether the relationship between WWI and fractures was consistent in the general population and identify any potential different population settings (Table 3). The results showed that the association between WWI and hip fracture was significantly different across the educational population, with participants below high school having a 39% and 65% higher prevalence of hip fracture than those in high school [0.60 (0.30, 1.02)] and above high school [0.36 (0.14, 1.02)], respectively. The association between WWI and fracture remained stable in the other subgroups (P for interaction > 0.05).
Discussion
In the cross-sectional study that enrolled 28,679 eligible participants, we investigated the association between a new indicator of obesity, the WWI, and fractures at different sites. Our results suggest that elevated WWI is significantly associated with higher prevalence of hip fracture and spine fracture, but not wrist fracture. These findings suggest that WWI may be a valid indicator for assessing the association between obesity and fracture prevalence. The current findings underscore the significance of WWI in preventing and managing patients who are at a higher risk of experiencing fractures. Additionally, the findings provide a foundation for future research into the causal relationship between WWI and the prevalence of fractures.
To our knowledge, this is the first study to assess the relationship between WWI and fractures. In the past, obesity and being overweight have been considered a protective factor of osteoporosis and fractures. Several epidemiological studies with menopausal women have investigated the association between BMI and fracture risk, and these results suggest that an increase in BMI is associated with a decreased risk of fracture, with the most pronounced protective effect especially for hip fractures [18, 44,45,46]. However, studies contradicting these results have gradually increased. In a study that included 799 menopausal women, Premaor et al. found a significantly lower risk of wrist fracture and a significantly higher risk of hip fracture compared with women who were not obese [47]. The results of our large sample size study also suggest an association between rising WWI and higher hip fractures and a non-significant negative association with wrist fractures. A UK cohort study that included participants of different genders also showed that obese participants had a higher risk of ankle and upper arm fractures, but a 35% lower risk of wrist fractures [48]. The findings of epidemiological studies that contradict this long-held belief have spurred renewed interest in the paradigm shift regarding obesity as a protective factor for osteoporotic fractures [49].
On the one hand, with advances in investigation methods, several studies have identified nonlinear associations and saturation effects between BMI and fractures in a different ages, sex, and ethnic groups, and these results suggest that the association between BMI and fracture cannot be described simply by a linear positive correlation [15, 50, 51]. In addition, studies from different countries and regions have shown significant differences between BMI and fracture risk at different sites [47, 52, 53].
On the other hand, most studies investigating the association between obesity and fractures use BMI and WC to measure obesity and cannot distinguish between muscle mass, fat mass, and fat distribution. Gnudi et al. proposed a link between BMD with fat mass and muscle mass in women with osteoporosis, suggesting body composition is an essential element in research exploring bone metabolism [54]. The WWI is a unique anthropometric index that is considered to be a marker that can assess both high-fat mass and low-muscle mass [55]. The "obesity paradox" observed in the relationship between BMI or WC and metabolic diseases were observed to be less pronounced in WWI [56]. The current findings suggest that the obesity paradox may not exist but is attributable to BMI's inability to distinguish between muscle mass and fat mass [57]. The results of several recent epidemiological studies suggest that WWI outperforms BMI, WC, and waist-height ratios in the assessment of obesity and cardiovascular disease [58], sarcopenia [57], cardiac mortality, and all-cause mortality [23, 59].
The results of the subgroup analyses showed that the correlations between WWI and hip fractures differed among the subgroups of education level. Results similar to this finding have been reported in previous studies [60]. Results from a cross-sectional study investigating American men aged 20 years and older suggest that higher education and income are significantly associated with high lumbar BMD and that the educational attainment of participants should be fully considered in the prevention and treatment of osteoporotic fractures [61]. The data suggest that the effects of education on bone health are broad and complex and may affect bone metabolism in a variety of ways, including through income, cognition, occupation, and physical activity patterns [62,63,64,65]. Despite the consistency of the findings concerning significant differences between subgroups of educational attainment with prior research, caution is warranted in interpreting the significant outcomes observed in the subgroup analysis. There is a potential risk of false positives due to the failure to account for multiplicity between subgroups, and this possibility should be considered when interpreting the results.
The underlying mechanisms of this negative correlation between WWI and fractures are not fully understood. The metabolic characteristics of subcutaneous and visceral fat differ, and pro-inflammatory cytokines and tumor necrosis factor-alpha from visceral fat can accelerate bone resorption and so have a negative impact on bone metabolism [66]. Furthermore, there is compelling evidence that mesenchymal stromal/stem cells (MSC) are negatively associated with adipocytic and osteoblast commitment. The same mechanisms that govern MSC formation locally within the marrow microenvironment may act systemically between peripheral adipose depots and trabecular and cortical bone in cases of subcutaneous or visceral obesity [67, 68].
The strengths of our study include the use of a complex multi-stage probability sampling design and a large sample size, which increase the reliability and representativeness of our study. Our research has several limitations. First, we were unable to determine a causal association between WWI and fractures because to the design of the cross-sectional analysis. In addition, due to database limitations, we were unable to include data on all covariates that have an impact on bone metabolism, such as menopause, in order to maintain a sufficiently large sample size. Nevertheless, the current correlation between WWI and fractures was stable enough to be less likely to be significantly influenced by unincluded factors.
Conclusion
Our results suggest that higher WWI is associated with an increased prevalence of hip fracture and spine fracture, but not wrist fracture. Further prospective studies and causal inference studies are needed to validate our findings.
Availability of data and materials
The survey data are publicly available on the internet for data users and researchers throughout the world ( www.cdc.gov/nchs/nhanes/).
Abbreviations
- WWI:
-
Weight-adjusted waist circumference index
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- LDL-C:
-
Low-density lipoprotein cholesterol
- Total 25 (OH):
-
D (25-hydroxy vitamin D
- PIR:
-
Income-to-Poverty Ratio
- MSC:
-
Mesenchymal stromal/Stem cells
References
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–9.
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–6.
Health UDo, Services H: Bone health and osteoporosis: a report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Office of the Surgeon General 2004, 87.
Ayers C, Kansagara D, Lazur B, Fu R, Kwon A, Harrod C. Effectiveness and safety of treatments to prevent fractures in people with low bone mass or primary osteoporosis: a living systematic review and network meta-analysis for the american college of physicians. Ann Intern Med. 2023;5:49.
Si L, Winzenberg TM, de Graaff B, Palmer AJ. A systematic review and meta-analysis of utility-based quality of life for osteoporosis-related conditions. Osteoporos Int. 2014;25(8):1987–97.
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364–76.
Xie R, Huang X, Zhang Y, Liu Q, Liu M. High low-density lipoprotein cholesterol levels are associated with osteoporosis among adults 20–59 years of age. Int J Gen Med. 2022;15:2261–70.
Xie R, Huang X, Liu Q, Liu M. Positive association between high-density lipoprotein cholesterol and bone mineral density in U.S. adults: the NHANES 2011–2018. J Orthop Surg Res. 2022;17(1):92.
Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022;399(10322):394–405.
Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, Mozaffarian D, Swinburn B, Ezzati M. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7(3):231–40.
Network GBoDC: Global Burden of Disease Study 2015 (GBD 2015) Obesity and Overweight Prevalence 1980–2015. In: IHME Seattle; 2017.
Wang J, Yan D, Hou X, Chen P, Sun Q, Bao Y, Hu C, Zhang Z, Jia W. Association of adiposity indices with bone density and bone turnover in the Chinese population. Osteoporos Int. 2017;28(9):2645–52.
Ma M, Feng Z, Liu X, Jia G, Geng B, Xia Y. The saturation effect of body mass index on bone mineral density for people over 50 years old: a cross-sectional study of the US population. Front Nutr. 2021;8:763677.
Tang Y, Liu Z, Wang S, Yi Q, Xia Y, Geng B. Development and validation of a novel screening tool for osteoporosis in older US adults: the NHANES cross-sectional study. Endocrine. 2022;76(2):446–56.
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16(11):1330–8.
Compston JE, Flahive J, Hosmer DW, Watts NB, Siris ES, Silverman S, Saag KG, Roux C, Rossini M, Pfeilschifter J, et al. Relationship of weight, height, and body mass index with fracture risk at different sites in postmenopausal women: the Global Longitudinal study of Osteoporosis in Women (GLOW). J Bone Miner Res. 2014;29(2):487–93.
Willig R, Luukinen H, Jalovaara P. Factors related to occurrence of hip fracture during a fall on the hip. Public Health. 2003;117(1):25–30.
Joakimsen RM, Fønnebø V, Magnus JH, Tollan A, Søgaard AJ. The Tromsø Study: body height, body mass index and fractures. Osteoporos Int. 1998;8(5):436–42.
van der Voort DJ, Geusens PP, Dinant GJ. Risk factors for osteoporosis related to their outcome: fractures. Osteoporos Int. 2001;12(8):630–8.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32(6):959–66.
Shieh A, Karlamangla AS, Karvonen-Guttierez C, Greendale GA. Menopause-related changes in body composition are associated with subsequent bone mineral density and fractures: study of Women’s Health Across the Nation. J Bone Miner Res. 2022;2:796.
Ma M, Liu X, Jia G, Geng B, Xia Y. The association between body fat distribution and bone mineral density: evidence from the US population. BMC Endocr Disord. 2022;22(1):170.
Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8(1):16753.
Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. 2021;50(3):780–6.
Zhang D, Shi W, Ding Z, Park J, Wu S, Zhang J. Association between weight-adjusted-waist index and heart failure: results from National Health and Nutrition Examination Survey 1999–2018. Front Cardiovasc Med. 2022;9:1069146.
Qin Z, Du D, Li Y, Chang K, Yang Q, Zhang Z, Liao R, Su B. The association between weight-adjusted-waist index and abdominal aortic calcification in adults aged ≥ 40 years: results from NHANES 2013–2014. Sci Rep. 2022;12(1):20354.
Cai S, Zhu T, Ding Y, Cheng B, Zhang A, Bao Q, Sun J, Li M, Liu X, Wang S. The relationship between the weight-adjusted-waist index and left ventricular hypertrophy in Chinese hypertension adults. Hypertens Res. 2023;46(1):253–60.
Qin Z, Chang K, Yang Q, Yu Q, Liao R, Su B. The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: A population-based study. Front Nutr. 2022;9:941926.
Cai S, Zhou L, Zhang Y, Cheng B, Zhang A, Sun J, Li M, Su Y, Bao Q, Zhang Y, et al. Association of the weight-adjusted-waist index with risk of all-cause mortality: a 10-year follow-up study. Front Nutr. 2022;9:894686.
Zhang Y, Xie R, Ou J. A U-shaped association between serum albumin with total triiodothyronine in adults. J Clin Lab Anal. 2022;36(6):e24473.
Xie R, Zhang Y. Index-based calculation or Transient Elastography to assess the degree of hepatic steatosis and fibrosis. J Nutr. 2022;2:71.
Zierfuss B, Höbaus C, Herz CT, Pesau G, Koppensteiner R, Schernthaner GH. Predictive power of novel and established obesity indices for outcome in PAD during a five-year follow-up. Nutr Metab Cardiovasc Dis. 2020;30(7):1179–87.
Ouyang Y, Quan Y, Guo C, Xie S, Liu C, Huang X, Huang X, Chen Y, Xiao X, Ma N, et al. Saturation effect of body mass index on bone mineral density in adolescents of different ages: a population-based study. Front Endocrinol (Lausanne). 2022;13:922903.
Ye J, Li Q, Nie J. Prevalence, characteristics, and associated risk factors of wrist fractures in americans above 50: the cross-sectional NHANES study. Front Endocrinol (Lausanne). 2022;13:800129.
Ma M, Liu X, Jia G, Liu Z, Zhang K, He L, Geng B, Xia Y. The association between depression and bone metabolism: a US nationally representative cross-sectional study. Arch Osteoporos. 2022;17(1):113.
Qin Z, Jiang L, Sun J, Geng J, Chen S, Yang Q, Su B, Liao R. Higher visceral adiposity index is associated with increased likelihood of abdominal aortic calcification. Clinics (Sao Paulo). 2022;77:100114.
Xie R, Zhang Y. Associations between dietary flavonoid intake with hepatic steatosis and fibrosis quantified by VCTE: evidence from NHANES and FNDDS. Nutr Metabol Cardiovasc Dis. 2023;2:51.
Xie R, Xiao M, Li L, Ma N, Liu M, Huang X, Liu Q, Zhang Y. Association between SII and hepatic steatosis and liver fibrosis: a population-based study. Front Immunol. 2022;13:925690.
Xie R, Zhang Y. Is assessing the degree of hepatic steatosis and fibrosis based on index calculations the best choice for epidemiological studies? Environ Pollut. 2022;317:120783.
Perperoglou A, Sauerbrei W, Abrahamowicz M, Schmid M. A review of spline function procedures in R. BMC Med Res Methodol. 2019;19(1):46.
Xie R, Zhang Y. Association between 19 dietary fatty acids intake and rheumatoid arthritis: results of a nationwide survey. Prost Leukotrienes Essential Fatty Acids. 2022;6:102530.
Luo J, Liu M, Zheng Z, Zhang Y, Xie R. Association of urinary caffeine and caffeine metabolites with bone mineral density in children and adolescents. Medicine. 2022;101(49):e31984.
Xie R, Liu Y, Wang J, Zhang C, Xiao M, Liu M, Zhang Y. Race and gender differences in the associations between cadmium exposure and bone mineral density in US adults. Biol Trace Elem Res. 2022;5:149.
Paganini-Hill A, Chao A, Ross RK, Henderson BE. Exercise and other factors in the prevention of hip fracture: the Leisure World study. Epidemiology. 1991;2(1):16–25.
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–73.
Honkanen RJ, Honkanen K, Kröger H, Alhava E, Tuppurainen M, Saarikoski S. Risk factors for perimenopausal distal forearm fracture. Osteoporos Int. 2000;11(3):265–70.
Premaor MO, Pilbrow L, Tonkin C, Parker RA, Compston J. Obesity and fractures in postmenopausal women. J Bone Miner Res. 2010;25(2):292–7.
Ong T, Sahota O, Tan W, Marshall L. A United Kingdom perspective on the relationship between body mass index (BMI) and bone health: a cross sectional analysis of data from the Nottingham Fracture Liaison Service. Bone. 2014;59:207–10.
Piñar-Gutierrez A, García-Fontana C, García-Fontana B, Muñoz-Torres M. Obesity and bone health: a complex relationship. Int J Mol Sci. 2022;23(15):4965.
Xie R, Liu M. Relationship between non-alcoholic fatty liver disease and degree of hepatic steatosis and bone mineral density. Front Endocrinol (Lausanne). 2022;13:857110.
Xie R, Zhang Y, Yan T, Huang X, Xie S, Liu C, Liu M. Relationship between nonalcoholic fatty liver disease and bone mineral density in adolescents. Medicine (Baltimore). 2022;101(41):e31164.
Beck TJ, Petit MA, Wu G, LeBoff MS, Cauley JA, Chen Z. Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women’s health initiative-observational study. J Bone Miner Res. 2009;24(8):1369–79.
Compston JE, Watts NB, Chapurlat R, Cooper C, Boonen S, Greenspan S, Pfeilschifter J, Silverman S, Díez-Pérez A, Lindsay R, et al. Obesity is not protective against fracture in postmenopausal women: GLOW. Am J Med. 2011;124(11):1043–50.
Gnudi S, Sitta E, Lisi L. Relationship of body mass index with main limb fragility fractures in postmenopausal women. J Bone Miner Metab. 2009;27(4):479–84.
Zhao P, Shi W, Shi Y, Xiong Y, Ding C, Song X, Qiu G, Li J, Zhou W, Yu C, et al. Positive association between weight-adjusted-waist index and hyperuricemia in patients with hypertension: the China H-type hypertension registry study. Front Endocrinol (Lausanne). 2022;13:1007557.
Fassio A, Idolazzi L, Rossini M, Gatti D, Adami G, Giollo A, Viapiana O. The obesity paradox and osteoporosis. Eat Weight Disord. 2018;23(3):293–302.
Kim JE, Choi J, Kim M, Won CW. Assessment of existing anthropometric indices for screening sarcopenic obesity in older adults. Br J Nutr. 2022;5:1–13.
Li Q, Qie R, Qin P, Zhang D, Guo C, Zhou Q, Tian G, Liu D, Chen X, Liu L, et al. Association of weight-adjusted-waist index with incident hypertension: The Rural Chinese Cohort Study. Nutr Metab Cardiovasc Dis. 2020;30(10):1732–41.
Ding C, Shi Y, Li J, Li M, Hu L, Rao J, Liu L, Zhao P, Xie C, Zhan B, et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: a prospective cohort study. Nutr Metab Cardiovasc Dis. 2022;32(5):1210–7.
Valentin G, Ravn MB, Jensen EK, Friis K, Bhimjiyani A, Ben-Shlomo Y, Hartley A, Nielsen CP, Langdahl B, Gregson CL. Socio-economic inequalities in fragility fracture incidence: a systematic review and meta-analysis of 61 observational studies. Osteoporos Int. 2021;32(12):2433–48.
Xiao PL, Fuerwa C, Hsu CJ, Peng R, Cui AY, Jiang N, Ma YG, Xu XH, Lu HD. Socioeconomic status influences on bone mineral density in American men: findings from NHANES 2011–2020. Osteoporos Int. 2022;33(11):2347–55.
Bai WY, Xia JW, Rong XL, Cong PK, Khederzadeh S, Zheng HF. Integrative analysis of genomic and epigenomic data reveal underlying superenhancer-mediated microRNA regulatory network for human bone mineral density. Hum Mol Genet. 2021;30(22):2177–89.
Tseng OL, Dawes MG, Spinelli JJ, Gotay CC, McBride ML. Utilization of bone mineral density testing among breast cancer survivors in British Columbia, Canada. Osteoporos Int. 2017;28(12):3439–49.
Benedetti MG, Furlini G, Zati A, Letizia Mauro G. The effectiveness of physical exercise on bone density in osteoporotic patients. Biomed Res Int. 2018;2018:4840531.
Fabiani R, Naldini G, Chiavarini M. Dietary patterns in relation to low bone mineral density and fracture risk: a systematic review and meta-analysis. Adv Nutr. 2019;10(2):219–36.
Morley JE, Baumgartner RN. Cytokine-related aging process. J Gerontol A Biol Sci Med Sci. 2004;59(9):M924-929.
Gimble JM, Zvonic S, Floyd ZE, Kassem M, Nuttall ME. Playing with bone and fat. J Cell Biochem. 2006;98(2):251–66.
Katzmarzyk PT, Barreira TV, Harrington DM, Staiano AE, Heymsfield SB, Gimble JM. Relationship between abdominal fat and bone mineral density in white and African American adults. Bone. 2012;50(2):576–9.
Acknowledgements
We would like to thank all participants in this study.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
YZ, JT and WT designed the research. JT, YZ and CT collected, analyzed the data, and drafted the manuscript. JT revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethical Approval and consent to participate
The portions of this study involving human participants, human materials, or human data were conducted in accordance with the Declaration of Helsinki and were approved by the NCHS Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
Consent to Publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tao, J., Zhang, Y., Tan, C. et al. Associations between weight-adjusted waist index and fractures: a population-based study. J Orthop Surg Res 18, 290 (2023). https://doi.org/10.1186/s13018-023-03776-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03776-8