Abstract
Background
Femoral tunnel can be drilled through tibial tunnel (TT), or independent of it (TI) by out-in (OI) technique or by anteromedial (AM) technique. No consensus has been reached on which technique achieves more proper femoral aperture position because there have been evolving concepts in the ideal place for femoral aperture placement. This meta-analysis was performed to analyze the current literature comparing femoral aperture placement by TI versus TT techniques in ACL reconstruction.
Methods
We performed a comprehensive systematic review and meta-analysis of English-language literature in PubMed, Cochrane, and Web of Science databases for articles comparing femoral aperture placement by TI versus TT techniques with aperture position assessed by direct measurement or by postoperative imaging, PXR and/or CT and/or MRI.
Results
We included 55 articles with study population of 2401 knees of whom 1252 underwent TI and 1149 underwent TT techniques. The relevant baseline characteristics, whenever compared, were comparable between both groups. There was nonsignificant difference between TI and TT techniques in the distance from aperture center to footprint center and both techniques were unable to accurately recreate the anatomic footprint position. TI technique significantly placed aperture at more posterior position than TT technique. TI technique significantly lowered position of placed aperture perpendicular to Blumensaat’s line (BL) than TT technique, and modifications to TT technique had significant effect on this intervention effect. Regarding sagittal plane aperture placement along both AP anatomical axis and BL, there was nonsignificant difference between both techniques.
Conclusion
Modifications to TT technique could overcome limitations in aperture placement perpendicular to BL. The more anterior placement of femoral aperture by TT technique might be considered, to some extent, a proper position according to recent concept of functional anatomical ACL reconstruction.
Similar content being viewed by others
Introduction
Improper femoral aperture placement is the most common cause of anterior cruciate ligament (ACL) reconstruction failure or unsatisfactory outcomes [1]. The criteria of proper femoral aperture placement had changed overtime. First, surgeons aimed mainly to restore the anteroposterior stabilizing function of ACL by isometric positioning of femoral aperture creating vertical ACL graft [2]. With further anatomical and biomechanical studies, surgeons realized the two-bundle anatomy of the ACL and the specific role of its lower, more shallow fibers (posterolateral bundle) in its rotatory stabilizing function. Accordingly, surgeons attempted to restore the native femoral footprint by inserting ACL graft at the footprint center (average site of the ACL two bundle) “Anatomical single bundle ACL reconstruction” [2]. However, given that recent research demonstrated that the size, morphology, and site of this footprint are highly variable from person to person and that this footprint is usually absent especially in chronic ACL injury, there is no standard guidelines applicable to all individuals that tell the surgeon where to place the ACL femoral aperture and the ACL graft insertion site should be individualized [1]. Moreover, there has been a recent discussion over the past decade that divided ACL insertion into direct and indirect fibers. This recent concept of ACL anatomy may affect the determination of the ideal place for performing femoral aperture where the new ligament might be positioned within the ACL footprint in the most functional load bearing position where the direct fibers lie "Functional anatomical ACL reconstruction" [1].
The femoral tunnel can be drilled through the tibial tunnel (TT), or independent of it (TI) by the out-in (OI) technique or by the anteromedial transportal (AM) technique. In TT technique, the placement of the femoral tunnel is dependent on the tibial tunnel [3]. However, because the diameter of the endoscopic femoral offset guide aimer and the shaft of the acorn femoral reamer are smaller than the tibial tunnel diameter, there is reasonable corresponding degree of freedom to externally rotate the offset guide and place the femoral tunnel as low in the intercondylar notch as possible [4], whereas in TI techniques, the surgeon could choose freely where to place the femoral tunnel, regardless of the tibial tunnel. However, this does not ensure proper placement of femoral tunnel, as surgeon may choose inappropriate positions [3].
There are advantages and disadvantages to each technique. The TT technique is more familiar and allows an isometric position and easy graft passage. However, disadvantages include increased vertical and potentially nonanatomic tunnels, alongside posterior tibial tunnel placement. The advantages of AM technique include the anatomical positioning of the femoral tunnel and theoretically better rotational stability. However, this approach may increase the risks of iatrogenic damage to the medial femoral condylar cartilage and creating critically short tunnels. The OI technique has additional advantage of lower risk of posterior wall rupture. However, acute femoral tunnel angle and additional lateral skin incisions are major impediments [3].
Difference in femoral tunnel orientation between both techniques has been studied extensively in literature. However, femoral tunnel obliquity does not reflect graft obliquity exactly. Graft obliquity is affected primarily by intraarticular aperture location of the femoral and tibial tunnels [5].
The aim of this review is to evaluate femoral aperture positioning achieved by each technique and its relevance to the modern studies assessing the anatomical and biomechanical properties of ACL femoral insertion. In addition, we assessed the effect of each technique on the tibial aperture position.
Methods
Search methods
We performed a comprehensive literature search of the following databases from their inception dates to March 2021: PubMed, Cochrane Central Register of Controlled Trials [CENTRAL], and Web of Science. Searches were carried out in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) [6]. Before the literature search, the research protocol for this review was registered with the PROSPERO international prospective register of systematic reviews and published online under registration number CRD42019133505. The full search strategy is presented in Additional file 1. Three independent reviewers (M.M.A., M.R.A, and H.K.H.) conducted the search separately. We also searched the reference lists of the included studies for additional eligible articles.
Criteria for considering studies for this review
The eligibility criteria for studies were as follows: studies directly comparing TT versus TI (AM or OI) femoral drilling techniques for femoral aperture placement with aperture position assessed by direct measurement or by postoperative imaging: PXR and/or CT and/or MRI and quantified by an appropriate method. Studies should report aperture position by a suitable statistic describing average and distribution, and sample numbers. Abstracts, case reports, and conference presentations were excluded. Only articles in English were included.
The eligibility criteria for participants were as follows: Human or cadaveric subjects, following single bundle ACL reconstruction in skeletally mature individuals.
Data collection and analysis
Study selection
The selection of studies was performed by 2 independent investigators (M.M.A. and M.R.A) separately. Any disagreement was resolved by an arbiter (most senior, third author [H.K.H.]).
Data extraction and management
Data from included studies were independently extracted into spreadsheets by the 3 investigators. In case of any missing data in any study, we tried to contact the corresponding author.
Assessment of risk of bias
Two reviewers (M.M.A. and M.R.A) independently appraised each article. Any disagreement was resolved by the arbiter. The revised and validated version of the Methodological Index for Non-randomized Studies (MINORS) scoring system was used [7]. In brief, the MINORS scoring system provides a method to assess bias, with a higher score indicative of less bias. The optimum score for comparative studies is 24.
Statistical analysis
We provided a qualitative synthesis of the findings from the included studies, structured according to the imaging technique and measurement method. If enough comparative studies were provided (at least 2) using the same measurement tool on the same imaging modality, a meta-analysis was performed. When trials included multiarm interventions, we combined arms utilizing the same intervention. A fixed-effects meta-analysis was used for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect. If substantial statistical heterogeneity (I2 statistics > 75%) was detected, the possible clinical and methodological reasons for this were explored qualitatively and quantitatively, also a random-effect model was used for meta-analysis. To quantitatively explore heterogeneity, we performed subgroup analyses searching for potential effect modification. Assessed effect modifiers included the type of experimental intervention (AM vs OI tibial independent technique) and modifications to the comparison intervention (conventional vs modified TT technique). Sensitivity analyses was performed to assess the effect of including studies of low-quality design (observational studies). We restricted these to femoral aperture position perpendicular to BL. We performed these analyses using RevMan software (version 5.3.5; Nordic Cochrane Centre, Copenhagen, Denmark).
Results
Search results
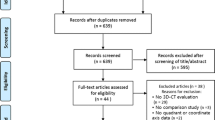
Details of study identification, inclusion, and exclusion are shown in Fig. 1 [8,9,10,11].
Study characteristics
Our review included 39 clinical studies [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50] and 16 basic science studies [51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]. The clinical studies included 21 retrospective cohort studies, 11 prospective cohort studies, and 7 randomized controlled trials (RCTs) [14, 24, 28, 36, 44, 48, 50]. (Three of them were registered, two [36, 50] prospectively in ClinicalTrials.gov and the third [24] retrospectively in Chinese Clinical Trial Registry.) From the 16 cadaveric studies, 6 were RCTs [53, 60,61,62,63,64] (2 of them quasi-randomized [53, 62]). Table in Additional file 2 summarizes the characteristics of included studies in this review, including number of knees assessed, imaging modality or its surrogate, and MINORS score for each study.
The design of all cadaveric studies was independent-measures design except 5 were conducted in a repeated-measures design [53, 54, 57, 58, 61]. The independent measures were on paired specimens in 6 studies [51, 55, 60, 62,63,64] (i.e., one knee of a cadaver pair was drilled with TT technique and the opposite knee was drilled with TI technique), on unpaired specimens in 4 studies [56, 59, 65, 66], and the pairing was unclear in one study [52].
Participants characteristics
Clinical studies
From a total of 2401 knees, 1252 underwent TI femoral tunnel drilling whereas 1149 received TT drilling. The mean age of participants undergoing TI and TT drilling procedure was 30.9 and 29 years, respectively. In the 20 studies, in which gender was reported and could be calculated, the percentage of male patients who had undergone TI and the TT drilling procedure was 77% and 87%, respectively. The time between injury and surgery, whenever reported in 11 studies, varied from less than 3 months in 4 studies [24, 32, 36, 48] and more than three months in seven studies [13, 15, 16, 23, 28, 45, 49]. However, whenever compared [24, 32, 36, 48, 49], there was nonsignificant difference between both groups.
Cadaveric studies
In all studies, the specimens were fresh not embalmed thus preserving bony and soft tissue anatomy. From a total of 428 placed apertures (in 328 knees), 232 were placed by TI technique whereas 196 were placed by TT technique. The weighted average age of specimens, in the 11 studies reporting a known age, was 66.6 years. In the 3 studies, reporting a known specimen’s gender, there were 54 males, 14 females, and 2 undetermined genders. In the 6 studies reporting about articular cartilage quality of specimens [52, 54, 56, 60, 61, 65], there were no significant, or even no, arthritis. ACL was intact in the 8 studies reporting about its integrity [52, 54,55,56,57,58, 60, 61]
Surgical techniques
Intervention integrity (the surgeon)
Thirty-five studies reported the number of surgeons which was same surgeon or surgical team in 22, two surgeons in 5, three or four surgeons in 5, eight to twenty-two surgeons in 3 studies. Most studies reported relevant information about surgeon's experience level like experience years or surgery volume or surgeon seniority. Qualitative inter-studies comparison showed that the surgeons had varying experience level. However, the type of the procedure chosen for each patient, in observational studies, was based on the preferred surgeon surgical technique.
Surgical technique of TT femoral tunnel drilling
From 47 studies reporting the intervention details, the TT technique included modifications in some of them. These modifications could be divided into (1) recreation of native coronal or sagittal ACL orientation by alteration of tibial tunnel extra-articular starting point in mediolateral (ML) or proximal-distal (PD) direction [67, 68], which was performed in 21 and 3 studies, respectively. (2) Alteration of position of tibial in relation to femur during femoral aperture placement. (3) AM portal-assisted TT femoral tunnel drilling. (4) Posterior "over the top" notchplasty (allowing increased offset guide rotation). (5) Intentional tibial aperture posterolateral beveling. As the first modification of altering tibial tunnel starting point is an old modification and was performed in nearly two-third (24/36) of studies reporting tibial tunnel starting point, in our review, modified technique (mTT) would denote only the other 4 modifications. So, there were 11 studies utilized mTT technique [14, 28, 32, 33, 47, 48, 50, 52, 57, 63, 64]. (Details of modifications in these studies are presented in table in Additional file 3).
The intraarticular target point for the tibial tunnel, whenever reported in 41 studies, had been aimed at the tibial footprint. However, it had been aimed at the anteromedial and posterolateral part of the footprint in 11 and 6 studies, respectively. From the 25 studies reporting tibial tunnel diameter, it was 8 mm, 9–10 mm, and 10–11 mm in 9, 4, and 12 studies, respectively. From the 47 studies reporting femoral aperture localization strategy, an offset femoral guide was utilized in 38 and was not utilized in 9 studies. Moreover, other utilized methods varied in different studies. (Details of localization strategies utilized in TT technique in included studies are presented in first table in Additional file 4).
Surgical technique of TI femoral tunnel drilling
Independent drilling of femoral tunnel was performed by AM technique in 37 studies or by OI technique in 10 studies. The TI technique was undetermined in one study [29]. In addition, in 7 three-arm studies, the independent drilling was performed by AM and OI techniques. From the 53 studies reporting femoral aperture localization strategy, the remnant ACL footprint was reported to be visualized in 18 studies. Also, the other utilized methods varied in different studies (Details of localization strategies utilized in TI technique in included studies are presented in second table in Additional file 4).
AM femoral tunnel drilling technique
From the 40 studies reporting intervention details of AM technique (total 44 studies), femoral tunnel was drilled through the single AM portal (two-portal technique) in 19 studies, through an accessory AM portal (three-portal technique) in 12 studies, and through either of them (in each of two subgroups) in one study [26]. The working AM portal was unclear in 6 studies [25, 38, 49, 50, 54, 61]. In 2 studies [56, 62], the femoral tunnel was drilled through medial parapatellar approach (open approach).
OI femoral tunnel drilling technique
From the 16 studies reporting intervention details of OI technique (total 17 studies), femoral tunnel was drilled by rear-entry guide in 3 studies [13, 15, 56] and front-entry guide in 13 studies.
Quality assessment of included studies
From 47 studies reporting about conflicts of interest (COI), 18 studies had potential COI. Six studies judged to be of notable concern as they were funded by private company who could gain from the study results, e.g., manufacturer [12, 35, 50, 57, 58, 60].
The MINORS scoring system deemed studies as acceptable quality with low bias (Additional file 2). The mean MINORS score for all included studies was (965 points/55 studies) = 18.2 points {76% of total possible points; range, (62.5–100%)}.
Follow-up duration was defined as the time interval between surgery and timing of femoral aperture position assessment, with a shorter time interval (less than 3 to 6 months) associated with a lower risk of bias, due to tunnel widening being unlikely. From the 28 clinical studies reporting the follow-up period, femoral aperture was assessed within one month in 15 studies. In the remaining 12 studies the average follow-up duration was 13 months.
While the age, and its associated degenerative changes, could affect the anatomy of the footprint and even the notch, the gender could affect only assessment tools that quantify F aperture position by measuring distance in millimeter (mm) from anatomical landmark. In clinical studies, the age and gender, whenever compared in 27 clinical studies, were comparable between the 2 groups. In cadaveric studies, while independent-measures design, with measures performed on paired specimens, eliminated among-individuals variations (e.g., age, gender, OA) except side-to-side variation within the same individual, the repeated-measures design eliminated all among-participants variations. However, it could have a carryover effect. Precautions carried out in the repeated-measures design studies to eliminate this carryover effect included filling the created femoral tunnels with epoxy [57] or cement [53] after completion of the first femoral tunnel positioning technique. As aperture placement in the other 3 studies included wire placement procedure only (i.e., no tunnel), they had no carryover effect.
Regarding sample size of knees analyzed in each group, generally the sample size was somewhat higher in TI group as it was presented by 2 subgroups (AM&OI) in the 7 multiarm studies. Also, nine double arm studies had unbalanced size in their 2 groups.
Regarding intervention integrity, qualitative within-studies comparison showed that the surgeon's experience level was comparable between both groups. However, that comparability was uncertain in 3 studies [13, 30, 60] and in all studies with non-contemporary groups when the surgeon changed his technique from TT to TI femoral drilling (13 studies). Regarding surgical technique, in one study [62], there was a major performance bias of utilizing surgical navigation system for femoral aperture localization in TI group only. Also, in 4 studies [23, 39, 63, 64], anterior notchplasty was performed in TT group only.
Effects of interventions (qualitative synthesis and meta-analysis)
Comparison of femoral aperture placement between TI and TT technique was approached either directly by comparing the ability of each technique to create the anatomic footprint position or indirectly by comparing the quantified aperture location placed by each technique. Both aperture and footprint positions were defined in the coronal and sagittal planes. Coronal plane position was assessed along the anteroposterior (AP) anatomical axis, along the line perpendicular to the Blumensaat’s line (BL), and along mediolateral direction. Sagittal plane position was assessed along the PD anatomical axis and along BL (Fig. 2).
Schematic diagram of profile view of medial wall of lateral femoral condyle. LICR; lateral intercondylar ridge. Blue lines: Anatomical coordinates; PD (proximal-distal) and AP (antero-posterior) axes. Red lines: Blumensaat's line coordinates; BL (Blumensaat's line) or DS axis (deep-to-shallow axis) and perpendicular to BL or HL (high-to-low axis)
In addition, comparison of tibial aperture position between both techniques was performed whenever reported in included studies.
Direct approach of comparing the ability of each technique to create the anatomic footprint position
-
A.
Footprint coronal plane position
-
1.
Along AP anatomical axis
Assessment of the distance of aperture center placed by each technique to the footprint center of the same knee on digitized 3d model in 2 studies (48 specimens) [53, 58] showed that TI technique placed aperture at less anterior distance from footprint than TT technique with a small mean difference of 3.3 mm (Additional file 5 and Fig. 3A). Also, while TT technique placed F aperture anterior to the footprint, albeit at small distance of 1.9 mm, TI technique placed it accurately at footprint center of same knee directly on 10 specimens (one study) [52]. Contradictory to the pervious findings, there was nonsignificant difference between both techniques in recreating the AP footprint position of the contralateral knee in 2 studies (46 participants) [12, 18] using MRI (Additional file 5 and Fig. 3B). Also, the difference in AP position%, measured by the anatomic coordinate axis (ACA) method, between aperture and footprint of contralateral knee, assessed on MRI, was nonsignificant between both techniques in one study (20 patients) [17].
Visual display of the distance of aperture center to footprint center in postero-anterior and proximal-distal axes measured on digitized 3D model of same knee (A) and on MRI of contralateral knee (B). Each figure includes 2 dotted circles (transtibial) and 2 solid circles (independent technique) representing apertures placed in 2 studies that assessed the displayed outcome
-
2.
Perpendicular to BL
In one study (20 specimens) [64], assessment of aperture spatial position in footprint referenced to BL on CT showed that TI technique placed a little bit more apertures in the lower deep quadrant of same knee footprint than TT technique. In another study [62]analyzing 20 specimens directly, TI technique placed significantly more apertures in the lower thirds of same knee footprint than TT. However, this study had a major performance bias of utilizing surgical navigation system for femoral aperture localization in TI group only.
-
B.
Footprint sagittal plane position along PD anatomical axis
There was nonsignificant difference between both techniques in recreating the PD footprint position of the same knee assessed on digitized 3D model in two studies (48 specimens) [53, 58] (Additional file 5 and Fig. 3A). Consistent finding was demonstrated in 2 studies (46 participants) [18, 69] comparing aperture placed by each technique to the contralateral knee footprint on MRI (Additional file 5 and Fig. 3B). Contradictory to the previous findings, while TT technique placed F aperture proximal to the footprint, TI technique placed it accurately at footprint center of same knee directly assessed on 10 specimens (one study) [52]. Consistent finding was demonstrated in one study (20 participants) [17] assessing the difference in PD position, measured by ACA method, between aperture and footprint of the contralateral knee as measured on MRI.
-
III.
Footprint absolute position
Directly comparing the distance of aperture center placed by each technique to footprint center of the same knee on digitized 3d model showed nonsignificant difference in 2 studies (48 specimens) [53, 58] (Additional file 5 and Fig. 3A). In 3 studies (87 patients) [12, 18, 26] assessing the ability of each technique to recreate the footprint position of the contralateral knee on MRI, there was nonsignificant difference in the distance of aperture center to footprint center (Additional file 5). Contradictory to the pervious findings, aperture placed by TI technique was significantly closer, albeit by small mean difference of 2.4 mm and 4 mm, in two studies (59 specimens) [61, 64] using CT scan. Assessing the ability of each technique to place the aperture center within the margins of footprint of same knee on photographed arthroscopic image in one study (20 specimens) [54], TI technique placed F aperture center at significantly closer distance to the closest point of footprint, albeit with a small mean difference of 3.4 mm. However, the tibial tunnel starting point in TT technique of this study was conventional point of Morgan [70]. For more detailed data, see summary of findings table of direct methods (Table 1).
Indirect approach of comparing the quantified aperture location placed by TT and TI techniques
The aperture location was quantified either as percentage ratio of overall scaling dimension from the distal femur or as distance in millimeters (mm) from a fixed anatomic landmark.
-
A.
Coronal plane position
-
1.
Perpendicular to BL as percentage ratio of an overall scaling dimension from the lateral femoral condyle (LFC) or the intercondylar notch
In 16 studies (1070 patients), TI technique significantly lowered the position of the placed aperture than TT technique as measured by the quadrant method [71] on 3D CT (Figs. 4A, 5) [21, 22, 34, 41, 42]. A consistent finding was demonstrated in 2 studies (102 patients) [45, 56] as measured by quadrant method on radiography (Additional file 6) and in one study (105 participants) [19] as measured by method proposed by Heming [72] on tunnel AP radiograph. Also, on the same projection of distal femur (tunnel radiograph), Mirzatolooei [35] demonstrated a consistent finding using Sommer's method [73]
Meta-analysis of aperture coronal plane position. A Perpendicular to BL measured on 3DCT by quadrant method (Higher percentage is defined as lower aperture location). B Along AP axis measured on 3DCT by anatomic coordinate axis method (Higher percentage is defined as more posterior aperture location). C Along AP axis measured on axial MRI by clock face method (Higher degrees is defined as more anterior aperture position). (c + m): combined conventional and modified TT groups. (AM + OI): combined AM and OI groups
Femoral apertures placed by each technique [transtibial (A) and independent (B)] quantified by quadrant method on 3D CT reconstructed profile view of medial wall of lateral femoral condyle. The area in the black square frame contains 16 small points representing the centers of femoral apertures placed in 16 studies and synthesized in forest plots presented in Figs. 4A and 7A. This is magnified in C and D, respectively. h: line perpendicular to the Blumensaat’s line, t: line parallel to the Blumensaat’s line
-
2.
Along AP anatomical axis
-
I.
As percentage ratio of an overall scaling dimension from LFC or intercondylar notch
In 4 studies (361 patients), TI technique placed femoral aperture in significantly more posterior position than TT technique as measured by ACA method [74] on 3D CT (Figs. 4B, 6) [29, 33, 40]. A consistent finding was demonstrated in 3 studies (126 participants) as measured by clock face method [75] on axial MRI (Fig. 4C) [25, 43, 47]. Also, in one study (20 specimens) [59], TI technique significantly placed femoral aperture significantly more posterior than TT technique as measured by method proposed by Heming on axial CT view. However, it may worth a little, to report that one study (20 specimens) [51] demonstrated that there is nonsignificant difference in aperture position along AP anatomical axis as measured by clock face method directly on specimens. However, this study is used an anterior target point at 11 o'clock position.
Femoral aperture placed by each technique [transtibial (A) and independent (B)] quantified by anatomic coordinate axis method on 3D CT reconstructed profile view of medial wall of lateral femoral condyle. Each figure includes 4 small points representing the centers of femoral apertures placed in 4 studies and synthesized in forest plots presented in Figs. 4B and 7B
-
II.
As distance in mm from a fixed anatomic landmark
A radiological study [36] using MRI performed on 61 participants demonstrated that the posterior margin of aperture placed by TI technique was significantly at more posterior distance from the over-the-top point (OTT) than TT technique. A consistent result was demonstrated on 20 specimens (one study) [60] where TI technique placed aperture center significantly closer to the inferior articular surface (IAS) than TT technique as measured on profile 3D CT view of medial wall of LFC. Contradictory to these findings, there was nonsignificant difference between both techniques in the distance of aperture to anterior notch tip as measured directly on 10 specimens (one study) [55]. Also, qualitative synthesis showed inconsistent results of 2 studies (40 specimens) assessing the distance of aperture inferior edge to inferior articular surface (IAS) on profile 3D CT view of medial wall of LFC. While one of them [63] showed nonsignificant difference between both techniques, the other [59] showed that TI technique placed aperture at significantly closer distance than TT technique.
-
B.
Sagittal plane position
-
1.
Along BL as percentage ratio of an overall scaling dimension from LFC or intercondylar notch
In 16 studies (1070 patients), there was nonsignificant difference between both techniques in the position of placed aperture along BL as measured by quadrant method [71] on 3D CT (Figs. 5, 7A) [21, 22, 34, 41, 42]. Using the same measurement method on radiography and MRI, a consistent result was demonstrated on 102 patients (2 studies) [45, 56] and 87 patients (2 studies) [25, 76], respectively (Additional file 6). Also, qualitative synthesis of results of 2 studies (80 patients) [13, 56] showed nonsignificant difference between both techniques in the position of anterior margin of placed aperture along BL as measured by Aglietti method [77] on radiography. Contradictory to the previous findings, TI technique placed femoral aperture at a significantly shallower position than the TT technique as measured by Harner method [77] on radiography in 2 studies (92 participants) [28, 46] (Additional file 6). A consistent finding was demonstrated in one study (30 patients) [20], where the placed femoral aperture screw head of TI technique was at a significantly shallower position than that of the TT technique as measured by the quadrant method on radiography. Also, in one study (12 specimens) [65], TI technique placed femoral aperture anterior margin at a significantly shallower position than the TT technique as measured by Aglietti method [77] directly on specimen.
Meta-analysis of aperture sagittal plane position. A Along BL measured on 3DCT by quadrant method (Higher percentage is defined as shallower aperture position). B Along DP axis measured on 3DCT by anatomic coordinate axis method (Higher percentage is defined as more distal aperture position). (c + m): combined conventional and modified TT groups. (AM + OI): combined AM and OI groups
-
2.
Along PD anatomical axis
-
I.
As percentage ratio of an overall scaling dimension from LFC or intercondylar notch
In 3 studies (361 patients) [25, 43, 47] there was nonsignificant difference between both techniques in the PD position of placed aperture as measured by the ACA method [74] on 3D CT (Figs. 6, 7B) [29, 33, 40]. Contradictory to that, in one study (100 patients) [37], TI technique placed femoral aperture at a significantly more distal position than the TT technique as measured by clock face method on CT coronal view.
-
II.
As distance in mm from a fixed anatomic landmark
Nonsignificant difference was demonstrated in 3 studies, the first (20 specimens) [51] and second (20 specimens) [59] measured the distance of aperture posterior edge to posterior articular surface on specimen and on CT, respectively, and the third (61 participants) [36] measured the distance of aperture posterior edge to OTT point on MRI. Contradictory to that a significant difference between both techniques was demonstrated. The direction of that intervention effect was diverse among studies. In 2 studies (40 specimens) [54, 60], the aperture center placed by TI technique was closer to PAS than TT technique as measured on specimen and CT. Other 2 studies showed a more distal position of F aperture placed by TI technique with the first (10 specimens) [55] measuring the distance of aperture center to anterior notch tip and the second (20 specimens) [63] measuring distance of aperture anterior edge to anterior articular surface on profile 3D CT view of medial wall of LFC. For more detailed data, see summary of findings table of indirect methods (Table 2) [31].
Comparison of tibial aperture position between TT and TI techniques
-
A.
Tibial aperture anteroposterior (AP) position
In 13 studies (740 patients), TT technique placed tibial aperture in a significantly more posterior position than TI technique as measured on CT [MD: 2.64% more posterior (95% CI: 4.42–0.86%)] (Additional file 7). Also, in one study (30 patients) assessing the distance between tibial aperture center and footprint center in AP direction on MRI, TT technique placed tibial aperture at more posterior distance from footprint than TI technique with a mean difference of 6.5 mm [18]. In another study analyzing 20 specimens directly, TT technique placed significantly more apertures in the posterior third of same knee footprint than TI technique [62]. Contradictory to the pervious findings, there was nonsignificant difference between both techniques in the tibial aperture AP position measured on MRI and radiography in 4 studies (156 participants) and 2 studies (92 participants), respectively (Additional file 7). Another study whose results could not be pooled measured the tibial aperture anterior margin AP position on radiography and demonstrated a consistent result [13]. In addition, the difference in AP position%, measured on MRI, between tibial aperture and footprint of contralateral knee was nonsignificant between both techniques in one study (20 patients) [17].
-
B.
Tibial aperture mediolateral (ML) position
There was nonsignificant difference between both techniques in the tibial aperture ML position measured on CT in 11 studies (703 participants) (Additional file 7). Using the same measurement method on radiography and MRI, a consistent result was demonstrated on 32 patients (one study) [46]; and 48 patients (one study) [25], respectively. In addition, there was nonsignificant difference between both techniques in recreating the ML footprint position of the contralateral knee in one study (30 participants) using MRI [18]. Also, the difference in ML position% measured on MRI between tibial aperture and footprint of contralateral knee was nonsignificant between both techniques in one study (20 patients) [17]. However, it may worth a little, to report that in one study (60 participants) TT technique placed tibial aperture in significantly more medial position than TI technique as measured on radiography [28].
Subgroup analyses
While the type of TI technique (AM or OI) had nonsignificant effect on the intervention effect on aperture position perpendicular to BL measured on CT, the presence or absence of modifications in TT technique had significant effect on intervention effect on the same outcome. (Details are presented in Additional file 8). Because the data in the analyzed subgroups should be independent, both Osti et al. and Tofra et al. studies were excluded from the first and second subgroup analyses, respectively. Each of them has intervention group that will contribute to both analyzed subgroups. However, these excluded three-arm studies also emphasize the results of subgroup analyses. Osti et al. study demonstrated nonsignificant difference between AM and OI techniques in the height of placed aperture perpendicular to BL measured on CT. Torfa et al. study demonstrated that mTT technique significantly lowered the position of placed aperture than conventional TT technique.
Sensitivity analysis
The intervention effect on aperture position perpendicular to BL measured on 3D CT differed a lot between the primary analysis (i.e., including all studies) and the sensitivity analysis in which we excluded observational studies. (Details are presented in Additional file 9).
Discussion
The key findings of the present study indicated that there was nonsignificant difference between TI and TT techniques in the distance from femoral aperture center to footprint center. If there was a difference (in the minority of included studies), it was that the TI technique might place aperture center closer to footprint center than TT technique but with a small mean difference. Moreover, both techniques were unable to accurately recreate the anatomic footprint position. This could be explained by the inability to visualize the footprint in two thirds of included studies and the utilization of the general “rules of thumb” to provide an approximate location for aperture placement which are not applicable to all individuals. Findings also indicated the following.
Regarding aperture placement in the coronal plane, there might be a difference between both techniques in the ability to achieve footprint position along AP anatomical axis which was that TI technique might place the femoral aperture center at less anterior distance from same knee footprint center with a small mean difference. Also, TI technique placed aperture at significantly more posterior position than TT technique. In the direction perpendicular to BL, TI technique significantly lowered the position of the placed aperture than TT technique.
Regarding aperture placement in the sagittal plane, there was nonsignificant difference between both techniques in the ability to achieve footprint position along PD anatomical axis. If there was a difference, it was that the TI might place aperture center at less proximal distance from footprint center than TT technique with moderate mean difference. Also, there was nonsignificant difference between both techniques in the position of aperture placed along both BL and PD anatomical axis. If there was a difference, there was inconsistency in the direction of the intervention effect.
Regarding the effect of each technique on the tibial aperture position, there might be a difference between both techniques in tibial aperture AP position which was that TT technique might place the tibial aperture at more posterior position than TI technique. However, in 13 studies assessing tibial aperture AP position on CT, the difference looked clinically insignificant as both the point of estimate of the intervention effect (2.64%) measured on CT in 13 studies and its 95% confidence interval (4.42–0.86%) were less than the reported average anatomical range of tibial footprint center AP position (7%) [78].
Relevance of our findings to the recent ACL direct/indirect insertion concept: The central axis of ACL direct insertion (= parallel to intercondylar ridge (ICR)) is inclined 70° and 30° with the BL and PD anatomical axis, respectively [1, 66] (Fig. 2). This could explain why the outcomes assessing aperture position along and perpendicular to BL, contradictory to those assessing it along AP and PD anatomical axes, could directly answer the question of the ability of each technique to properly position the aperture according to the new concept of direct and indirect fibers of ACL femoral insertion. As the aperture to be performed is smaller and geometrically distinct from the area occupied by ACL femoral insertion, researchers advised recently to place aperture eccentrically in the footprint where the structurally and functionally important direct fibers lie [1]. Putting altogether, we could suggest that the more anterior and distal placement along AP and PD anatomical axes would be more advantageous, not the reverse. Also, the differential in aperture placement along the perpendicular to BL, which is nearly parallel to ICR, may not be so crucial if the aperture is placed closely behind the ICR. However, the shallower placement along BL would be highly more advantageous. Fortunately, sagittal plane aperture position, whether along PD or along BL, is adjustable by changing offset guide size even in TT technique.
Regarding participants included in our review, in cadaveric studies, the average age of specimens was 67.5 years which was older than the average young age of population undergoing ACL reconstruction. However, whenever reported, specimens with degenerative changes were excluded. In clinical studies, the average age was 28.5 years which is the average age group undergoing ACL reconstruction. Regarding intervention integrity, the greatest single variable in a surgical comparison study is the surgeon, while same surgeon performing the procedures reduces operative variability; the difference in surgeons with variant experience level in our studies could make our findings generalizable to all surgeon groups.
Our review analyzed femoral aperture placement in TT technique with all its suggested modifications and the TI technique whether AM or OI. In addition, our review analyzed the effect of each technique on tibial aperture position which could also affect the ACL graft obliquity. Our review included 55 studies involving a total of 2401 knees and analyzing femoral aperture placement using both approaches of indirectly comparing the quantified aperture placed by each technique and directly comparing the ability of each technique to create the anatomic footprint position.
There was substantial heterogeneity in the intervention effect on aperture position along and perpendicular to BL on CT scan, this could be explained first by the statistically demonstrated effect of mTT technique (see subgroup analysis) which could also explain the inconsistency in the results of Larson et al. [59] and Tompkin et al. [63] studies where Larson et showed a significantly lower aperture placement by TI technique and Tompkin et al. showed nonsignificant difference between both techniques. Second, the included studies utilized different targets for femoral aperture placement which varied according to the chronological evolution of the appropriate femoral aperture position and the in-between studies variability. However, this variation was only inter-study variation not intra-study variation. Our review included studies from the nineties of the twentieth century when the target for aperture placement was at a point as close as possible to the over-the-top point [55], or just deep to AM bundle site [56], or at 11 O’clock position [13]. Then, there were studies from the first decade and the early second decade of the twenty-first century when aperture placement aimed at high deep part of footprint to mimic the AM bundle [16, 36, 40, 51, 54]. However, most of our studies used a target point at footprint center or its surrogate by other localization strategies. Third, regarding femoral aperture localization strategies, we found that, whenever reported, they varied in different studies. They included mainly clock face method, footprint remnants, and fixed anatomic landmarks. The clock face method [75] is confusing as reported by some surgeons. Neither the knee flexion angle in which the clock face was applied, nor the transverse reference axis of the clock face were specified in our studies, especially that there are different methods for clock face referencing in the literature [72, 79]. The footprint remnants method could be ineffective with the increase in time between injury and surgery which varied in our studies. The utilized anatomic landmarks varied in our studies. Localization strategies also included intraoperative assistance by fluoroscopy and navigation system in two [14, 37] and one studies [62], respectively. Lastly, the potentially different surgical technique, utilized among the included studies, may explain the high heterogeneity in the intervention effect on aperture position along and perpendicular to BL. First, the AM portal technique varied in our studies. Drilling the femoral tunnel through an accessory AM portal, while viewing through standard AM one, might allow better visualization and proper localization of femoral aperture at the best desired position. Second, the performance of notchplasty varied in our studies (performed in 9 studies). Technically, the TT technique requires an accurate notchplasty to visualize the femoral footprint. In contrast when performing AM portal reconstruction, the AM portal allows visualization of footprint without the need for notchplasty (97). Third, tibia tunnel intraarticular target point varied in our studies. Tibial tunnel aiming anteriorly at tibial footprint would direct the guide to a significantly shallower femoral aperture position. Fourth, tibial tunnel diameter varied in our studies. In the TT technique, increasing tibial tunnel diameter allows more maneuverability of the guide and adjusting femoral aperture to the best desired position [68]. Lastly, posterior wall thickness, permitted by offset guide, varied in our studies. This might lead to variability in the sagittal position of placed femoral aperture. This could also explain the inconsistency in the direction of intervention effect on aperture sagittal plane position between Gavriliidis et al. [54] and Miller et al. [60] studies on one side and Grondvedt et al. [55] and Tompkins et al. [63] studies on the other side. While the first 2 studies found that TI technique placed aperture more proximal than TT technique, the other two found that TI technique placed aperture more distal than TT technique. The size of utilized offset guide differed in these studies (6 mm and 7 mm in the first and second two studies, respectively).
There are some limitations in our review. Due to our thoughts that the anatomical positioning of femoral aperture is an anatomical outcome that could not be confounded too much by independent intraoperative and post-operative variables, we included RCTs and observational studies in our review. However, we assessed that decision by performing sensitivity analysis on aperture position perpendicular to BL measured on CT. In this sensitivity analysis, the intervention effect changed a lot. So, our results in that outcome (especially the intervention effect size) should be interpreted cautiously. In addition, as explained previously, alteration of tibial tunnel starting point was not included in defining mTT technique in our review. This surgical factor might influence aperture placement in our studies. For instance, the better placement of aperture center in Gadikota et al. [53] study more than Kaseta et al. [58] (1.5 mm versus 4.5 mm both anterior and proximal distance to same knee footprint center) could be explained by difference in tibial tunnel starting point which was Piasecki’s modified point [68] in Gadikota et al. study and Morgan conventional point [70] in Kaseta et al. study.
Two previous reviews compared femoral aperture location following TT and TI techniques. The first one [8] included 6 observational studies. Authors demonstrated a similar finding to ours; that TI technique placed femoral aperture in a lower position than TT technique. However, they compared the quantified femoral aperture location of each technique using the quadrant method and ACA method on 3D CT without taking into consideration the difference in axis direction between BL and anatomical coordinates. This drawback could explain the demonstrated inconsistency in the intervention effect on femoral aperture deep-to-shallow position between measurement using quadrant and ACA methods. Also, the review did not directly answer the question of how each technique was able to recreate the anatomic footprint. Moreover, the authors took an improper statistical approach of including all groups of three-arm studies in the meta-analysis resulting in counting the control group twice in the pooling analysis, giving those individuals twice their weight. The second one [9], included both observational studies and RCTs. Although the authors demonstrated that the TI technique placed femoral aperture significantly closer to the footprint center than the TT technique, the difference was small of 2.69 mm. Also, the authors pooled studies assessing femoral aperture position on different imaging modality or its surrogate. This is obviously an inaccurate approach as these modalities have different diagnostic accuracy. Moreover, they took the same improper statistical approach of including all groups of three-arm studies in the meta-analysis.
Conclusion
Implication for practice
This systematic review and meta-analysis of clinical and cadaveric studies demonstrated that both techniques were unable to accurately recreate the anatomic femoral footprint position. To recreate the anatomic footprint position, surgeons may consider the patient-specific locations of footprint. It also demonstrated that while the difference between both techniques was nonsignificant in aperture placement in the sagittal plane, it was significant in the coronal plane. This coronal plane placement could be either along the perpendicular to BL or along the AP anatomical axis. Along the perpendicular to BL, this statistically significant difference could be overcome by modifications to TT technique and may be non-crucial according to the recent concept of functional ACL reconstruction. Along the AP anatomical axis, the demonstrated direction of intervention effect, which was more posterior placement of femoral aperture by TI technique, could be, to some extent, in favor of the TT technique according to recent concept of functional ACL reconstruction. In addition, the review demonstrated that TT technique might place the tibial aperture at more posterior position than TI technique and the difference looked clinically insignificant.
Implication for research
We advise conducting comparative studies using accurate and similar localization strategies for femoral aperture placement. Also, we advise the introduction of new assessment tools that reference the femoral aperture position to the axis of direct fibers insertion and the use of these tools in new studies comparing the ability of each technique to properly place femoral aperture.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jorge PB, Escudeiro D, Severino NR, Santili C, de Paula LeiteCury R, Junior AD, Guglielmetti LGB,. Positioning of the femoral tunnel in anterior cruciate ligament reconstruction: functional anatomical reconstruction. BMJ Open Sport Exerc Med. 2018;4(1):e000420. https://doi.org/10.1136/bmjsem-2018-000420.
Lopez-Vidriero E, Hugh Johnson D. Evolving concepts in tunnel placement. Sports Med Arthrosc Rev. 2009;17(4):210–6. https://doi.org/10.1097/JSA.0b013e3181bf6668.
de Paula LeiteCury R, Simabukuro AM, de Marques Oliveira V, Escudeiro D, Jorge PB, Severino FR, Guglielmetti LGB,. Anteromedial positioning of the femoral tunnel in anterior cruciate ligament reconstruction is the best option to avoid revision: a single surgeon registry. J Exp Orthop. 2020;7(1):11. https://doi.org/10.1186/s40634-020-00225-x.
Raffo CS, Pizzarello P, Richmond JC, Pathare N. A reproducible landmark for the tibial tunnel origin in anterior cruciate ligament reconstruction: avoiding a vertical graft in the coronal plane. Arthroscopy. 2008;24(7):843–5. https://doi.org/10.1016/j.arthro.2007.12.005.
Zhang C, Xu H, Li X, Wang Y, Zhang Q, Zhu Q. Oblique femoral tunnel or oblique graft? A modified anteromedial portal technique to obtain vertical femoral tunnel and oblique graft in anatomic anterior cruciate ligament reconstruction. Eur J Orthop Surg Traumatol. 2013;23(6):731–5. https://doi.org/10.1007/s00590-012-1046-4.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. https://doi.org/10.1186/2046-4053-4-1.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6. https://doi.org/10.1046/j.1445-2197.2003.02748.x.
Lee DH, Kim HJ, Ahn HS, Bin SI. Comparison of femur tunnel aperture location in patients undergoing transtibial and anatomical single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3713–21. https://doi.org/10.1007/s00167-015-3657-x.
Riboh JC, Hasselblad V, Godin JA, Mather RC. Transtibial versus independent drilling techniques for anterior cruciate ligament reconstruction a systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2013;41(11):2693–702. https://doi.org/10.1177/0363546513506979.
Nct. Femoral tunnel position on conventional MRI after anterior cruciate ligament reconstruction-transtibial technique versus transportal technique. https://clinicaltrialsgov/show/NCT01513434 (2012)
N. Comparison of 3 techniques for recreation of anterior cruciate ligament anatomic footprint. https://clinicaltrialsgov/show/NCT01513434 (2016)
Abebe ES, Moorman CT 3rd, Dziedzic TS, Spritzer CE, Cothran RL, Taylor DC, Garrett WE Jr, DeFrate LE. Femoral tunnel placement during anterior cruciate ligament reconstruction: an in vivo imaging analysis comparing transtibial and 2-incision tibial tunnel-independent techniques. Am J Sports Med. 2009;37(10):1904–11. https://doi.org/10.1177/0363546509340768.
Aglietti P, Zaccherotti G, Menchetti PP, De Biase P. A comparison of clinical and radiological parameters with two arthroscopic techniques for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1995;3(1):2–8. https://doi.org/10.1007/BF01553517.
Han JK, Chun KC, Lee SI, Kim S, Chun CH. Comparison of modified transtibial and anteromedial portal techniques in anatomic single-bundle ACL reconstruction. Orthopedics. 2019;42(2):83–9. https://doi.org/10.3928/01477447-20190211-04.
Harner CD, Marks PH, Fu FH, Irrgang JJ, Silby MB, Mengato R. Anterior cruciate ligament reconstruction: endoscopic versus two-incision technique. Arthroscopy. 1994;10(5):502–12. https://doi.org/10.1016/s0749-8063(05)80004-0.
Ahn JH, Jeong HJ, Ko CS, Ko TS, Kim JH. Three-dimensional reconstruction computed tomography evaluation of tunnel location during single-bundle anterior cruciate ligament reconstruction: a comparison of transtibial and 2-incision tibial tunnel-independent techniques. Clin Orthop Surg. 2013;5(1):26–35. https://doi.org/10.4055/cios.2013.5.1.26.
Arno S, Bell CP, Alaia MJ, Singh BC, Jazrawi LM, Walker PS, Bansal A, Garofolo G, Sherman OH. Does anteromedial portal drilling improve footprint placement in anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2016;474(7):1679–89. https://doi.org/10.1007/s11999-016-4847-7.
Bowers AL, Bedi A, Lipman JD, Potter HG, Rodeo SA, Pearle AD, Warren RF, Altchek DW. Comparison of anterior cruciate ligament tunnel position and graft obliquity with transtibial and anteromedial portal femoral tunnel reaming techniques using high-resolution magnetic resonance imaging. Arthroscopy. 2011;27(11):1511–22. https://doi.org/10.1016/j.arthro.2011.07.007.
Chang CB, Choi JY, Koh IJ, Lee KJ, Lee KH, Kim TK. Comparisons of femoral tunnel position and length in anterior cruciate ligament reconstruction: modified transtibial versus anteromedial portal techniques. Arthroscopy. 2011;27(10):1389–94. https://doi.org/10.1016/j.arthro.2011.06.013.
Cho Y, Cho J, Kim D. Normal sagittal of the anterior cruciate ligament can be reproduced using accessory anteromedial portal technique: a magnetic resonance imaging study. Arch Orthop Trauma Surg. 2012;132(7):1011–9. https://doi.org/10.1007/s00402-012-1498-3.
Clockaerts S, Van Haver A, Verhaegen J, Vuylsteke K, Leenders T, Lagae KC, Verdonk P. Transportal femoral drilling creates more horizontal ACL graft orientation compared to transtibial drilling: A 3D CT imaging study. Knee. 2016;23(3):412–9. https://doi.org/10.1016/j.knee.2016.02.014.
de Abreu-e-Silva GM, Baumfeld DS, Bueno EL, Pfeilsticker RM, de Andrade MA, Nunes TA. Clinical and three-dimensional computed tomographic comparison between ACL transportal versus ACL transtibial single-bundle reconstructions with hamstrings. Knee. 2014;21(6):1203–9. https://doi.org/10.1016/j.knee.2014.05.004.
Franceschi F, Papalia R, Rizzello G, Del Buono A, Maffulli N, Denaro V. Anteromedial portal versus transtibial drilling techniques in anterior cruciate ligament reconstruction: any clinical relevance? A retrospective comparative study. Arthrosc J Arthrosc Relat Surg. 2013;29(8):1330–7. https://doi.org/10.1016/j.arthro.2013.05.020.
Geng Y, Gai P. Comparison of 2 femoral tunnel drilling techniques in anterior cruciate ligament reconstruction. A prospective randomized comparative study. BMC Musculoskelet Disord. 2018;19(1):454. https://doi.org/10.1186/s12891-018-2376-0.
Guler O, Mahirogullari M, Mutlu S, Cerci MH, Seker A, Cakmak S. Graft position in arthroscopic anterior cruciate ligament reconstruction: anteromedial versus transtibial technique. Arch Orthop Trauma Surg. 2016;136(11):1571–80. https://doi.org/10.1007/s00402-016-2532-7.
Hart A, Sivakumaran T, Burman M, Powell T, Martineau PA. A prospective evaluation of femoral tunnel placement for anatomic anterior cruciate ligament reconstruction using 3-dimensional magnetic resonance imaging. Am J Sports Med. 2018;46(1):192–9. https://doi.org/10.1177/0363546517730577.
Hensler D, Working ZM, Illingworth KD, Tashman S, Fu FH. Correlation between femoral tunnel length and tunnel position in ACL reconstruction. J Bone Joint Surg Am. 2013;95(22):2029–34. https://doi.org/10.2106/jbjs.l.01315.
Hussin EA, Aldaheri A, Alharbi H, Farouk HA. Modified transtibial versus anteromedial portal techniques for anterior cruciate ligament reconstruction, a comparative study. Open Access J Sports Med. 2018;9:199–213. https://doi.org/10.2147/oajsm.s157729.
Illingworth KD, Hensler D, Working ZM, Macalena JA, Tashman S, Fu FH. A simple evaluation of anterior cruciate ligament femoral tunnel position: the inclination angle and femoral tunnel angle. Am J Sports Med. 2011;39(12):2611–8. https://doi.org/10.1177/0363546511420128.
Inderhaug E, Larsen A, Strand T, Waaler PA, Solheim E. The effect of feedback from post-operative 3D CT on placement of femoral tunnels in single-bundle anatomic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):154–60. https://doi.org/10.1007/s00167-014-3355-0.
Jaecker V, Zapf T, Naendrup JH, Pfeiffer T, Kanakamedala AC, Wafaisade A, Shafizadeh S. High non-anatomic tunnel position rates in ACL reconstruction failure using both transtibial and anteromedial tunnel drilling techniques. Arch Orthop Trauma Surg. 2017;137(9):1293–9. https://doi.org/10.1007/s00402-017-2738-3.
Lee DW, Kim JG, Lee JH, Park JH, Kim DH. Comparison of modified transtibial and outside-in techniques in anatomic single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(10):2857–70. https://doi.org/10.1016/j.arthro.2018.05.041.
Lee JK, Lee S, Seong SC, Lee MC. Anatomic single-bundle ACL reconstruction is possible with use of the modified transtibial technique: a comparison with the anteromedial transportal technique. J Bone Joint Surg Am. 2014;96(8):664–72. https://doi.org/10.2106/jbjs.m.00088.
Matassi F, Sirleo L, Carulli C, Innocenti M. Anatomical anterior cruciate ligament reconstruction: transtibial versus outside-in technique: SIGASCOT Best Paper Award Finalist 2014. Joints. 2015;3(1):6–14.
Mirzatolooei F. Comparison of short term clinical outcomes between transtibial and transportal TransFix(R) femoral fixation in hamstring ACL reconstruction. Acta Orthop Traumatol Turc. 2012;46(5):361–6. https://doi.org/10.3944/aott.2012.2679.
Noh JH, Roh YH, Yang BG, Yi SR, Lee SY. Femoral tunnel position on conventional magnetic resonance imaging after anterior cruciate ligament reconstruction in young men: transtibial technique versus anteromedial portal technique. Arthroscopy. 2013;29(5):882–90. https://doi.org/10.1016/j.arthro.2013.01.025.
Osti M, Krawinkel A, Ostermann M, Hoffelner T, Benedetto KP. Femoral and tibial graft tunnel parameters after transtibial, anteromedial portal, and outside-in single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(9):2250–8. https://doi.org/10.1177/0363546515590221.
Pascual-Garrido C, Swanson BL, Swanson KE. Transtibial versus low anteromedial portal drilling for anterior cruciate ligament reconstruction: a radiographic study of femoral tunnel position. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):846–50. https://doi.org/10.1007/s00167-012-1988-4.
Seo SS, Kim CW, Kim JG, Jin SY. Clinical results comparing transtibial technique and outside in technique in single bundle anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013;25(3):133–40. https://doi.org/10.5792/ksrr.2013.25.3.133.
Shin YS, Ro KH, Lee JH, Lee DH. Location of the femoral tunnel aperture in single-bundle anterior cruciate ligament reconstruction: comparison of the transtibial, anteromedial portal, and outside-in techniques. Am J Sports Med. 2013;41(11):2533–9. https://doi.org/10.1177/0363546513500764.
Silva A, Sampaio R, Pinto E. ACL reconstruction: comparison between transtibial and anteromedial portal techniques. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):896–903. https://doi.org/10.1007/s00167-011-1645-3.
Song EK, Kim SK, Lim HA, Seon JK. Comparisons of tunnel-graft angle and tunnel length and position between transtibial and transportal techniques in anterior cruciate ligament reconstruction. Int Orthop. 2014;38(11):2357–62. https://doi.org/10.1007/s00264-014-2457-0.
Tasdemir Z, Gulabi D, Saglam F, TokgozOzal S, Elmali N. Does the anteromedial portal provide clinical superiority compared to the transtibial portal in anterior cruciate ligament reconstruction in nonprofessional athletes in short-term follow-up? Acta Orthop Traumatol Turc. 2015;49(5):483–91. https://doi.org/10.3944/aott.2015.15.0016.
Venosa M, Delcogliano M, Padua R, Alviti F, Delcogliano A. Femoral tunnel positioning in anterior cruciate ligament reconstruction: anteromedial portal versus transtibial technique-a randomized clinical trial. Joints. 2017;5(1):34–8. https://doi.org/10.1055/s-0037-1601413.
Xu Y, Ao Y, Wang J, Yu J, Cui G. Relation of tunnel enlargement and tunnel placement after single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(7):923–32. https://doi.org/10.1016/j.arthro.2011.02.020.
Yanasse RH, Lima AA, Antoniassi RS, Ezzedin DA, Laraya MH, Mizobuchi RR. Transtibial technique versus two incisions in anterior cruciate ligament reconstruction: tunnel positioning, isometricity and functional evaluation. Rev Bras Ortop. 2016;51(3):274–81. https://doi.org/10.1016/j.rboe.2016.04.001.
Yau WP, Fok AW, Yee DK. Tunnel positions in transportal versus transtibial anterior cruciate ligament reconstruction: a case-control magnetic resonance imaging study. Arthroscopy. 2013;29(6):1047–52. https://doi.org/10.1016/j.arthro.2013.02.010.
Youm YS, Cho SD, Lee SH, Youn CH. Modified transtibial versus anteromedial portal technique in anatomic single-bundle anterior cruciate ligament reconstruction: comparison of femoral tunnel position and clinical results. Am J Sports Med. 2014;42(12):2941–7. https://doi.org/10.1177/0363546514551922.
Çiloğlu O, Çiçek H, Yılmaz A, Özalay M, Söker G, Leblebici B. Comparison of clinical and radiological parameters with two different surgical methods for anterior cruciate ligament reconstruction. J Knee Surg. 2020;33(9):938–46. https://doi.org/10.1055/s-0040-1710363.
Trofa DP, Saltzman BM, Corpus KT, Connor PM, Fleischli JE, Piasecki DP. A hybrid transtibial technique combines the advantages of anteromedial portal and transtibial approaches: a prospective randomized controlled trial. Am J Sports Med. 2020;48(13):3200–7. https://doi.org/10.1177/0363546520956645.
Albuquerque RF, Amatuzzi MM, Pacheco AP, Angelini FJ, Campos O Jr. Positioning of the femoral tunnel for arthroscopic reconstruction of the anterior cruciate ligament: comparative study of 2 techniques. Clinics (Sao Paulo). 2007;62(5):613–8. https://doi.org/10.1590/s1807-59322007000500013.
Bedi A, Musahl V, Steuber V, Kendoff D, Choi D, Allen AA, Pearle AD, Altchek DW. Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy. 2011;27(3):380–90. https://doi.org/10.1016/j.arthro.2010.07.018.
Gadikota HR, Sim JA, Hosseini A, Gill TJ, Li G. The relationship between femoral tunnels created by the transtibial, anteromedial portal, and outside-in techniques and the anterior cruciate ligament footprint. Am J Sports Med. 2012;40(4):882–8. https://doi.org/10.1177/0363546511434276.
Gavriilidis I, Motsis EK, Pakos EE, Georgoulis AD, Mitsionis G, Xenakis TA. Transtibial versus anteromedial portal of the femoral tunnel in ACL reconstruction: a cadaveric study. Knee. 2008;15(5):364–7. https://doi.org/10.1016/j.knee.2008.05.004.
Grontvedt T, Pena F, Engebretsen L. Accuracy of femoral tunnel placement and resulting graft force using one- or two-incision drill guides. A cadaver study on ten paired knees. Arthroscopy. 1996;12(2):187–92. https://doi.org/10.1016/s0749-8063(96)90009-2.
Giron F, Buzzi R, Aglietti P. Femoral tunnel position in anterior cruciate ligament reconstruction using three techniques. A cadaver study. Arthroscopy. 1999;15(7):750–6. https://doi.org/10.1016/s0749-8063(99)70007-1.
Jennings JK, Leas DP, Fleischli JE, D’Alessandro DF, Peindl RD, Piasecki DP. Transtibial versus anteromedial portal ACL reconstruction: is a hybrid approach the best? Orthop J Sports Med. 2017;5(8):2325967117719857. https://doi.org/10.1177/2325967117719857.
Kaseta MK, DeFrate LE, Charnock BL, Sullivan RT, Garrett WE Jr. Reconstruction technique affects femoral tunnel placement in ACL reconstruction. Clin Orthop Relat Res. 2008;466(6):1467–74. https://doi.org/10.1007/s11999-008-0238-z.
Larson AI, Bullock DP, Pevny T. Comparison of 4 femoral tunnel drilling techniques in anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg. 2012;28(7):972–9. https://doi.org/10.1016/j.arthro.2011.12.015.
Miller CD, Gerdeman AC, Hart JM, Bennett CG, Golish SR, Gaskin C, Miller MD. A comparison of 2 drilling techniques on the femoral tunnel for anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(3):372–9. https://doi.org/10.1016/j.arthro.2010.08.012.
Robert HE, Bouguennec N, Vogeli D, Berton E, Bowen M. Coverage of the anterior cruciate ligament femoral footprint using 3 different approaches in single-bundle reconstruction: a cadaveric study analyzed by 3-dimensional computed tomography. Am J Sports Med. 2013;41(10):2375–83. https://doi.org/10.1177/0363546513498989.
Steiner ME, Battaglia TC, Heming JF, Rand JD, Festa A, Baria M. Independent drilling outperforms conventional transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(10):1912–9. https://doi.org/10.1177/0363546509340407.
Tompkins M, Cosgrove CT, Milewski MD, Brockmeier SF, Hart JM, Miller MD. Anterior cruciate ligament reconstruction femoral tunnel characteristics using an accessory medial portal versus traditional transtibial drilling. Arthrosc J Arthrosc Relat Surg. 2013;29(3):550–5. https://doi.org/10.1016/j.arthro.2012.10.030.
Tompkins M, Milewski MD, Brockmeier SF, Gaskin CM, Hart JM, Miller MD. Anatomic femoral tunnel drilling in anterior cruciate ligament reconstruction: use of an accessory medial portal versus traditional transtibial drilling. Am J Sports Med. 2012;40(6):1313–21. https://doi.org/10.1177/0363546512443047.
Tudisco C, Bisicchia S. Drilling the femoral tunnel during ACL reconstruction: transtibial versus anteromedial portal techniques. Orthopedics. 2012;35(8):e1166-1172. https://doi.org/10.3928/01477447-20120725-14.
Wolf BR, Ramme AJ, Britton CL, Amendola A. Anterior cruciate ligament tunnel placement. J Knee Surg. 2014;27(4):309–17. https://doi.org/10.1055/s-0033-1364101.
Gougoulias N, Khanna A, Griffiths D, Maffulli N. ACL reconstruction: can the transtibial technique achieve optimal tunnel positioning? A radiographic study. Knee. 2008;15(6):486–90. https://doi.org/10.1016/j.knee.2008.07.006.
Piasecki DP, Bach BR Jr, Espinoza Orias AA, Verma NN. Anterior cruciate ligament reconstruction: can anatomic femoral placement be achieved with a transtibial technique? Am J Sports Med. 2011;39(6):1306–15. https://doi.org/10.1177/0363546510397170.
Abebe ES, Utturkar GM, Taylor DC, Spritzer CE, Kim JP, Moorman CT 3rd, Garrett WE, DeFrate LE. The effects of femoral graft placement on in vivo knee kinematics after anterior cruciate ligament reconstruction. J Biomech. 2011;44(5):924–9. https://doi.org/10.1016/j.jbiomech.2010.11.028.
Morgan CD, Kalman VR, Grawl DM. Definitive landmarks for reproducible tibial tunnel placement in anterior cruciate ligament reconstruction. Arthroscopy. 1995;11(3):275–88. https://doi.org/10.1016/0749-8063(95)90003-9.
Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL: Radiographic quadrant method. Am J Knee Surg. 1997;10(1):14–21 (discussion 21-12).
Heming JF, Rand J, Steiner ME. Anatomical limitations of transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(10):1708–15. https://doi.org/10.1177/0363546507304137.
Sommer CFNF, Müller W. Improperly placed anterior cruciate ligament grafts: correlation between radiological parameters and clinical results. Knee Surg Sports Traumatol Arthrosc. 2000;8:207–13.
Forsythe B, Kopf S, Wong AK, Martins CA, Anderst W, Tashman S, Fu FH. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am. 2010;92(6):1418–26. https://doi.org/10.2106/JBJS.I.00654.
Rue JPBM, Bach BR Jr. Hybrid single-bundle anterior cruciate ligament reconstruction technique using a transtibial drilled femoral tunnel. Tech Knee Surg. 2008;7(2):107–14. https://doi.org/10.1097/BTK.0B013E3181770793.
Youm YS, Cho SD, Eo J, Lee KJ, Jung KH, Cha JR. 3D CT analysis of femoral and tibial tunnel positions after modified transtibial single bundle ACL reconstruction with varus and internal rotation of the tibia. Knee. 2013;20(4):272–6. https://doi.org/10.1016/j.knee.2012.10.024.
Klos TV, Harman MK, Habets RJ, Devilee RJ, Banks SA. Locating femoral graft placement from lateral radiographs in anterior cruciate ligament reconstruction: a comparison of 3 methods of measuring radiographic images. Arthroscopy. 2000;16(5):499–504. https://doi.org/10.1053/jars.2000.4634.
Parkar AP, Adriaensen M, Vindfeld S, Solheim E. The anatomic centers of the femoral and tibial insertions of the anterior cruciate ligament: a systematic review of imaging and cadaveric studies reporting normal center locations. Am J Sports Med. 2017;45(9):2180–8. https://doi.org/10.1177/0363546516673984.
Mochizuki T, Muneta T, Nagase T, Shirasawa S, Akita KI, Sekiya I. Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(4):356–61. https://doi.org/10.1016/j.arthro.2005.09.020.
Acknowledgements
The authors would like to thank Prof. Amr A. Abdelrahman in Orthopedic Department, Ain Shams University, for his substantial contributions to conception and design of this review.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). No author or related institution has received any financial benefit from research in this review.
Author information
Authors and Affiliations
Contributions
HKH conceived of the review and performed the statistical analysis. Rest of authors participated in the design and coordination of the review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Search strategy.
Additional file 2
. Characteristics of included studies table.
Additional file 3
. Studies with modifications in TT technique.
Additional file 4
. Femoral aperture localization strategy utilized in TT and TI technique in included studies.
Additional file 5
. Metanalyses of direct outcomes.
Additional file 6
. Metanalyses of indirect outcomes.
Additional file 7
. Metanalyses of tibial aperture position.
Additional file 8
. Subgroup analyses by variation in TI techniques {AM vs OI} (Fig. A) and by modifications to TT technique {conventional TT vs modified TT (mTT)} (Fig. B).
Additional file 9
. Sensitivity analysis excluding low quality-design studies (observational studies).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Haroun, H.K., Abouelsoud, M.M., Allam, M.R. et al. Transtibial versus independent femoral tunnel drilling techniques for anterior cruciate ligament reconstruction: evaluation of femoral aperture positioning. J Orthop Surg Res 17, 166 (2022). https://doi.org/10.1186/s13018-022-03040-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03040-5