Abstract
Background
Management of recalcitrant diabetic foot ulcers remains challenging. Tibial transverse transport (TTT) is an effective method for enhancing the healing of foot ulcers. This retrospective study reports a novel triplanar osteotomy in the tibia and assesses the clinical outcomes of TTT for diabetic foot ulcers.
Methods
Fifty-nine patients with recalcitrant diabetic foot ulcers were divided into the TTT (32 patients) and control (27 patients) groups. In the TTT group, the patients underwent triplanar osteotomy of the proximal tibia, followed by 2 weeks of medial distraction and 2 weeks of lateral distraction. In the control group, the patients received conventional management, including debridement, revascularization, and reconstruction. Ulcer healing and healing time, amputation, recurrence, and complications were assessed at an 18-month follow-up visit. Computed tomography angiography (CTA) was used to evaluate vessel changes in the lower limbs of patients in the TTT group.
Results
The TTT group was superior to the control group in the healing rate (90.6% [29/32] vs. 66.7% [18/27]) and the healing time (4.6 ± 1.7 months vs. 7.4 ± 2.5 months), respectively. The proportions of amputation and recurrence in the TTT group were lower than that in the control group, without statistical difference. After triplanar osteotomy and transverse distraction, CTA demonstrated an increase in small vessels in the wound and ipsilateral limb. All patients achieved satisfactory union of the osteotomized bone fragment after removal of the external fixator.
Conclusions
Triplanar osteotomy combined with proximal tibial transverse distraction accelerates wound healing and limb salvage caused by severe and recalcitrant diabetic foot ulcers. Triplanar osteotomy not only increases the bone contact area, which is beneficial for rapid bone reconstruction, but also preserves the vascularization of the bone fragment and substantially facilitates capillary angiogenesis during distraction. These results suggest that triplanar osteotomy followed by tibial transverse distraction is an effective method for treating diabetic foot ulcers.
Similar content being viewed by others
Background
Foot ulcerations are a severe, chronic diabetic complication of the lower limbs, with a global prevalence of 6.3% [1]. As the leading cause of infection, amputation, and hospitalization in patients with diabetes mellitus, foot ulcerations are a growing health concern. Diabetic foot ulcers in patients with peripheral neuropathy commonly result from repetitive high pressure over an area that has been subjected to high vertical or shear stress [2]. Peripheral vascular diseases also lead to limb ischemia and foot ulcers [3].
Foot ulcers can heal in patients undergoing appropriate management, including surgical debridement, off-loading of pressure, osteotomies, tendon-balancing interventions, reconstruction with flaps or skin grafting, and revascularization [2, 4,5,6]. However, recurrence is nearly 60% within 3 years after healing [7]. The management options mentioned above do not resolve profound skin microcirculation, muscle metabolism, and concomitant neuropathy, which can be triggered by repetitive stress, leading to inflammation and ulceration [8, 9]. Therefore, the treatment of recalcitrant diabetic foot ulcers remains a challenge for orthopedic surgeons.
Based on the law of tension stress, distraction osteogenesis promotes neovascularization and microcirculation in bone and surrounding soft tissue, leading to increased and prolonged perfusion to the distal tissue of the limb [10,11,12,13]. Tibial transverse transport (TTT) was introduced as a novel technique to treat local ischemic diseases, which involves corticotomy in the proximal tibia followed by medial-then-lateral distraction to accelerate the healing of foot ulcers [10, 14, 15]. The effect of TTT is due to neovascularization and neurogenesis during wound healing, which results in continuous perfusion and scarless tissue formation, with improved tactile sensation in the foot [14, 16]. In this study, we developed a triplanar osteotomy in the proximal tibia followed by TTT to preserve vascularization of the bone fragment and substantially facilitate capillary angiogenesis for ulcer healing.
Patients and methods
Patients
The study was approved by the ethics committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. All participants provided informed consent prior to participating in the study. We retrospectively reviewed 59 consecutive patients with chronic diabetic foot ulcers who reported to our hospital from May 2015 to March 2019. Inclusion criteria were patients with diagnosis of diabetes mellitus based on the American Diabetes Association criteria [17], over 18 years of age, with non-healing or recurrent foot ulcers for at least 6 months, and with ulcers classified as Grade 2-B to 3-D (wound penetrating the tendon, capsule, bone, or joint with infection and/or ischemia) based on the University of Texas wound classification system [18]. Exclusion criteria included non-diabetic foot ulcers, ulcers above the ankle joint, local signs of infection that presented as cellulitis or suppuration in the surgical area of the calf [14], history of life-threatening diseases (such as cerebral infarction, myocardial infarction, heart failure, or cancer) within the last 3 months, use of current drugs (cortical steroids, immunosuppressive drugs, or chemotherapy treatment) that affected bone metabolism, poor compliance to follow-up, and death before the end of the 18-month follow-up study period.
Fifty-nine patients were divided into 2 groups: 32 patients assigned to the TTT group underwent triplanar osteotomy and TTT, while 27 patients assigned to the control group underwent negative pressure therapy followed by split-thickness skin grafting or flap reconstruction. All procedures were performed by XZ and GW. There were no significant differences in sex, age, body mass index (BMI), duration of diabetes mellitus, duration of foot ulcers, ulcer area, or grade of foot ulcers assessed by the University of Texas wound classification system between the 2 groups. Demographic data are shown in Table 1.
For all patients, wound cultures were performed to identify the causative organisms and their antibiotic sensitivities, which were the basis for prescribing oral or intravenous antibiotics according to the Infectious Diseases Society of America guidelines [19, 20]. The probe-to-bone test and plain radiographs were used to diagnose chronic osteomyelitis in infected wounds [21, 22]. The ankle brachial index accompanied by palpation of the dorsalis pedis and posterior tibial arteries was used to screen for peripheral arterial disease of the lower limb [23]. Computed tomography angiography (CTA) and color Doppler ultrasonography were performed to evaluate vascular status. Further assessment and revascularization were necessary, if there was atherosclerotic evidence of obstruction and occlusion. Semmes–Weinstein monofilaments were used to identify peripheral sensory neuropathy in patients with foot ulcers [24].
Surgical techniques
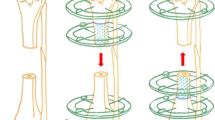
Patients underwent TTT surgery under general anesthesia in supine position on a radiolucent operating table. Two curved skin incisions, 3 cm in length and 1 cm medial to the tibial crest, were made. The proximal incision was approximately 2 cm distal to the tibial tuberosity, while the distal incision was approximately 6 cm distal to the tibial tuberosity. The periosteum was exposed and carefully preserved after retraction of the subcutaneous soft tissue. A triplanar osteotomy (6.5 cm in height and 1.5 cm in width) was created on the medial cortex of the proximal tibia after drilling multiple holes along the 3 sides (proximal, distal, and lateral) of the rectangle; the medial margin of the tibia was used as the medial side of the rectangle, and the cortex located on the posterior tibia was lightly removed. After pre-drilling with the director, 2 half-pins (diameter, 4.0 mm) were inserted into the osteotomized bone fragment perpendicular to the transverse transport, and another 2 half-pins (diameter, 5.0 mm) were implanted proximally and distally into the tibia to stabilize the external fixator. The position of the half-pins and osteotomy site were confirmed using an image intensifier. The modular components were then assembled to form a stable apparatus for distraction. Approximately, 2.0 cm was maintained between the external fixation and skin.
For diabetic foot ulcers, thorough debridement was performed in all patients. The ulcer area was assessed by measuring the maximum length and width. In the TTT group, the debridement was performed after assembling the external fixators and closing the incisions, and the wounds were left open. In the control group, more than one debridement with negative pressure therapy was necessary, and split-thickness skin grafting or local/free flap coverage can be performed only after the wound bed is prepared (Fig. 1).
The surgical procedure of triplanar osteotomy and transverse distraction. A A triplanar osteotomy (6.5 cm in height with a width of 1.5 cm) was created on the medial cortex of the proximal tibia along the 3 sides (proximal, distal, and lateral) of the rectangle; the medial margin of the tibia was used as the medial side of the rectangle. B–D 2 curved skin incisions were made. The external fixator was assembled after triplanar osteotomy and insertion of half pins
Postoperative care
Gauze was used to cover the pin site and was changed every 5 to 7 days in the TTT group, while wound dressing changes were applied daily to patients in both groups, keeping the wound dry. Mobilization, including physiotherapy, with active and passive range of motion exercises for the hip, knee, and ankle started on the first postoperative day. Patients in the TTT group were encouraged to start early partial weight-bearing with crutches. For those undergoing gradual transport, medial distraction started on the eighth postoperative day at a rate of 1 mm per day (0.25 mm every 6 h). After 14 days of medial distraction, 14 days of lateral distraction was performed at the same rate. Radiographs were obtained biweekly to monitor the extent of distraction and position of the transported bone fragment. Two weeks after the distraction, the external fixator was removed in the outpatient clinic. CTA was performed 1 month after removal of the external fixator to assess vascular status after transverse transport.
All patients reported to the hospital for follow-up every 2 weeks during the first 3 months postoperatively and subsequently at 1–3 months intervals until the final 18-month follow-up evaluation. Home-based care strategies, including glycemic control, foot skin temperature monitoring, and off-load footwear after ulcer healing, were recommended to prevent foot ulcer recurrence. Ulcer status and related complications were assessed and recorded for both groups.
Statistical analysis
The results of this study are expressed as mean ± standard deviation. Student’s t test was used for continuous variables, while the chi-square test or Fisher’s exact test was used for categorical variables to assess statistical differences. The counting data were compared using the nonparametric Kruskal–Wallis H-test. Statistical significance was set at P < 0.05. All analyses were performed using SPSS software (version 25.0; IBM Corporation, Armonk, NY, USA).
Results
The ulcer healing rate at the 18-month follow-up was significantly higher in the TTT group (90.6%, 29/32) than in the control group (66.7%, 18/27). The recorded healing time revealed a significant difference between the 2 groups (p = 0.02). The healing time was 4.6 ± 1.7 months in the TTT group, which was substantially shorter than that in the control group (7.4 ± 2.5 months) (P < 0.001). A lower proportion of patients in the TTT group (6.3%, 2/32) underwent major amputation compared to that in the control group (18.5%, 5/27), without statistical difference. In the TTT group, 2 patients underwent major amputations due to massive thromboses in the popliteal, tibial anterior, and tibial posterior arteries. In the control group, 3 patients showed persistent and severe ulceration, 2 patients exhibited pain that caused disability and underwent major amputations. All amputations were performed below the knee joint, and the residual limb wound healed smoothly in these patients. The recurrence rate was 3.1% (1/32) in the TTT group and 14.8% (4/27) in the control group; however, there was no significant difference between the 2 groups. Three patients with persistent recurrent ulcers in the control group underwent major amputations; other recurrent ulcers in the 2 groups received daily wound dressing changes, and the ulcers healed. More small vessels were found in the wound and ipsilateral limb when CTA was performed (Fig. 2).
A 68-year-old man suffered from recalcitrant diabetic foot ulcer for 2 years. A Ischemic and necrotic toes and soft tissues at distal foot preoperatively. B Preoperative CTA image showed small vessels of the affected calf and foot were damaged. C, D The necrotic tissues were removed after debridement. E, F The triplanar osteotomy and external fixator sites were confirmed on radiographs postoperatively. G, H After medial distraction, the bone fragment is transported medially. I the image showed the affected foot during distraction. J The bone fragment was completely united 4 weeks after removal of the external fixator. K The ulcer was completely healed at 10 weeks postoperatively. L Postoperative CTA image showed more small vessels were present in the affected limb
To avoid fracture at the osteotomy site, the external apparatus was removed 2 weeks after distraction when the preliminary callus could be visualized. We reduced the frequency of dressing changes to maintain compression and dryness around the pin site. No pin tract infection occurred, and satisfactory union of the osteotomized bone fragment was achieved in all the patients (Fig. 2).
Discussion
Tibial transverse transport with corticotomy in the proximal tibia is an emerging new surgical technique for the treatment of severe chronic limb ischemic diseases such as diabetic foot ulcers. During distraction, neovascularization and increased perfusion in the ulcerated foot accelerate healing, limb salvage, and decrease ulcer recurrence [14]. In this study, we developed a novel triplanar osteotomy in the proximal tibia, followed by tibial transverse transport, for the management of recalcitrant diabetic foot ulcers. Compared to conventional surgical therapy, triplanar osteotomy combined with TTT exhibited a higher rate of ulcer healing and a lower rate of amputation and recurrence at 18-month follow-up.
Due to the hyperglycemic status of patients with diabetes, the pathophysiology of foot ulcers is characterized by neuropathic, vascular, and immune system disorders [25]. Oxidative stress in nerve cells and glycosylation of nerve cell proteins lead to neuropathy and further ischemia [26]. Moreover, endothelial cell dysfunction occurs after from hyperglycemia-induced changes in the peripheral arteries, leading to reduced vasodilation and increased vasocontraction [26, 27]. Additionally, immune function changes, including decreased healing response and increased apoptosis of immune response cells, are observed in patients with diabetic foot ulcers [27]. Thus, the treatment of diabetic foot ulcers should focus on not only angiogenesis and neurogenesis caused by surgical techniques, but also self-management, including glycemic control, home monitoring, and appropriate foot care. However, most conventional surgical therapies emphasize peripheral percutaneous angioplasty and wound healing of foot ulcers, contributing to a high rate of recurrence, amputation, and even death [18, 28].
Our study demonstrated that after treatment with TTT, there was neovascularization and increased microcirculation in the diabetic foot, which is consistent with outcomes observed in animal studies [16, 29]. Yang et al. [16] reported that increased endothelial progenitor cells were found in the wound following TTT management, confirming that transverse transport is beneficial for angiogenesis in the foot. Meanwhile, immunomodulatory responses have been found to play an active role after TTT treatment, especially in the late stage of ulcer healing. M1 and M2 macrophages are the most prominent cells in the inflammation and proliferation phases of tissue repair [30, 31]. M1 macrophages are remarkably promoted to M2 by TTT, indicating a switch from inflammation to the proliferation phase of wound healing [32]. M2 macrophages release vascular endothelial growth factors to promote blood vessel formation and guide axonal regeneration [33]. Therefore, angiogenesis and neurogenesis mutually contribute to the resolution of inflammation and initiation of healing [34]. Additionally, the TTT procedure can also induce positive systemic responses by mobilizing bone marrow-derived endothelial progenitor cells and mesenchymal stem cells to the ulcer area to promote histogenesis [35].
In comparison to the TTT technique reported by Chen et al., it is worth noting that a 6.5-cm by 1.5-cm triplanar osteotomy instead of a 5-cm by 1.5-cm corticotomy was performed in our study [14]. To preserve and accelerate perfusion of the transported bone fragment as much as possible, and to increase the bone contact area after distraction, the medial margin of the tibia, rather than a vertical rectangle osteotomized in the center of the proximal medial tibia, was used as the base of the rectangle. In a recent study by Grüneboom et al., hundreds of capillaries, referred to as trans-cortical vessels (TCVs), were verified to originate in the bone marrow, cross-cortical bone perpendicular to the shaft and connect to the periosteal circulation in human limb bone [36]. Furthermore, TCVs can mediate the recruitment of immune cells from the bone marrow to the circulation for host defense against inflammation [36, 37]. Hence, for minimally invasive incision and intact periosteum retention, triplanar osteotomy combined with transverse transport could induce the TCV system in the cortices to facilitate neovascularization and immunomodulation. In addition, according to the hypothesis of ‘open window’ [15], triplanar osteotomy of the proximal tibia could also contribute to relieving bone marrow pressure, decreasing vasocontraction, and consequently improving microcirculation to foot ulcers.
The skin is normally juvenile immediately after an ulcer has healed, which is the period when patients think they no longer have a foot problem. Consequently, patients may not pay attention to follow-up podiatric care and warning signs of recurrence [38]. In accordance with Armstrong et al., we encouraged patients in this study to ensure glycemic control, ongoing podiatric care at intervals of 1–3 months, appropriate-fitting footwear to relieve plantar pressure, and home-based foot care, including monitoring of pedal skin temperature and other inflammatory signs to prevent ulcer recurrence [7].
This study has several limitations. It was a retrospective, nonrandomized study. Therefore, selection bias could have occurred. However, the patients in both groups were consecutively recruited by different surgeons using the same criteria, and these patients will continue to be observed to assess long-term outcomes. Additionally, the number of patients was small and heterogeneous. Further studies in larger populations are necessary to confirm the benefits of this unique therapy.
In conclusion, our results indicate that proximal TTT is a useful treatment option for recalcitrant diabetic foot ulcers. Triplanar osteotomy not only increases the bone contact area after transport, which is beneficial for rapid bone healing, but also preserves the vascularization of the bone fragment and substantially facilitates capillary angiogenesis during distraction. Such innovative therapy during the active phase of diabetic foot ulcers combined with a focus on improving care after healing of the ulcer can result in improved quality of life.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Change history
17 November 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1186/s13018-023-04351-x
Abbreviations
- TTT:
-
Tibial transverse transport
- BMI:
-
Body mass index
- CTA:
-
Computed tomography angiography
- TCVs:
-
Trans-cortical vessels
References
Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis (dagger). Ann Med. 2017;49:106–16.
Bus SA, van Deursen RW, Armstrong DG, Lewis JE, Caravaggi CF, Cavanagh PR, et al. Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: a systematic review. Diabetes Metab Res Rev. 2016;32(Suppl 1):99–118.
Monteiro-Soares M, Boyko EJ, Ribeiro J, Ribeiro I, Dinis-Ribeiro M. Predictive factors for diabetic foot ulceration: a systematic review. Diabetes Metab Res Rev. 2012;28:574–600.
Biz C, Ruggieri P. Minimally invasive surgery: osteotomies for diabetic foot disease. Foot Ankle Clin. 2020;25:441–60.
Suh HS, Oh TS, Hong JP. Innovations in diabetic foot reconstruction using supermicrosurgery. Diabetes Metab Res Rev. 2016;32(Suppl 1):275–80.
Hinchliffe RJ, Brownrigg JR, Andros G, Apelqvist J, Boyko EJ, Fitridge R, et al. Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Diabetes Metab Res Rev. 2016;32(Suppl 1):136–44.
Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376:2367–75.
Greenman RL, Panasyuk S, Wang X, Lyons TE, Dinh T, Longoria L, et al. Early changes in the skin microcirculation and muscle metabolism of the diabetic foot. Lancet. 2005;366:1711–7.
Boulton AJ, Kirsner RS, Vileikyte L. Clinical practice. Neuropathic diabetic foot ulcers. N Engl J Med. 2004;351:48–55.
Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989:249–81.
Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990:8–26.
Ohashi S, Ohnishi I, Kageyama T, Imai K, Nakamura K. Distraction osteogenesis promotes angiogenesis in the surrounding muscles. Clin Orthop Relat Res. 2007;454:223–9.
Aronson J. Temporal and spatial increases in blood flow during distraction osteogenesis. Clin Orthop Relat Res. 1994. https://doi.org/10.1097/00003086-199404000-00020.
Chen Y, Kuang X, Zhou J, Zhen P, Zeng Z, Lin Z, et al. Proximal tibial cortex transverse distraction facilitating healing and limb salvage in severe and recalcitrant diabetic foot ulcers. Clin Orthop Relat Res. 2020;478:836–51.
Nie X, Kuang X, Liu G, Zhong Z, Ding Y, Yu J, et al. Tibial cortex transverse transport facilitating healing in patients with recalcitrant non-diabetic leg ulcers. J Orthop Translat. 2021;27:1–7.
Yang Y, Li Y, Pan Q, Bai S, Wang H, Pan XH, et al. Tibial cortex transverse transport accelerates wound healing via enhanced angiogenesis and immunomodulation. Bone Joint Res. 2022;11:189–99.
American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40:S11–S24.
Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care. 1998;21:855–9.
Ahluwalia R, Lázaro-Martínez JL, Reichert I, Maffulli N. Advances in pharmacotherapy for diabetic foot osteomyelitis. Expert Opin Pharmacother. 2021;22:2281–91.
Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJG, Armstrong DG, et al. 2012 Infectious diseases society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54:e132–73.
Morales Lozano R, Gonzalez Fernandez ML, Martinez Hernandez D, Beneit Montesinos JV, Guisado Jimenez S, Gonzalez Jurado MA. Validating the probe-to-bone test and other tests for diagnosing chronic osteomyelitis in the diabetic foot. Diabetes Care. 2010;33:2140–5.
Aicale R, Cipollaro L, Esposito S, Maffulli N. An evidence based narrative review on treatment of diabetic foot osteomyelitis. Surgeon. 2020;18:311–20.
Potier L, Abi Khalil C, Mohammedi K, Roussel R. Use and utility of ankle brachial index in patients with diabetes. Eur J Vasc Endovasc Surg. 2011;41:110–6.
Kumar S, Fernando DJ, Veves A, Knowles EA, Young MJ, Boulton AJ. Semmes-Weinstein monofilaments: a simple, effective and inexpensive screening device for identifying diabetic patients at risk of foot ulceration. Diabetes Res Clin Pract. 1991;13:63–7.
Wolf G. New insights into the pathophysiology of diabetic nephropathy: from haemodynamics to molecular pathology. Eur J Clin Invest. 2004;34:785–96.
Noor S, Zubair M, Ahmad J. Diabetic foot ulcer–a review on pathophysiology, classification and microbial etiology. Diabetes Metab Syndr. 2015;9:192–9.
Paraskevas KI, Baker DM, Pompella A, Mikhailidis DP. Does diabetes mellitus play a role in restenosis and patency rates following lower extremity peripheral arterial revascularization? A critical overview. Ann Vasc Surg. 2008;22:481–91.
Giurato L, Vainieri E, Meloni M, Izzo V, Ruotolo V, Fabiano S, et al. Limb salvage in patients with diabetes is not a temporary solution but a life-changing procedure. Diabetes Care. 2015;38:e156–7.
Matsuyama J, Ohnishi I, Kageyama T, Oshida H, Suwabe T, Nakamura K. Osteogenesis and angiogenesis in regenerating bone during transverse distraction: quantitative evaluation using a canine model. Clin Orthop Relat Res. 2005. https://doi.org/10.1097/01.blo.0000150562.24256.a4:243-50.
Atri C, Guerfali FZ, Laouini D. Role of human macrophage polarization in inflammation during infectious diseases. Int J Mol Sci. 2018. https://doi.org/10.3390/ijms19061801.
Gu Q, Yang H, Shi Q. Macrophages and bone inflammation. J Orthop Translat. 2017;10:86–93.
Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8:958–69.
Wu J, Xie H, Yao S, Liang Y. Macrophage and nerve interaction in endometriosis. J Neuroinflammation. 2017;14:53.
Porcheray F, Viaud S, Rimaniol AC, Leone C, Samah B, Dereuddre-Bosquet N, et al. Macrophage activation switching: an asset for the resolution of inflammation. Clin Exp Immunol. 2005;142:481–9.
Jin L, Deng Z, Zhang J, Yang C, Liu J, Han W, et al. Mesenchymal stem cells promote type 2 macrophage polarization to ameliorate the myocardial injury caused by diabetic cardiomyopathy. J Transl Med. 2019;17:251.
Gruneboom A, Hawwari I, Weidner D, Culemann S, Muller S, Henneberg S, et al. A network of trans-cortical capillaries as mainstay for blood circulation in long bones. Nat Metab. 2019;1:236–50.
Herisson F, Frodermann V, Courties G, Rohde D, Sun Y, Vandoorne K, et al. Direct vascular channels connect skull bone marrow and the brain surface enabling myeloid cell migration. Nat Neurosci. 2018;21:1209–17.
Bus SA, van Netten JJ, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, et al. IWGDF guidance on the prevention of foot ulcers in at-risk patients with diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):16–24.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from National Key Research and Development Program of China (No. 2020YFC2004900); Clinical Technology Innovation Project of Shanghai Hospital Development Center (Grant SHDC12019X06); Basic Research Project of Shanghai Sixth People's Hospital (General Cultivation Project, ynms202104).
Author information
Authors and Affiliations
Contributions
All authors contributed to the planning of the study. JX and SL wrote the article. JX, SL, YS, BB, TZ, QK, XZ, and GW conducted the study. JX, SL, and GW assisted in statistical analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, and all participants provided informed consent prior to participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail:https://doi.org/10.1186/s13018-023-04351-x
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, J., Li, S., Sun, Y. et al. RETRACTED ARTICLE: Triplanar osteotomy combined with proximal tibial transverse transport to accelerate healing of recalcitrant diabetic foot ulcers. J Orthop Surg Res 17, 528 (2022). https://doi.org/10.1186/s13018-022-03410-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03410-z