Abstract
Background
A novel nanohydroxyapatite/polyamide-66 cage (n-HA/PA66 cage) with a horseshoe shape was designed to lower the subsidence rate of the traditional hollow cylindrical n-HA/PA66 cage. However, no studies have compared the incidence of subsidence in the two cages. The purpose of this study was to compare the long-term clinical and radiological outcomes of the novel n-HA/PA66 cage with the hollow cylindrical n-HA/PA66 cage after anterior cervical discectomy and fusion (ACDF) to treat single-level cervical degenerative disk disease (CDDD).
Methods
Fifty-two patients with novel n-HA/PA66 cages (Group A) and fifty-five patients with hollow cylindrical n-HA/PA66 cages (Group B) were included. The radiological parameters included intervertebral height (IH), C2-7 angle (C2-7a), segmental alignment (SA), subsidence rate, and fusion rate. The clinical outcomes were visual analog scale (VAS) scores, Japanese Orthopedic Association (JOA) scores, and patient satisfaction rates.
Results
The pre- and postoperative SA, C2-7a, and fusion rates of the patients in Groups A and B were similar. The preoperative and 6-month postoperative IHs in both groups were comparable. However, the final follow-up IH in Group B was significantly smaller than that in Group A (35.9 mm vs. 36.7 mm). The difference in the subsidence rates at the final follow-up between Group A (5.8%, 3/52) and Group B (18.2%, 10/55) was significant. The VAS score, JOA score, and patient satisfaction rate were not significantly different.
Conclusions
The novel n-HA/PA66 cage had similar favorable SA, C2-7a, fusion rate, and clinical outcomes compared to the hollow cylindrical n-HA/PA66 cage for treating single-level ACDF. Moreover, the novel n-HA/PA66 cage achieved a lower subsidence rate and higher IH than the hollow cylindrical n-HA/PA66 cage at the final follow-up.
Similar content being viewed by others
Introduction
With the aging of the population, the incidence of cervical degenerative disk disease (CDDD) is significantly increasing [1, 2]. The main complaints of CDDD are neck pain, myelopathy, and/or radiculopathy, which impair the professional capability and daily life of patients [3].
Robinson and Smith first reported anterior cervical discectomy and fusion (ACDF) in the 1950s, and it evolved to be the most commonly used method for the surgical treatment of CDDD [4, 5]. The surgical procedure of ACDF has been relatively standard over the decades since its introduction. The focus has been for improvements through the alterations of the intervertebral cage with different materials and designs [6].
Currently, Titanium and PEEK are two materials primarily used to produce cervical intervertebral cages. Titanium has good biocompatibility, but it is radiopaque and has a relatively high elastic modulus, which could lead to stress shielding and a high subsidence rate [7]. PEEK can achieve suitable biomechanical support and radiolucency, but its disadvantage is its intrinsic bioinertness [8, 9].
The hollow cylindrical nanohydroxyapatite/polyamide-66 cage (n-HA/PA66, Sichuan National Nano Technology Co., Ltd. Chengdu, Sichuan) is composed of nanohydroxyapatite and polyamide-66, and its biomechanical properties are found to match well with those of natural bone [10, 11]. The high n-HA content in the composites determines the favorable biocompatibility and bioactivity of the n-HA/PA66 cage [11]. The clinical and radiological outcomes of the hollow cylindrical n-HA/PA66 cages used in ACDF for the treatment of CDDD patients were suggested to be satisfactory in both short- and long-term follow-up [9, 12]. However, the n-HA/PA66 cage has relatively high subsidence rates (10.6%) during long-term follow-up, which could lead to cervical kyphosis, neural foramen stenosis, and yellow ligament folds after surgery [9, 10].
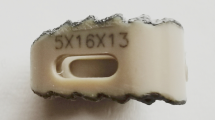
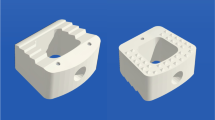
Previous studies have demonstrated that the morphology of the cage might be one of the most important factors related to the incidence of subsidence [13,14,15]. Hence, to decrease the incidence of subsidence, the morphology of the n-HA/PA66 cage was redesigned (the novel n-HA/PA66 cage). The novel n-HA/PA66 cage is a horseshoe-shaped cage with a more suitable shape and larger bone graft volume than the hollow cylindrical n-HA/PA66 cage (Fig. 1). Nevertheless, to our knowledge, no studies have compared the subsidence rates of the novel n-HA/PA66 cage and the hollow cylindrical n-HA/PA66 cage. Therefore, the purpose of this study was to compare the long-term clinical and radiological outcomes of the novel n-HA/PA66 cage with the hollow cylindrical n-HA/PA66 cage after ACDF for the treatment of single-level CDDD.
Materials and methods
This study was a retrospective study that was approved by the ethics committee of West China Hospital of Sichuan University, and informed consent was obtained from the patients. All methods were carried out in accordance with relevant guidelines and regulations.
Fifty-two patients with CDDD who underwent single-level ACDF with the novel n-HA/PA66 cage (Group A) in our department between January 2013 and July 2015 were included. Fifty-five patients with hollow cylindrical n-HA/PA66 cages (Group B) placed after ACDF were also included for comparison. The inclusion criteria were as follows: (1) radiculopathy and/or myelopathy from single-level cervical disk herniation, (2) no response to 3 months of nonsurgical management, and (3) no previous spine surgery. The exclusion criteria were (1) previous spine surgery, (2) active infection, and (3) inflammatory spondyloarthropathies. All patients were followed up for at least 7 years.
All surgeries for all patients in this study were accomplished by the same surgeon and by following standard surgical procedures [4, 16]. All procedures were performed in supine position and through a transverse skin incision on the right side of the neck. After resecting the cartilage of the endplates at the operation level and removing the osteophytes as well as the ruptured posterior longitudinal ligament, a suitable cage filled with morselized bone from local decompression was inserted into the intervertebral space. The operated level was then stabilized by an ATLANTIS Anterior Cervical Plate System (Medtronic Sofamor Danek USA, Inc. Memphis, TN). All patients were told to wear a cervical collar for 6 weeks postoperatively.
Frontal and lateral radiographs and three-dimensional CT (3d-CT) of the cervical spine were obtained preoperatively, 6 months postoperatively, and at final follow-up (Fig. 2). The following parameters obtained from lateral radiography were used to evaluate the radiological outcomes: intervertebral height (IH); the distance from the midpoint of the superior endplate of the upper vertebrae to the midpoint of the inferior endplate of the lower vertebrae; C2-7 angle (C2-7a); the Cobb angle between the C2 and C7 vertebrae; segmental alignment (SA); and the Cobb angle between the upper and lower vertebra of the implanted level. Negative values were defined as kyphosis, while positive values were defined as lordosis. The loss of IH > 2 mm was regarded as subsidence [9]. The fusion status was evaluated on 3D-CT by the 5-grade criteria proposed by Brantigan and Steffee [17]: grade 4 or 5 were defined as fused; Grade 3 was defined as uncertain; Grade 1 or 2 were defined as unfused.
The clinical outcomes were evaluated by the visual analog scale (VAS) and Japanese Orthopedic Association (JOA) scores preoperatively, 6 months postoperatively, and at the final follow-up. We also collected the patient satisfaction levels at the final follow-up: very satisfied, somewhat satisfied, somewhat dissatisfied, and very dissatisfied [5].
Statistical analysis was performed by using SPSS 22.0 (IBM Corp., Armonk, NY, USA). Quantitative variables were expressed as the mean ± standard deviation and analyzed by Student’s t test or the Mann‒Whitney U test as appropriate. The χ2 test or Fisher’s exact test was used to analyze categorical variables. Statistical significance was set at P < 0.05.
Results
The average follow-up time of the 107 included patients was 96.1 ± 7.5 months. The demographic data (age, sex, smoking status, operative time, and blood loss) of the patients in Group A and Group B were comparable (Table 1). In this study, the operative segments included C3/4, C4/5, C5/6, and C6/7. The difference in the proportions of the different operative segments between Group A and Group B was not significant (Table 1).
The radiological outcomes of the patients in Group A and Group B are listed in Table 2. The SA and C2-7a of the patients in both groups were significantly improved at 6 months postoperatively and at the final follow-up. No significance was found regarding pre- and postoperative SA and C2-7a between Group A and Group B. The fusion rates at 6 months postoperatively (57.6%) and final follow-up (98.0%) in Group A were similar to those in Group B (56.3% at 6 months postoperatively and 96.3% at final follow-up, respectively). The preoperative and 6-month postoperative IHs in Group A and Group B were comparable. However, the IH at the final follow-up in Group B was significantly smaller than that in Group A (35.9 mm vs. 36.7 mm). No subsidence was observed at 6 months follow-up in either group, but the difference in the subsidence rates between Group A (5.8%, 3/52) and Group B (18.2%, 10/55) at the final follow-up was significant (P < 0.05).
Table 3 shows the clinical outcomes of the patients in Group A and Group B. The JOA and VAS scores of the patients in both groups were relieved postoperatively and were further improved at the final follow-up. No significant differences were found in the VAS score and JOA score of the patients in Group A and Group B during the different periods (preoperatively, 6 months postoperatively, and at the final follow-up). The proportion of patients who were very satisfied or somewhat satisfied in Group A was 90.4% (47/52), which was similar to that in Group B (89.1%, 49/55).
Discussion
HA is the main inorganic phase of the bone matrix, so it is widely applied to make scaffolds for bone tissue repair [18]. PA66 is a form of opalescent crystalline polymer with excellent mechanical properties (good elasticity, strength, and high elongation), and its unique molecular structure is beneficial for its modification [19]. The nHA crystals and the carboxy and amide groups of PA66 are similar to bone apatite and collagen, respectively, so the n-HA/PA66 composites were used to mimic natural bone in previous studies. They found that the physical, chemical, and mechanical characteristics of n-HA/PA66 match well with those of natural bone [11]. The biocompatibility and oseogenesis of the n-HA/PA66 composite scaffolds were also indicated to be good both in vitro and in vivo [20].
The n-HA/PA66 cage used in ACDF was firstly designed as a hollow cylindrical shape and some scholars has reported its clinical and radiological outcomes. Yang et al. [12] investigated the outcomes for the use of hollow cylindrical n-HA/PA66 cages for single-level ACDF and concluded that the hollow cylindrical n-HA/PA66 cage is a satisfactory reconstructing implant after ACDF. Hu et al. [9] further analyzed the long-term follow-up (> 7 years) results of hollow cylindrical n-HA/PA66 cages used in single-level ACDF in comparison to PEEK cages. Although there were similar radiological and clinical outcomes with the hollow cylindrical n-HA/PA66 cage as the PEEK cage, the subsidence rates of the hollow cylindrical n-HA/PA66 cage were relatively high (10.6%). The authors speculated that the main reason may be that the shape of the hollow cylindrical n-HA/PA66 cage was less suitable than that of the PEEK cage, which had an impact on the biomechanical properties of the cage.
Sequentially, to reduce the subsidence rate, the hollow cylindrical n-HA/PA66 cage was redesigned into a horseshoe-shaped cage with a more suitable shape and larger bone graft volume (novel n-HA/PA66 cage). In this study, 52 patients with novel n-HA/PA66 cages (Group A) and 55 patients with hollow cylindrical n-HA/PA66 cages (Group B) were included. The 6-month postoperative IHs in both groups were comparable and significantly improved after the surgery. However, the IH at the final follow-up of Group A was significantly higher than that of Group B (36.7 mm vs. 35.9 mm, p < 0.05). Meanwhile, the subsidence rate at the final follow-up of Group A was 5.8% (3/52), which was significantly lower than that of Group B (18.2%, 10/55). These results indicated that the modifications to the morphology of the hollow cylindrical n-HA/PA66 cage were effective in lowering the subsidence rate.
Subsidence is associated with multiple factors, such as bone mineral density, smoking, operative segments, and cage characteristics (material, shape, height, etc.) [9, 21]. In the present study, the patient demographic data (age, sex, operative time, blood loss, and segments) of Groups A and B were similar, while the primary difference between the two groups was cage shape. Different cage shapes correlated with different cage-endplate interfaces and bone graft shapes and volumes and finally led to variational postoperative fusion and subsidence resistance [14, 22]. Compared to the hollow cylindrical n-HA/PA66 cage, the novel n-HA/PA66 cage’s horseshoe shape has more inverse distributed jags, which can better mimic the concave contour of the vertebral endplate and improve the contact area and anchorage. Interestingly, the bone graft volume of the novel n-HA/PA66 cage was higher than that of the hollow cylindrical n-HA/PA66 cage, but the fusion rates at 6 months postoperatively and at the final follow-up in both groups were comparable.
Postoperative complications such as cervical kyphosis, recurrence of neurological symptoms, and internal fixation failure may be related to cage subsidence because it can compromise IH and neural foramen stenosis [9, 10]. Fortunately, no patients in either group complained about subsidence-related symptoms during the follow-up. Furthermore, the JOA and VAS scores in Groups A and B were similar; they improved postoperatively and were maintained at the final follow-up. These findings could explain the comparably ideal patient satisfaction at the final follow-up in both groups.
There were several limitations in the present study. First, this was a retrospective study with a small sample size. Second, this study did not analyze patients with multiple CDDD. Hence, future prospective studies with more patients with multiple CDDD are required to investigate the outcomes when using novel n-HA/PA66 cages.
Conclusions
The novel n-HA/PA66 cage achieved favorable SA, C2-7a, fusion rate, and clinical outcomes, which were similar to those of the hollow cylindrical n-HA/PA66 cage in patients with CDDD who underwent single-level ACDF during a 7-year follow-up. At the final follow-up, the patients with novel n-HA/PA66 cages had a lower subsidence rate and higher IH than the patients with hollow cylindrical n-HA/PA66 cages.
Availability of data and materials
Data will be available upon request to the corresponding author.
Abbreviations
- n-HA:
-
Nanohydroxyapatite
- PA:
-
Polyamide
- ACDF:
-
Anterior cervical discectomy and fusion
- CDDD:
-
Cervical degenerative disk disease
- IH:
-
Intervertebral height
- C2-7a:
-
C2-7 angle
- SA:
-
Segmental alignment
- VAS:
-
Visual analog scale
- JOA:
-
Japanese Orthopedic Association
- PEEK:
-
Polyetheretherketone
- 3d-CT:
-
Three-dimensional CT
- TLIF:
-
Transforaminal lumbar interbody fusion
- ACCF:
-
Anterior cervical corpectomy and fusion
References
Baucher G, Taskovic J, Troude L, Molliqaj G, Nouri A, Tessitore E. Risk factors for the development of degenerative cervical myelopathy: a review of the literature. Neurosurg Rev. 2022;45(2):1675–89.
Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. Clin Spine Surg. 2015;28(5):136–40.
Schuermans VNE, Smeets A, Boselie AFM, Zarrouk O, Hermans SMM, Droeghaag R, Curfs I, Evers S, van Santbrink H. Cost-effectiveness of anterior surgical decompression surgery for cervical degenerative disk disease: a systematic review of economic evaluations. Eur Spine J. 2022;31(5):1206–18.
Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. JBJS. 1958;40(3):293–5.
Zhu C, Yang X, Wang L, Hu BW, Liu LM, Wang LN, Liu H, Song YM. Comparison of dynamic cervical implant versus anterior cervical discectomy and fusion for the treatment of single-level cervical degenerative disc disease: a five-year follow-up. Clin Neurol Neurosurg. 2018;164:103–7.
Chong E, Pelletier MH, Mobbs RJ, Walsh WR. The design evolution of interbody cages in anterior cervical discectomy and fusion: a systematic review. BMC Musculoskelet Disord. 2015;16:99.
Park PJ, Lehman RA. Optimizing the spinal interbody implant: current advances in material modification and surface treatment technologies. Curr Rev Musculoskelet Med. 2020;13(6):688–95.
Buck E, Li H, Cerruti M. Surface modification strategies to improve the osseointegration of poly(etheretherketone) and its composites. Macromol Biosci. 2020;20(2):e1900271.
Hu B, Yang X, Hu Y, Lyu Q, Liu L, Zhu C, Zhou C, Song Y. The n-HA/PA66 cage versus the PEEK cage in anterior cervical fusion with single-level discectomy during 7 years of follow-up. World Neurosurg. 2019;123:e678–84.
Zhong W, Liang X, Tang K, Luo X, Quan Z, Jiang D. Nanohydroxyapatite/polyamide 66 strut subsidence after one-level corpectomy: underlying mechanism and effect on cervical neurological function. Sci Rep. 2018;8(1):12098.
Wang X, Li Y, Wei J, de Groot K. Development of biomimetic nano-hydroxyapatite/poly(hexamethylene adipamide) composites. Biomaterials. 2002;23(24):4787–91.
Yang X, Liu L, Song Y, Kong Q, Zeng J, Tu C. Outcome of single level anterior cervical discectomy and fusion using nano-hydroxyapatite/polyamide-66 cage. Indian J Orthop. 2014;48(2):152–7.
Chen G, Yin M, Liu W, Xin B, Bai G, Wang J, Wang J, Gao X, Wang Y, Liu C, et al. A novel height-adjustable nano-hydroxyapatite/polyamide-66 vertebral body for reconstruction of thoracolumbar structural stability after spinal tumor resection. World Neurosurg. 2019;122:e206–14.
Wang J, Qian Z, Ren L. Biomechanical comparison of optimal shapes for the cervical intervertebral fusion cage for C5–C6 cervical fusion using the anterior cervical plate and cage (ACPC) fixation system: a finite element analysis. Med Sci Monit Int Med J Exp Clin Res. 2019;25:8379–88.
Zhang Y, Quan Z, Zhao Z, Luo X, Tang K, Li J, Zhou X, Jiang D. Evaluation of anterior cervical reconstruction with titanium mesh cages versus nano-hydroxyapatite/polyamide66 cages after 1- or 2-level corpectomy for multilevel cervical spondylotic myelopathy: a retrospective study of 117 patients. PLoS ONE. 2014;9(5):e96265.
Zhu C, He M, Mao L, Li T, Zhang L, Liu L, Feng G, Song Y. Titanium-interlayer mediated hydroxyapatite coating on polyetheretherketone: a prospective study in patients with single-level cervical degenerative disc disease. J Transl Med. 2021;19(1):14.
Brantigan JW, Steffee AD. A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine. 1993;18(14):2106–7.
Cámara-Torres M, Sinha R, Sanchez A, Habibovic P, Patelli A, Mota C, Moroni L. Effect of high content nanohydroxyapatite composite scaffolds prepared via melt extrusion additive manufacturing on the osteogenic differentiation of human mesenchymal stromal cells. Biomater Adv. 2022;137:212833.
Yan J, Nie L, Li G, Zhu Y, Gao M, Wu R, Wang B. Axial crystal growth evolution and crystallization characteristics of bi-continuous polyamide 66 membranes prepared via the cold non-solvent-induced phase separation technique. Polymers. 2022;14(9):1706.
Wang H, Li Y, Zuo Y, Li J, Ma S, Cheng L. Biocompatibility and osteogenesis of biomimetic nano-hydroxyapatite/polyamide composite scaffolds for bone tissue engineering. Biomaterials. 2007;28(22):3338–48.
Alan N, Vodovotz L, Muthiah N, Deng H, Guha D, Agarwal N, Ozpinar A, Mushlin HM, Puccio L, Hamilton DK, et al. Subsidence after lateral lumbar interbody fusion using a 3D-printed porous titanium interbody cage: single-institution case series. J Neurosurg Spine. 2022;1:1–7.
Manickam PS, Roy S, Shetty GM. Biomechanical evaluation of a novel s-type, dynamic zero-profile cage design for anterior cervical discectomy and fusion with variations in bone graft shape: a finite element analysis. World Neurosurg. 2021;154:e199–214.
Acknowledgements
Not applicable.
Funding
This work was supported by National Natural Science Foundation of China [81871772 & 82172495 & 82072386]; the Key Research and Development Project of Science & Technology Department of Sichuan Province [2022ZDZX0029 & 2022YFS0260 & 2021YFG0240]; and 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University [2021HXFH003 & ZYGD21001]. The organization had no involvements in the study design, collection, analysis, or interpretation of data, in the writing of the manuscript, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
ZZ and CZ conceptualized and designed the study, drafted the initial manuscript. ZD carried out the initial analyses, reviewed and revised the manuscript. LL and YS coordinated and supervised data collection, critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of West China Hospital of Sichuan University, and informed consent was obtained from the patients.
Consent for publication
The patients gave written consent for publication of their clinical details and clinical images. A copy of the written consent is available for review by the editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zeng, Z., Zhu, C., Deng, Z. et al. A novel nanohydroxyapatite/polyamide-66 cage for reducing the subsidence rate after single-level anterior cervical discectomy and fusion: a comparative study of 7-year follow-up. J Orthop Surg Res 18, 54 (2023). https://doi.org/10.1186/s13018-023-03521-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03521-1