Abstract
Background
Hybrid construction (HC) may be an ideal surgical strategy than noncontinuous total disc replacement (TDR) and noncontinuous anterior cervical discectomy and fusion (ACDF) in the treatment of noncontinuous cervical spondylopathy. However, there is still no consensus on the segmental selection for ACDF or TDR in HC. The study aims to analyse the effects of different segment selection of TDR and ACDF on cervical biomechanical characteristics after HC surgery.
Methods
Twelve FEMs of C2–C7 were constructed based on CT images of 12 mild cervical spondylopathy volunteers. Two kinds of HC were introduced in our study: Fusion-arthroplasty group (Group 1), upper-level (C3/4) ACDF, and lower-level TDR (C5/6); Arthroplasty-fusion group (Group 2), upper-level (C3/4) TDR and lower-level ACDF (C5/6). The follow-load technique was simulated by applying an axial initial load of 73.6 N through the motion centre of FEM. A bending moment of 1.0 Nm was applied to the centre of C2 in all FEMs. Statistical analysis was carried out by SPSS 26.0. The significance threshold was 5% (P < 0.05).
Results
In the comparison of ROMs between Group 1 and Group 2, the ROM in extension (P = 0.016), and lateral bending (P = 0.038) of C4/5 were significantly higher in Group 1 group. The average intervertebral disc pressures at C2/3 in all directions were significantly higher in Group 1 than those in Group 2 (P < 0.005). The average contact forces in facet joints of C2/3 (P = 0.007) were significantly more than that in Group 2; however, the average contact forces in facet joints of C6/7 (P < 0.001) in Group 1 group were significantly less than that in Group 2.
Conclusions
Arthroplasty-fusion is preferred for intervertebral disc degeneration in adjacent upper segments. Fusion-arthroplasty is preferred for patients with lower intervertebral disc degeneration or lower posterior column degeneration.
Trial registration: This research was registered in Chinese Clinical Trial Registry (ChiCTR1900020513).
Similar content being viewed by others
Background
Cervical spondylopathy is a commonly seen degenerative spinal disease, which can decrease the patient’s motor function and quality of life [1]. Degenerative changes of cervical discs and ligamentous hypertrophy can attribute to chronic spinal cord compression and then lead to the progression of cervical spondylopathy [2]. Noncontinuous cervical spondylopathy is a special kind of multilevel cervical spondylopathy, the condition of which is the normal intermediate segment located between two noncontiguous degenerative segments [3].
Anterior cervical discectomy and fusion (ACDF) is the most widely used surgical method in the treatment of cervical spondylopathy, which can decompress nervous structures and achieve cervical realignment [4]. However, ACDF may increase the stress of intervertebral discs and endplates as well as facet joints overloading, which can cause adjacent segment degeneration (ASD) and cervical instability [5]. Previous studies ameliorated this procedure with skip-level ACDF, which included single segment titanium plates and self-locking cages or zero-p; it is reported that this method could achieve satisfactory clinical outcomes [6,7,8]. Although the intermediate segment is not fused in this procedure, it will stand with more additive stress from fused segments on the upper and lower sides, as well as compensative hypermobility for fused segments, which can accelerate intervertebral disc degeneration [3].
Cervical disc prosthesis, which is called cervical total disc replacement (TDR), can maintain physiological cervical movement instead of intervertebral fusion; this can decrease kinematic overloading at upper and lower adjacent segments [1]. TDR is usually carried out at the intervertebral level without instability or facet joint degeneration [9]. In addition, the facet joint can be overloaded at the TDR level, while the force transmission decreases at the adjacent levels [10, 11].
Hybrid construction (HC) combines TDR and ACDF together [9]. Previous studies yield that HC could provide ideal clinical outcomes and radiologic parameters; in addition, HC would not significantly change the total range of motion (ROM) or the ROM of adjacent segments [9, 12, 13]. HC may be an ideal surgical strategy than noncontinuous TDR and noncontinuous ACDF in the treatment of noncontinuous cervical spondylopathy. There is still no consensus on the segmental selection for the usage of ACDF or TDR in HC. Previous finite element analysis (FEA) simplified the vertebral distraction during the insertion of an intervertebral implant in the models, which could not simulate the real biomechanical environment [14]. In addition, most previous biomechanical studies just used the data of one case to draw a conclusion without statistical support, which could affect the accuracy of its conclusions [14,15,16].
To provide more convincing evidence for the implementation of HC, we performed FEA on the cervical biomechanical characteristics of noncontinuous cervical spondylopathy patients. The data obtained from FEA were statistically analysed. We hope that this study can analyse the effects of different segment selection of TDR and ACDF on cervical biomechanical characteristics after HC surgery.
Methods
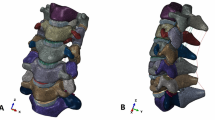
The geometry models
In this study, FEA technology is based on computed tomography (CT) images (SOMATOM Definition AS + , Siemens, Germany, a thickness of 0.75 mm and an interval of 0.69 mm) of the cervical spine (C2–C7) to build real clinical models, which is effective in construct finite element models (FEMs) from radiologic information [17]. This modelling technique can help surgeons make an optimal surgical strategy by predicting potential risks with satisfactory precision and effectiveness. Twelve mild cervical spondylopathy volunteers were included in this study (six male and six females), whose DICOM format CT images were fully achieved. These radiographic images were used to reconstruct geometric models of C2–C7 cervical vertebrae in Mimics 17.0 (Materialize Inc, Leuven, Belgium). The geometric models were output as STL files and then imported into Geomagic Studio 12.0 (3D System Corporation, Rock Hill, SC, USA) to adjust these models into physical structures.
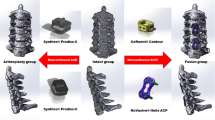
The implants analysed in this study included NuVasive® Helix ACP (NuVasive, Inc. San Diego, CA, USA), CoRoent® Contour (NuVasive, Inc., San Diego, CA, USA) and Prodisc-C (Synthes, Inc., West Chester, PA, USA). The basic information of implants is shown in Table 1. Solidworks 2016 (Dassault Systèmes, MA, USA) was used to build the FEMs of these devices and assemble them with cervical vertebra models. HC is different from hybrid decompression. The utility of cervical discectomy and corpectomy is called hybrid decompression [18,19,20]. Therefore, we should not confuse these two concepts. Considering intermediate C4/5 got the most attention in the previous studies on noncontinuous cervical spondylopathy, C3/4 and C5/6 were selected to perform HC in our study [3, 14, 17]. Two kinds of HC were introduced in our study: Fusion-Arthroplasty group (Group 1), upper-level (C3/4) ACDF and lower-level TDR (C5/6); Arthroplasty-Fusion group (Group 2), upper-level (C3/4) TDR and lower-level ACDF (C5/6). All the models were used to perform these different HC strategies in the software mentioned above. In ACDF, NuVasive® Helix ACP and CoRoent® Contour were implanted at intervertebral level after removing relevant intervertebral disc, anterior longitudinal ligament (ALL), and posterior longitudinal ligament (PLL). In TDR, we implanted Prodisc-C at the corresponding level after the resection of relevant intervertebral junctional structures (Fig. 1). In practice, the posterior longitudinal ligament should be removed from the implanted segment to achieve adequate decompression of the neural structure. The models in this study simulated the actual surgical procedure; therefore, they required the removal of the posterior longitudinal ligaments at the implanted segments.
Hypermesh 12.0 (Altair, Troy, MI, USA) was used to construct high-quality meshes of these models. Material properties, experimental conditions, and FEA were then set and carried out in ABAQUS 6.13 (Dassault Systems Corporation, MA, USA).
Material properties
Material properties and element types are shown in Table 2 [15, 17, 21,22,23]. In these FEMs, the thickness of cortical shell and endplates was set as 0.4 mm [24]. As to the facet joint, the articular surface was covered with cartilage, which was assigned with nonlinear surface-to-surface contact; the thickness of cartilage and the gap were 0.5 mm [14]. The structure of the intervertebral disc is as follows: Nucleus occupied about 40% volume of the intervertebral discs, and the annulus was around 60%; annulus fibres accounted for about 19% of the annulus fibrosus volume; the inclination of the annulus fibrosus to the transverse plane was 15° to 30°; a tie connection was defined between the parts of intervertebral discs and endplates [3, 14]. In addition, six groups of ligaments included ALL, PLL, ligament flavum (LF), interspinous ligament (IL), supraspinous ligament (SL), and capsular ligament (CL); all of them were inserted into the model [15, 25].
Experimental condition
The interfaces between natural structures of the cervical spine were assigned with a tie constraint; the contact of facet joints was set to a friction sliding; the C7 bottom surface was set to completely constrained in all degrees of freedom [24]. The simulation of screw-vertebra interface and screw-implant interface was set to a tie constraint; the interface between the cancellous bone graft and CoRoent® Contour was assigned with a frictionless contact; end plates and nucleus of ProDisc-C were set to have full surface contact with a tie constraint [17, 21]. The follow-load technique was simulated by applying an axial initial load of 73.6 N through the motion centre of FEM, which was equivalent to muscle forces and head weight; the motion of the entire C2–C7, including flexion, extension, lateral bending, and axial rotation under the bending moment of 1.0 Nm was applied to the centre of C2 in all FEMs to simulate flexion, extension, lateral bending and axial rotation of entire C2–C7 [10]. The ROM of each intervertebral level was achieved and compared with the published data to validate the reliability of our FEMs [10, 17, 26,27,28]. This study was concerned with the analysis of assemblies with connection joints or contact conditions. The traditional manual H-element convergence method was used in this study. In addition, the second-order mass element level default element size was used in this study. The initial mesh control was used in this study to ensure that the geometry was consistent with the undeformed. Finally, this study used a local grid to control the desired location to achieve convergence. All FEMs in this study were treated as above.
Statistical analysis
Statistical analysis was carried out using Statistical Package for the Social Sciences version 26.0 software (SPSS, Inc, Chicago, IL). Mean ± standard deviation (SD) was used to report continuous variables. Normality was tested via the Shapiro–Wilk test. Wilcoxon rank-sum test was used to analyse variables that were not normally distributed. Normally distributed variables were analysed by Student’s t test. The significance threshold was 5% (P < 0.05).
Results
ROM at different levels
The predicted ROM of C2-C7 FEMs was compared with the published data from previous studies (Fig. 2) [10, 17, 26,27,28]. The average ROMs of intact FEM from C2/3 to C6/7 were in good agreement with previous studies. A comparison of ROMs at different intervertebral levels between the intact group, Group 1, and Group 2 is shown in Table 3. The results showed that the ROMs in lateral bending at the arthroplasty segments were significantly more than that of the corresponding segment under physiological conditions (P < 0.05). In the comparison of ROMs between Group 1 and Group 2, the usage of arthroplasty at C5/6 could significantly increase the ROMs of the distal adjacent segment in extension (P = 0.015); in addition, the implant of arthroplasty at C3/4 could significantly increase the ROMs of the proximal adjacent segment in lateral bending (P = 0.039). The difference in ROMs between implant segments was related to the biomechanical characteristics of implants. No significant difference was found in total ROM between Group 1 and Group 2. This suggested that both treatment strategies had similar effects on the overall ROMs of the cervical spines.
Intervertebral disc pressures
Table 4 shows the average pressures in intervertebral discs at different levels. The average intervertebral disc pressures of C2/3, C4/5, and C6/7 in Group 1 were significantly higher than that in the intact group in all directions (P < 0.005). In comparison between the intact group and Group 2, the average intervertebral disc pressures in Group 2 were significantly higher than that in the intact group (P < 0.005); however, no between-group difference was found at C2/3 in all directions (P > 0.005). The average intervertebral disc pressures at C2/3 were significantly higher in Group 1 than those in Group 2 in all directions (P < 0.005).
Contact forces and pressures of facet joints
Table 5 shows the comparison of average contact forces in facet joints in extension between the intact group, Group 1, and Group 2. Compared with intact group, average contact forces in facet joints of C2/3 (P < 0.001), C4/5 (P < 0.001) and C6/7 (P < 0.001) were significantly higher in Group 1. Similarly, average contact forces in facet joints of C2/3 (P = 0.030), C4/5 (P = 0.005) and C6/7 (P < 0.001) were significantly higher in Group 2 than that in intact group. The average contact forces in facet joints of C2/3 (P = 0.007) were significantly more than that in Group 2; however, the average contact forces in facet joints of C6/7 (P < 0.001) in Group 1 were significantly less than that in Group 2 group. Table 6 shows the comparison of average contact pressures in facet joints in extension between the intact group, Group 1, and Group 2. Compared with intact group, average contact pressures in facet joints of C2/3 (P < 0.001) and C4/5 (P < 0.001) were significantly higher in Group 1 and Group 2 (P = 0.030 and P < 0.001, respectively); however, average contact pressures in facet joints of C6/7 (P < 0.001) were significantly less in Group 2 than those in Intact group. In comparison between Group 1 and Group 2, average contact pressures in facet joints of C2/3 (P = 0.007) were significantly less in Group 2, while average contact pressure in facet joints of C6/7 (P < 0.001) was significantly higher in Group 1.
Discussion
The selection of surgical strategy in the treatment of noncontinuous cervical spondylopathy remains controversial, the difficulty of which lies in the preservation of intermedial intervertebral disc [14, 26]. It is reported that noncontinuous ACDF may theoretically bear additive stress from upper and lower fused levels with hypermobility in compensation, which will accelerate intervertebral disc degeneration [3, 29]. To decrease additive stress from fusion massed on the normal intermediate segment, long segmental anterior fusion is usually carried out in the treatment of noncontinuous cervical spondylopathy; long segmental anterior fusion always includes the intermediate segments [3]. However, this method is associated with a high risk of ASD and nonunion.
It is reported that noncontinuous TDR is a safe and effective treatment of noncontinuous cervical spondylopathy [8]. However, in multilevel TDR, the indication is more restricted, the technique is difficult, the prosthesis-related complication rate is high, and the cost is expensive [3, 30]. Our previous study showed that noncontinuous TDR required high biomechanical stability of the lower intervertebral level. This is because the stability of biomechanical structure and appropriate physiological curvature of the cervical spine could be required by noncontinuous TDR. Therefore, TDR is not suitable for patients with lower adjacent intervertebral disc degeneration [17]. HC contains the technical characteristics of ACDF and TDR. Therefore, it may be a good surgical strategy to solve the above problems.
The implementation of HC is still controversial. Most related studies apply HC in the treatment of C3 to C7 continuous cervical spondylopathy, which failed in the conservative treatment for more than six weeks [31]. In making optimal surgical strategy preoperatively, compensation of ROM, intervertebral stress, and facet joint force at adjacent levels should be taken into consideration [32].
Most previous studies used one sample, while anatomical differences could influence the ROM, intervertebral disc stress, and facet force [33, 34]. Therefore, multiple models were included in this study for statistical analysis to improve the accuracy of the conclusions. Our study showed that compared with intact FEM, HC mainly changed cervical movement characteristics in lateral bending and decreased the overall motion of the cervical spine. The possible reason is that ACDF changes the curvature of the cervical spine so that the cervical rotation centre shifts, and then the tension of cervical ligaments is increased by distraction [9, 35]. We found that the hypermobility of the intermedial intervertebral disc of Group 1 was more obvious than in Group 2, which implied that the protective effect of Group 1 on the intermedial intervertebral segment is weak.
In our study, average pressures in cervical intervertebral discs significantly increased after Group 1; however, Group 2 did not significantly change the physiological intervertebral disc pressure at the upper adjacent levels (C2/3). This suggests that Group 2 is closer to the physiological cervical biomechanical characteristics; Group 1 and Group 2 had similar effects on the average intervertebral disc pressure at the intermedial level (C4/5). Considering the mobility of the intermedial intervertebral disc of Group 1 was higher than Group 2, the protective effect of Group 1 on the intermedial intervertebral disc might be achieved by increasing segmental ROM to buffer the intervertebral disc pressure [24].
In this study, Group 1 could significantly reduce the contact forces in the facet joints of the lower adjacent segments, which implied Group 1 was suitable for patients with posterior column degeneration in lower adjacent segments. However, this was at the cost of increasing the contact forces of the upper adjacent facet joints. Both Group 1 and Group 2 could increase the contact forces in the intermedial facet joints. This indicates that neither surgical procedure is suitable for patients with severe posterior column degeneration at intermedial levels. In contrast, Wu et al. [26] reported that the biomechanical characteristics of the untreated segments were less influenced by HC. The reason might be that their study did not simulate the insertion procedure of implants; this would ignore the distraction of vertebrae after inserting implants. In addition, they discussed the HC, which included Zero-P and Prestige-LP. The design of Zero-P makes it difficult to improve cervical lordosis, especially in ACDF with multiple segments [36]. Prestige-LP can produce higher von Mises stress than Prodisc-C at the posterior flanges on the end plate [21]. Therefore, the satisfactory biomechanical characteristics obtained in the treatment of noncontinuous cervical spondylopathy with the above-mentioned HC are at the expense of increasing the internal stress of implants. These two implants may not be recommended for this type of procedure. There are still some limitations in this study, which require further improvement in future work. First, although image data of 12 volunteers are included in this study for modelling, it is difficult to completely simulate the changes in biomechanical characteristics of intervertebral disc degeneration. Second, the depth of implants has a great impact on the cervical biomechanical properties after HC. In this study, only standardized implant depth can be used for analysis; it is difficult to carry out an in-depth discussion on a more complex situation. Therefore, we can only use FEA to study the trend of biomechanical characteristics of the FEMs. In future studies, we will use artificial intelligence technology-assisted FEA to improve research methods, hoping to further improve the accuracy.
Conclusions
The results of our study show that HC has high requirements on biomechanical characteristics of unoperated cervical vertebra segments in the treatment of noncontinuous cervical spondylopathy. The protective effect of fusion-arthroplasty on the intermedial intervertebral segments is weak. Arthroplasty-fusion is closer to the physiological cervical biomechanical characteristics in the upper adjacent segments. Therefore, Arthroplasty-fusion is preferred for intervertebral disc degeneration in adjacent upper segments. Fusion-arthroplasty can significantly reduce the average pressures in intervertebral discs and contact forces of facet joints at lower adjacent segments. Therefore, fusion-arthroplasty is preferred for the treatment of patients with lower intervertebral disc degeneration or lower posterior column degeneration.
Availability of data and materials
Please contact author for data requests.
Abbreviations
- ACDF:
-
Anterior cervical discectomy and fusion
- ASD:
-
Adjacent segment degeneration
- TDR:
-
Total disc replacement
- HC:
-
Hybrid construction
- ROM:
-
Range of motion
- FEA:
-
Finite element analysis
- CT:
-
Computed tomography
- FEM:
-
Finite element model
- ALL:
-
Anterior longitudinal ligament
- PLL:
-
Posterior longitudinal ligament
- LF:
-
Ligament flavum
- IL:
-
Interspinous ligament
- SL:
-
Supraspinous ligament
- CL:
-
Capsular ligament
- SD:
-
Mean ± standard deviation
References
Lee SB, Cho KS, Kim JY, Yoo DS, Lee TG, Huh PW. Hybrid surgery of multilevel cervical degenerative disc disease: review of literature and clinical results. J Korean Neurosurg Soc. 2012;52(5):452–8. https://doi.org/10.3340/jkns.2012.52.5.452.
Morishita Y, Maeda T, Ueta T, Naito M, Shiba K. Dynamic somatosensory evoked potentials to determine electrophysiological effects on the spinal cord during cervical spine extension: clinical article. J Neurosurg Spine. 2013;19(3):288–92. https://doi.org/10.3171/2013.5.SPINE12933.
Wu TK, Wang BY, Cheng D, Rong X, Lou JG, Hong Y, Liu H. Clinical and radiographic features of hybrid surgery for the treatment of skip-level cervical degenerative disc disease: a minimum 24-month follow-up. J Clin Neurosci. 2017;40:102–8. https://doi.org/10.1016/j.jocn.2017.02.030.
Miyamoto H, Maeno K, Uno K, Kakutani K, Nishida K, Sumi M. Outcomes of surgical intervention for cervical spondylotic myelopathy accompanying local kyphosis (comparison between laminoplasty alone and posterior reconstruction surgery using the screw-rod system). Eur Spine J. 2014;23(2):341–6. https://doi.org/10.1007/s00586-013-2923-1.
Wang KF, Duan S, Zhu ZQ, Liu HY, Liu CJ, Xu S. Clinical and radiologic features of 3 reconstructive procedures for the surgical management of patients with bilevel cervical degenerative disc disease at a minimum follow-up period of 5 years: a comparative study. World Neurosurg. 2018;113:e70–6. https://doi.org/10.1016/j.wneu.2018.01.157.
Wang HR, Li XL, Dong J, Yuan FL, Zhou J. Skip-level anterior cervical discectomy and fusion with self-locking stand-alone PEEK cages for the treatment of 2 noncontiguous levels of cervical spondylosis. J Spinal Disord Tech. 2013;26(7):E286–92. https://doi.org/10.1097/BSD.0b013e31828679b3.
Shi S, Liu ZD, You WJ, Ouyang YP, Li XF, Qian L, Zhong GB. Application of a stand-alone anchored spacer in noncontiguous anterior cervical arthrodesis with radiologic analysis of the intermediate segment. J Clin Neurosci. 2016;25:69–74. https://doi.org/10.1016/j.jocn.2015.05.050.
Qizhi S, Lei S, Peijia L, Hanping Z, Hongwei H, Junsheng C, Jianmin L. A comparison of zero-profile devices and artificial cervical disks in patients with 2 noncontiguous levels of cervical spondylosis. Clin Spine Surg. 2016;29(2):E61–6. https://doi.org/10.1097/BSD.0000000000000096.
Yilmaz M, Yucesoy K, Erbayraktar RS, Altinag RS. Anterior hybrid construction of multilevel cervical disc disease and spondylotic spinal stenosis: surgical results and factors affecting adjacent segment problems. J Orthop Surg Res. 2021;16(1):298. https://doi.org/10.1186/s13018-021-02393-7.
Lee JH, Park WM, Kim YH, Jahng TA. A biomechanical analysis of an artificial disc with a shock-absorbing core property by using whole-cervical spine finite element analysis. Spine. 2016;41(15):E893–901. https://doi.org/10.1097/BRS.0000000000001468.
Faizan A, Goel VK, Biyani A, Garfin SR, Bono CM. Adjacent level effects of bilevel disc replacement, bi level fusion and disc replacement plus fusion in cervical spine–a finite element based study. Clin Biomech (Bristol, Avon). 2012;27(3):226–33. https://doi.org/10.1016/j.clinbiomech.2011.09.014.
Chen J, Xu L, Jia YS, Sun Q, Li JY, Zheng CY, Bai CX, Yu QS. Cervical anterior hybrid technique with bi-level Bryan artificial disc replacement and adjacent segment fusion for cervical myelopathy over three consecutive segments. J Clin Neurosci. 2016;27:59–62. https://doi.org/10.1016/j.jocn.2015.07.030.
Boddapati V, Lee NJ, Mathew J, Vulapalli MM, Lombardi JM, Dyrszka MD, Sardar ZM, Lehman RA, Riew KD. Hybrid anterior cervical discectomy and fusion and cervical disc arthroplasty: an analysis of short-term complications, reoperations, and readmissions. Glob Spine J. 2021;11(8):1183–9. https://doi.org/10.1177/2192568220941453.
Wu TK, Meng Y, Liu H, Wang BY, Hong Y, Rong X, Ding C, Chen H. Biomechanical effects on the intermediate segment of noncontiguous hybrid surgery with cervical disc arthroplasty and anterior cervical discectomy and fusion: a finite element analysis. Spine J. 2019;19(7):1254–63. https://doi.org/10.1016/j.spinee.2019.02.004.
Ouyang P, Lu T, He X, Gao Z, Cai X, Jin Z. Biomechanical comparison of integrated fixation cage versus anterior cervical plate and cage in anterior cervical corpectomy and fusion (ACCF): a finite element analysis. Med Sci Monit. 2019;25:1489–98. https://doi.org/10.12659/MSM.913630.
Wong CE, Hu HT, Hsieh MP, Huang KY. Optimization of three-level cervical hybrid surgery to prevent adjacent segment disease: a finite element study. Front Bioeng Biotechnol. 2020;8:154. https://doi.org/10.3389/fbioe.2020.00154.
Sun X, Sun S, Zhang T, Kong C, Wang W, Lu S. Biomechanical comparison of noncontiguous cervical disc arthroplasty and noncontiguous cervical discectomy and fusion in the treatment of noncontinuous cervical degenerative disc disease: a finite element analysis. J Orthop Surg Res. 2020;15(1):36. https://doi.org/10.1186/s13018-020-1549-3.
Liu JM, Peng HW, Liu ZL, Long XH, Yu YQ, Huang SH. Hybrid decompression technique versus anterior cervical corpectomy and fusion for treating multilevel cervical spondylotic myelopathy: which one is better? World Neurosurg. 2015;84(6):2022–9. https://doi.org/10.1016/j.wneu.2015.08.039.
Odate S, Shikata J, Kimura H, Soeda T. Hybrid decompression and fixation technique versus plated 3-vertebra corpectomy for 4-segment cervical myelopathy: analysis of 81 cases with a minimum 2-year follow-up. Clin Spine Surg. 2016;29(6):226–33. https://doi.org/10.1097/BSD.0b013e31827ada34.
Ashkenazi E, Smorgick Y, Rand N, Millgram MA, Mirovsky Y, Floman Y. Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosurg Spine. 2005;3(3):205–9. https://doi.org/10.3171/spi.2005.3.3.0205.
Lin CY, Kang H, Rouleau JP, Hollister SJ, Marca FL. Stress analysis of the interface between cervical vertebrae end plates and the Bryan, Prestige LP, and ProDisc-C cervical disc prostheses: an in vivo image-based finite element study. Spine. 2009;34(15):1554–60. https://doi.org/10.1097/BRS.0b013e3181aa643b.
Mo Z, Li Q, Jia Z, Yang J, Wong DW, Fan Y. Biomechanical consideration of prosthesis selection in hybrid surgery for bi-level cervical disc degenerative diseases. Eur Spine J. 2017;26(4):1181–90. https://doi.org/10.1007/s00586-016-4777-9.
Mo Z, Zhao Y, Du C, Sun Y, Zhang M, Fan Y. Does location of rotation center in artificial disc affect cervical biomechanics? Spine. 2015;40(8):E469–75. https://doi.org/10.1097/BRS.0000000000000818.
Manickam PS, Roy S. The biomechanical study of cervical spine: a finite element analysis. Int J Artif Organs. 2022;45(1):89–95. https://doi.org/10.1177/0391398821995495.
Rong X, Wang B, Ding C, Deng Y, Chen H, Meng Y, Yan W, Liu H. The biomechanical impact of facet tropism on the intervertebral disc and facet joints in the cervical spine. Spine J. 2017;17(12):1926–31. https://doi.org/10.1016/j.spinee.2017.07.009.
Wu TK, Meng Y, Wang BY, Rong X, Hong Y, Ding C, Chen H, Liu H. Biomechanics following skip-level cervical disc arthroplasty versus skip-level cervical discectomy and fusion: a finite element-based study. BMC Musculoskelet Disord. 2019;20(1):49. https://doi.org/10.1186/s12891-019-2425-3.
Liu Q, Guo Q, Yang J, Zhang P, Xu T, Cheng X, Chen J, Guan H, Ni B. Subaxial cervical intradiscal pressure and segmental kinematics following atlantoaxial fixation in different angles. World Neurosurg. 2016;87:521–8. https://doi.org/10.1016/j.wneu.2015.09.025.
Panjabi MM, Crisco JJ, Vasavada A, Oda T, Cholewicki J, Nibu K, Shin E. Mechanical properties of the human cervical spine as shown by three-dimensional load-displacement curves. Spine. 2001;26(24):2692–700. https://doi.org/10.1097/00007632-200112150-00012.
Visocchi M, Marino S, Ducoli G, Barbagallo G, Ciappetta P, Signorelli F. Hybrid implants in anterior cervical decompressive surgery for degenerative disease. J Craniovertebr Junction Spine. 2021;12(1):54–60. https://doi.org/10.4103/jcvjs.JCVJS_184_20.
Ren X, Chu T, Jiang T, Wang W, Wang J, Li C, Zhang Z. Cervical disk replacement combined with cage fusion for the treatment of multilevel cervical disk herniation. Clin Spine Surg. 2016;29(6):218–25. https://doi.org/10.1097/BSD.0b013e31826994bb.
Cho BY, Lim J, Sim HB, Park J. Biomechanical analysis of the range of motion after placement of a two-level cervical ProDisc-C versus hybrid construct. Spine. 2010;35(19):1769–76. https://doi.org/10.1097/BRS.0b013e3181c225fa.
Zhang J, Meng F, Ding Y, Li J, Han J, Zhang X, Dong W. Hybrid surgery versus anterior cervical discectomy and fusion in multilevel cervical disc diseases: a meta-analysis. Medicine (Baltimore). 2016;95(21):e3621. https://doi.org/10.1097/MD.0000000000003621.
Herron MR, Park J, Dailey AT, Brockmeyer DL, Ellis BJ. Febio finite element models of the human cervical spine. J Biomech. 2020;113:110077. https://doi.org/10.1016/j.jbiomech.2020.110077.
Mumtaz M, Zafarparandeh I, Erbulut DU. Investigation into cervical spine biomechanics following single, multilevel and hybrid disc replacement surgery with dynamic cervical implant and fusion: a finite element study. Bioengineering (Basel). 2022. https://doi.org/10.3390/bioengineering9010016.
Lee MJ, Dumonski M, Phillips FM, Voronov LI, Renner SM, Carandang G, Havey RM, Patwardhan AG. Disc replacement adjacent to cervical fusion: a biomechanical comparison of hybrid construct versus two-level fusion. Spine. 2011;36(23):1932–9. https://doi.org/10.1097/BRS.0b013e3181fc1aff.
Chen Y, Liu Y, Chen H, Cao P, Yuan W. Comparison of curvature between the zero-p spacer and traditional cage and plate after 3-level anterior cervical discectomy and fusion: mid-term results. Clin Spine Surg. 2017;30(8):E1111–6. https://doi.org/10.1097/BSD.0000000000000440.
Acknowledgements
This research was performed mainly in Xuanwu Hospital Capital Medical University, National Clinical Research Center for Geriatric Diseases and the PLA General Hospital. The data analysis in this study was mainly done in Beijing Glitzern Technology Co., Ltd.
Funding
This study was funded by Beijing Hospitals Authority Youth Programme (QML20210805), Beijing Key Laboratory of Applied Biomechanics Research Open Project in 2022 (2022KF03), National Natural Youth Cultivation Program of 2021 in Xuanwu Hospital Capital Medical University (QNPY2021018), and Research and Cultivation Fund of Capital Medical University (1220010144).
Author information
Authors and Affiliations
Contributions
XS, QZ, LC, JW and JH designed this research and built the FEMs. ZS, YL and YZ collected the CT images. WT and SL carried out the FEA. YC recruited volunteers. SS edited the tables and figures. All authors participated in the writing and revision of this article.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by Ethics Committee of the Xuanwu Hospital Capital Medical University (clinical study review [2018] 083). This research was registered in Chinese Clinical Trial Registry (ChiCTR1900020513). All volunteers included in this study provided their informed consent at the enrolment on the use of their data for research.
Consent for publication
All authors agreed to publish this article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, X., Zhang, Q., Cao, L. et al. Biomechanical effects of hybrid constructions in the treatment of noncontinuous cervical spondylopathy: a finite element analysis. J Orthop Surg Res 18, 57 (2023). https://doi.org/10.1186/s13018-023-03537-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03537-7