Abstract
Background
For ages, humankind and horses have been closely related to occupational and recreational activities. The dangers of engaging with horses have been previously reported. Among sporting activities, horse riding is well-known for its risks. Despite multiple recommendations to wear protective gear, horse-related activities still comprise the risk of severe injuries. This study aimed to examine: (1) if specific mechanisms are correlated to particular injury patterns and (2) if injury types are related to patient demographics.
Methods
From one level I trauma center, between July 2019 and July 2022 (3 years) all emergency reports and discharge letters were retrospectively reviewed by full-text search regarding horse-related injuries. Patient demographics, body mass index, trauma mechanism, injury types, and initiated treatment were extracted from medical records and analyzed.
Results
During the study period, 95 patients with 99 horse-related injuries were included. The overwhelming majority of the patients was female (93.7%). Age averaged 35.3 years (range 6 to 71). BMI was 23.6 kg/m2. Inpatient treatment was required in 60.6%. Length of hospital stay averaged 10 days. Surgical treatment was performed in 55 patients (55.6%). Open reduction and internal fixation was the most common procedure (74.5%). Trauma mechanism was fall from a horse followed by being hit by a horse (60.6% and 23.2%, respectively). Injured upper extremities counted up for 52.5% followed by spinal and pelvic injuries (23.2%). Spinal and pelvic injuries were related to fall from a horse (p < 0.001). Injuries to the lower extremities were predominantly caused by a kick of the horse when the rider was unmounted (p = 0.001) and negatively related to a fall from a horse (p = 0.002). Ten patients got their fingers tangled while holding the reins and suffered from injuries to the upper extremity (p < 0.001). Three of them required an amputation (30%).
Conclusion
Despite the fact that patients are young and healthy, horse related injuries must not be underestimated. In our study, almost two-thirds of the patients required inpatient treatment and 50% underwent surgery. We could show that patient age was related to injury severity according to the Abbreviated Injury Scale (AIS). Spinal and pelvic injuries were significantly related to a fall from a horse with a significantly greater trauma impact according to the AIS. Therefore, these severe entities need to be ruled out in such events. Accidents caused by holding the reins, may result in serious injuries to the hand with 30% requiring an amputation. Doctors need to be aware of possible horse-related injury patterns to reduce morbidity.
Similar content being viewed by others
Background
For ages, mankind has been domesticating horses for occupational and recreational activities. During the recent decades, in industrial countries the relationship with horses has focused on sports and leisure. The dangers of engaging with horses and their unpredictable behavior when it comes to unforeseen circumstances have been previously reported [1, 2]. Among sporting activities, horse riding is well known for its risks in regards to their height, velocity, kicking force, and weight [2, 3]. Despite multiple recommendations to wear personal protective equipment, horse-related activities still comprise the risk of severe injuries comparable to motorized sports [4,5,6].
While the awareness of risk factors associated with horse-related injuries may be useful for prevention among horseback riders [7], the knowledge of risk factors among medical staff may help with diagnostics and may reduce morbidity. This study aimed to examine: (1) if specific mechanisms are correlated to particular injury patterns and (2) if injury types are related to different patient demographics.
Methods
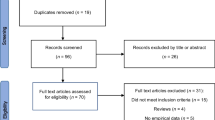
This study was an Institutional Review Board approved retrospective cohort study of consecutive patients undergoing treatment for horse-related injuries in one level I and referral trauma center in an urban area. During the study period, from the start of July 2019 through to the end of June 2022 (3 years) a total of 102 injuries were identified by full-text search of patient medical records (MEDICO, CGM Europe) that had treatment for horse-related injuries. Inclusion criteria were outpatient or inpatient treatment for injuries caused by horse-riding or during associated nonriding activities (e.g. feeding, grooming, shoeing, etc.). Exclusion criteria were injuries to persons not involved with the normal handling of the animals or injuries that occurred fatefully. No patients were phoned in specifically for this study; all data were obtained from preexisting medical records and radiographs.
Clinical data assessment
Patient demographics, injury mechanism and pattern, and medical treatment were extracted from the hospital documentation program (MEDICO, CGM Europe). Gender, age, Body-Mass-Index (BMI), insurance status, and injury mechanism were collected as descriptive data. Injury pattern, inpatient treatment, length of hospital stay, and surgeries performed were utilized as outcomes data. Radiographs were reviewed utilizing the picture archiving and communication system (PACS) (IMPAX 6.6.1, AGFA HealthCare N.V., Belgium).
Statistical analysis
For statistical analysis, Excel (Microsoft® Office Excel©, Version 16.44) and SPSS version 27.0 (IBM, Chicago, IL) were utilized. To compare continuous variables (age, BMI, inpatient stay) T-test was performed. For nominally and ordinally scaled data, the Cℎi2 test or Fischer's exact test was applied. A significance threshold of p < 0.05 was selected for all statistical tests and the p values determined were rounded to three decimal places.
Results
During the study period, full-text search revealed 102 presentations for horse-related injuries. Three patients were excluded. One patient suffered from a horse-bite while feeding and caressing an unknown horse on a meadow. Two patients twisted their ankles while walking next to their horse or longeing a horse. The latter injuries occurred fatefully without being caused by the horse. (Fig. 1). Four patients presented twice during the study period for different accidents, which left us with 99 horse-related injuries in 95 patients. The overwhelming majority of the patients was female (93.7%). Age averaged 35.5 years (range 6–71) with 20 patients younger than 18 years (21.1%). BMI was 23.6 kg/m2 (SD ± 4.03). One third of the patients (32/95) had a private health insurance, which is three times as much as in the normal population (10.5%) [8].
Trauma mechanism
Trauma mechanism was falling from a horse followed by being kicked or trampled by a horse (60.6% and 23.2%, respectively). Ten patients got their fingers tangled while holding the reins. Other trauma mechanisms were observed in 6 patients including getting a foot trapped in a stirrup, being hit by the head of the horse, and being squashed while being in a horse stall. Injured upper extremities counted up for 52.5% followed by spinal and pelvic injuries (23.2%). Spinal and pelvic injuries were related to fall from a horse (p < 0.001) and negatively related to injuries of the lower extremities (p = 0.002). Injuries to the lower extremities were predominantly caused by a kick from the horse when the rider was unmounted (p = 0.001) (Table 1).
Injury severity varied from 1 to 5 according to the Abbreviated Injury Scale (AIS) with an average of 2.13 (SD ± 0.95) and was related to the age of the patients (p = 0.015). AIS was not related to BMI (p = 0.595). Sixty patients were admitted for inpatient treatment (60.6%). Patients treated in the hospital had a higher AIS compared to those treated as outpatients (AIS 2.45 vs. 1.64, respectively; p < 0.001). Surgical treatment was performed in 55 patients (55.6%). Open reduction and internal fixation (ORIF) was the most common procedure (74.5%) (Table 2). Length of hospital stay averaged 9.9 days (SD ± 26.7).
Injury types
Patients with spinal or pelvic injuries had a higher AIS (2.48 vs. 2.03, respectively; p = 0.046) and were treated for significantly longer in hospital (25 days) compared to other injuries (p = 0.019). This was caused by two patients with complete and incomplete tetraplegia after trauma to the cervical spine. Patients with spinal or pelvic injuries tended to be older (38.5 vs 34.4 years) but that was not significant (p = 0.280). Eleven patients with injuries of the spine and pelvis underwent surgery (47.8%) (Table 3).
The majority of patients (52, 52.5%; respectively) presented for injuries to the upper limb. Thereof, thirty-five patients were admitted for inpatient treatment (67.3%). Length of hospital stay was shortest for patients with upper extremity injuries and averaged 4.1 days (p = 0.041). Surgery was performed in 34 patients (65.4%) (Table 4). Injuries involving the hand required surgery most frequently (35.3%). This results also from rein injuries. Ten patients got their fingers tangled while holding the reins and therefore suffered from injuries to the upper extremity (p = 0.001). Three of them required an amputation (30%).
Lower extremity injuries were related to a kick from a horse or being trodden on a foot (p = 0.001) and occurred in 20 patients (20.2%). Nine patients (45%) were admitted to the hospital for subsequent surgery. Open reduction and internal fixation of the ankle joint was performed in two patients. Three patients underwent ORIF for tibial shaft and tibial plateau fractures. Additionally, one patient required an anterior cruciate ligament replacement after being knocked down while walking her horse. Two patients suffered from foot injuries and one patient underwent a hip arthroscopy for a flake fracture and microfracturing of the femoral head.
Because of head injuries, nine patients (9.1%) were presented in the emergency department. Mean age of patients with head trauma was 41.7 years compared to 34.7 years for the rest of the study population (p = 0.304). Head trauma had the lowest AIS (1.89) and varied from contusion (5 patients) and head wound with active bleeding (one patient) to severe traumatic brain injury with intracranial hemorrhage. One patient (1%) deceased due to traumatic brain injury with brainstem lesion. Therefore, the mortality rate of our study was 1.0%.
Discussion
Despite the fact that injuries related to equestrian accidents form only a small percentage of attendances to the emergency department especially in urban areas, injury patterns should not be underestimated and consequences of these injuries can be profound [6, 9]. Most of the horse-related injuries (60.6%) occurred while mounted on horseback, followed by being kicked by a horse. This is in concordance with a US National Electronic Injury Surveillance System (NEISS) data analysis and previous studies [4, 9]. This single center experience reveals that injury patterns vary between mounted and unmounted individuals. While falling from a horse leads to more severe spinal and pelvic injuries, tangling up in reins resulted in upper extremity injuries (1). No gender specific differences in injury types were observed, but injury severity was related to patient age according to the AIS (2).
Regarding the female majority in our study population, differences of horse-related activities exist between nations and countries. Horseback riding seems to be a male sport in Israel with 79% injured boys [10]. Whereas, a 10-year national trauma database analysis in the US showed a 50/50 distribution between males and females [1]. Studies from Australia found 54–59% females with horse-related injuries [7, 11]. In contrast hereto, there is a predominance of females in Europe. Two studies from The Netherlands and France found 81% females with equestrian-related injuries [2, 12]. Whereas, a Swedish study revealed up to 98% injured females [13]. In Germany, horseback riding is a popular sport especially for younger females (80%) [14]. Therefore, our study population of 93% females is reasonable but makes it almost impossible to find any gender specific differences.
Despite, the worldwide trend of people becoming more overweight and obese, the observed BMI in our study averaged 23.6 kg/m2. This is less than the average BMI of 26.01 kg/m2 for women in Germany [15], which might be related to the fact that horseback riding in Germany is expensive and an upper-class sport. The high rate of privately insured patients supports this theory. This may also be accentuated by the younger age (35.3 years) of the study population. The younger age of patients with horse-related injuries is a previously reported characteristic [9, 11, 16]. Additionally, in contrast to previous findings, that increasing BMI was associated with an increase in injury severity [17], in our study the AIS was not related to BMI.
Most studies report head trauma as the most common injury [1, 9, 10, 18]. Especially studies with its focus on children reported up to 30% head injuries [10, 16, 18]. In contrast hereto, only 10% of the patients in our study presented with head injuries, but our study combined children and adults. Additionally, Moss et al. reported already in 2002 a significant reduction of head injuries related to the development of improved protective helmets [9]. We could show that head injuries had the lowest AIS compared to other injuries. Still, traumatic brain injury remains the leading external cause of death [3, 19] and Lin et al. summed up, that in horseback riders traumatic brain injuries remain the most significant cause of mortality [20]. In line with that, in the current study one patient deceased due to traumatic brain injury with brainstem lesion. The resulting mortality rate (1%) of our study also reflects the mortality rate of equestrian related injuries of about 1% in previous studies [2, 7].
Falling from a horse was significantly related to spinal or pelvic injuries. Regarding spinal injuries previous studies reported more lumbar and thoracic than cervical spine injuries with a predominance of the thoracolumbar junction [6, 21] (Fig. 2). The average hospital admittance time (25 days) for spinal and pelvic injuries in our study was significantly longer than for other body regions but comparable to other European studies (11–43 days) [6]. The extended length of stay was caused by the significantly greater AIS and was accentuated by two patients with complete and incomplete tetraplegia after trauma to the cervical spine, who started early spinal rehabilitation. Previous studies also found 3% severely neurologically impaired patients [1]. This supports the conclusion by Lin et al., that in horseback riders spinal cord injuries are a significant cause of long-term morbidity [20].
In our study, injuries to the upper limb were the most common injuries. This is in concordance with other European studies from France, Austria, and Hungary [12, 22] and might reflect a difference in personal protective equipment. Moss et al. already described a decline in head injuries and an increase in the number and severity of upper limb injuries [9]. To our knowledge, no data exist comparing differences between nations or regions regarding the utilization of helmets. In a study by Kiss et al. Children in Austria wore a helmet in 70% compared to 43% in Hungary [22]. Abu-Zidan and Rao [7] reported a helmet use of 73% in an Australian study. Injuries to the upper extremity seemed to be less severe. Therefore, length of hospital stay was shortest for patients with upper extremity injuries. Surgery was performed in 34 patients (65.4%). Injuries involving the hand required surgery most frequently (35.3%). While many types of injuries are common for horseback-riding and grooming-related activities, literature regarding injuries to the fingers and thumb is sparse. Mangal et al. [23] reported one case with traumatic multi-finger amputations after trying to rein a horse. Abu-Zidan and Rao [7] reported seven patients (3%) that were entangled with reins and needed hospitalization, but did not report any injuries or treatment. The current study reveals that 10% of the injuries were caused by fingers tangled with reins or ropes (Fig. 3a, b). Most of them resulted in injuries to the ligaments and tendons, which could be reinserted in 40% of the cases. Still, three of them required an amputation (30%). The injury mechanism at it may be comparable to rodeo roping thumb injuries [24].
Lower limb injuries occurred in 20% of the patients. Altgärde et al. [13] reported 24% in adults and 19% in children. A US database query revealed 16.4% injured lower extremities [16]. Lower limb injuries were related to a kick from a horse or being trodden on a foot. To our knowledge, this has not been described before. This is supported by Lang et al. [11], who found a significantly greater number of lower extremity injuries in adults compared to children. This may be related to the fact, that adults are more involved in grooming and feeding.
We acknowledge the limitations of our study. The major limitation of this study was its retrospective design. While in the study by Lang et al. approximately 20% of the injuries occurred while working, the presented study was performed in an urban setting, where horseback riding is a popular recreational activity. Therefore, we are not able to report injury patterns for occupational activities. Additionally, due to the fact that our trauma center includes orthopedics, hand surgery, plastic surgery, and neurosurgery but no ENT department, isolated facial injuries treated by an ENT-specialist might be missed. Therefore, further data and studies are warranted.
Doctors should counsel patients involved in horseback riding to become thoroughly aware of the risks of equestrian-related sport and to understand the importance of appropriate training and safety gear [3].
Conclusion
Despite the fact that patients are young and healthy, horse related injuries must not be underestimated. In our study, almost two-thirds of the patients required inpatient treatment and 50% underwent surgery. We could show that patient age was related to injury severity according to the Abbreviated Injury Scale (AIS). Spinal and pelvic injuries were significantly related to a fall from a horse with a significantly greater trauma impact according to the AIS. Therefore, these severe entities need to be ruled out in such events. Accidents caused by holding the reins, may result in serious injuries to the hand with 30% requiring an amputation. Doctors need to be aware of possible horse-related injury patterns to reduce morbidity.
Availability of data and materials
All data are available within the manuscript.
References
Mutore K, Lim J, Fofana D, Torres-Reveron A. Hearing hoofbeats? Think head and neck trauma: a 10-year NTDB analysis of equestrian-related trauma in the USA. Trauma Surg Acute Care Open. 2021;6(1):e000728.
Van Balen PJ, Barten DG, Janssen L, Fiddelers AAA, Brink PR, Janzing HMJ. Beware of the force of the horse: mechanisms and severity of equestrian-related injuries. Eur J Emerg Med Off J Eur Soc Emerg Med. 2019;26(2):133–8.
Nelson DE, Bixby-Hammett D. Equestrian injuries in children and young adults. Am J Dis Child. 1992;146(5):611–4.
Thomas KE, Annest JL, Gilchrist J, Bixby-Hammett DM. Non-fatal horse related injuries treated in emergency departments in the United States, 2001–2003. Br J Sports Med. 2006;40(7):619–26.
Mayberry JC, Pearson TE, Wiger KJ, Diggs BS, Mullins RJ. Equestrian injury prevention efforts need more attention to novice riders. J Trauma. 2007;62(3):735–9.
Siebenga J, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, Patka P. Spine fractures caused by horse riding. Eur Spine J Off Publ Eur Spine Soc the Eur Spinal Deformity Soc Eur Sect Cerv Spine Res Soc. 2006;15(4):465–71.
Abu-Zidan FM, Rao S. Factors affecting the severity of horse-related injuries. Injury. 2003;34(12):897–900.
Ersatzkassen VD. Daten zum Gesundheitswesen: Versicherte. https://www.vdek.com/presse/daten/b_versicherte.html. Accessed 21 Sept 2022; 2022.
Moss PS, Wan A, Whitlock MR. A changing pattern of injuries to horse riders. Emerg Med J EMJ. 2002;19(5):412–4.
Gross I, Hadar A, Bala M, Hashavya S. The epidemiology, injury patterns and outcomes of horse-related injuries in Israeli children. Isr Med Assoc J IMAJ. 2019;21(4):279–82.
Lang J, Sathivelu M, Tetsworth K, Pollard C, Harvey K, Bellamy N. The epidemiology of horse-related injuries for different horse exposures, activities, and age groups in Queensland, Australia. J Trauma Acute Care Surg. 2014;76(1):205–12.
Laurent R, Uhring J, Bentahar M, Constantinou B, de Billy B, Langlais J. Epidemiology of equestrian injuries in children. Arch Pediatrie organe officiel de la Societe francaise de pediatrie. 2012;19(10):1053–7.
Altgarde J, Redeen S, Hilding N, Drott P. Horse-related trauma in children and adults during a two year period. Scand J Trauma Resusc Emerg Med. 2014;22:40.
Holtschmit JH. Verletzt im Sattel: Mit welchen Traumata plagen sich Reiter? (Injuries while mounted: What injuries bother horseback-riders?). https://www.gots.org/blog/2020/05/04/verletzt-im-sattel-mit-welchen-traumata-plagen-sich-reiter/. Accessed 09 July 2022.
Obesity TEAftSo. MEAN BODY MASS INDEX (BMI) IN ADULT WOMEN. https://easo.org/mean-body-mass-index-bmi-in-adult-women/. Accessed 8 Dec 2018.
Loder RT. The demographics of equestrian-related injuries in the United States: injury patterns, orthopedic specific injuries, and avenues for injury prevention. J Trauma. 2008;65(2):447–60.
Rupp JD, Flannagan CA, Leslie AJ, Hoff CN, Reed MP, Cunningham RM. Effects of BMI on the risk and frequency of AIS 3+ injuries in motor-vehicle crashes. Obesity. 2013;21(1):E88-97.
Wolyncewicz GEL, Palmer CS, Jowett HE, Hutson JM, King SK, Teague WJ. Horse-related injuries in children—unmounted injuries are more severe: a retrospective review. Injury. 2018;49(5):933–8.
Ingemarson H, Grevsten S, Thoren L. Lethal horse-riding injuries. J Trauma. 1989;29(1):25–30.
Lin CY, Wright J, Bushnik T, Shem K. Traumatic spinal cord injuries in horseback riding: a 35-year review. Am J Sports Med. 2011;39(11):2441–6.
Silver JR. Spinal injuries resulting from horse riding accidents. Spinal cord. 2002;40(6):264–71.
Kiss K, Swatek P, Lenart I, et al. Analysis of horse-related injuries in children. Pediatr Surg Int. 2008;24(10):1165–9.
Mangal R, Stead TG, Ganti L, Jasper T, Sleigh BC. Traumatic multi-finger amputations after trying to rein in a horse. Cureus. 2019;11(7): e5171.
Morgan RF, Nichter LS, Friedman HI, McCue FC 3rd. Rodeo roping thumb injuries. J Hand Surg. 1984;9(2):178–80.
Acknowledgements
We thank the Department of Hand- and Plastic Surgery for their support. We acknowledge support by the Open Access Publication Funds of the Ruhr-Universität Bochum.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MH wrote the main manuscript text and contributed to study concept/design, data analysis, and interpretation. MB and KW helped with data collection, interpretation and writing the paper. NK, BR, and TS helped with interpretation and contributed to review of the final manuscript and final submission of the paper. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee. Obtaining the informed consent from involved patients was waived by the Research Ethics Committee due to its retrospective design. All procedures involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
Consent for publication
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Competing interests
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hoffmann, M.F., Bernstorff, M., Kreitz, N. et al. Horse-related injury patterns: a single center report. J Orthop Surg Res 18, 83 (2023). https://doi.org/10.1186/s13018-023-03549-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03549-3